Variations in the anastomotic morphology of the deep plantar arterial arch, including vascularization principally from the medial plantar artery, should be considered when performing reconstructive foot procedures to ensure optimal flap and wound healing.
Dr. Bryan G. Beutel, Kansas City University College of Medicine, Department of Pathology and Anatomical Sciences, 1750 Independence Avenue, Kansas City, Missouri, 64106, USA. E-mail: BryanBeutel@gmail.com
Introduction: Forefoot structures are vascularized through the deep plantar arch, an anastomotic network classically described between the deep branch of the lateral plantar artery (dLPA) and the deep plantar artery (DPA). While it supplies the medial aspect of the plantar foot, the medial plantar artery (MPA) is not described as providing a vascular contribution to the deep plantar arterial arch.
Case Report: During routine cadaveric dissection of bilateral lower extremities in a 96-year-old Caucasian male, a unique anomaly was noted within the deep plantar arterial arch. The superficial branch of the medial plantar artery (sMPA) was found to course laterally at the level of the first metatarsophalangeal joint and anastomose with the DPA to form the deep plantar arch. No contribution was noted from the LPA. A total of 89 feet from 49 cadavers were subsequently examined, and no other donors exhibited this distinct morphology, resulting in an estimated prevalence of 2.3% of feet.
Conclusion: This case study describes a novel bilateral plantar vascular anomaly and reviews the potential clinical significance of this variant, which should be considered during various reconstructive flap procedures of the foot.
Keywords: Deep plantar arch, medial plantar artery, deep plantar artery, foot reconstruction, variant.
The deep plantar arch is the dominant arterial supply to the plantar surface of the foot, formed through an anastomosis between the deep branch of the lateral plantar artery (LPA) and deep plantar artery (DPA). Classically, the posterior tibial artery (PTA) bifurcates as the LPA and medial plantar artery (MPA) distal to the medial malleolus [1,2]. The LPA then courses laterally between the quadratus plantae and flexor digitorum brevis muscles before splitting into two terminal branches near the base of the fifth metatarsal: the superficial (sLPA) and deep (dLPA) LPA [1]. While the sLPA continues distal to the lateral aspect of the fifth digit, the dLPA commonly branches medially and courses deep to the oblique head of the adductor hallucis muscle, where it anastomoses with the DPA, a terminal branch of the dorsalis pedis artery that traverses proximally in the first intermetatarsal space between the two heads of the first dorsal interosseous muscle [3]. The MPA typically courses along the medial plantar foot and divides into both superficial (sMPA) and deep (dMPA) branches near the base of the first metatarsal [3]. The dMPA travels laterally between the abductor hallucis and flexor digitorum brevis and provides branches to plantar musculature, whereas the sMPA continues distally into the first digit, where it forms an anastomosis with the first plantar metatarsal artery. Branches of the MPA have not been described as providing vascular contributions to the deep plantar arch. However, connections between the MPA and LPA have been noted to form a superficial plantar arch superficial to the flexor digitorum brevis muscle [3]. The present case demonstrates a novel variation in the composition of the deep plantar arch identified bilaterally during cadaveric dissection, describes measurements of the medial and lateral plantar arteries and associated branches, and provides a discussion of the potential clinical implications of this finding.
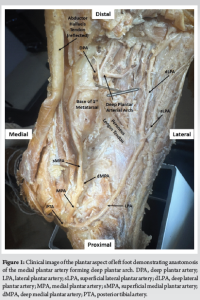
Following dissection of a 96-year-old Caucasian male cadaver, an anatomical variation of the deep plantar arterial arch was identified bilaterally. The dissection began with the reflection of the skin and plantar aponeurosis to expose the plantar foot musculature. Flexor digitorum brevis and abductor hallucis muscles were transected to expose the terminal split of the PTA into the LPA and MPA. The tendons of the flexor digitorum longus were reflected to allow visualization of the oblique head of the adductor hallucis. Both the flexor hallucis brevis and the oblique head of the adductor hallucis were removed using blunt dissection to expose the deep plantar arch and preserve the neurovasculature. The MPA was observed dividing into a superficial and deep branch at the level of the tarsometatarsal junction, with the sMPA continuing into the forefoot. Distal to the first metatarsophalangeal joint, the sMPA produced a branch that coursed laterally, anastomosing with the deep plantar artery in the region of the first intermetatarsal space to form the deep plantar arch (Fig. 1). The LPA traversed the lateral aspect of the plantar foot, where it split into superficial and deep branches at the base of the fifth metatarsal. The sLPA continued distally, and the dLPA was noted to course distally into the region of the second plantar interosseous muscle without contributing to the deep plantar arch. This variant was observed in both the right and left lower extremities and was independently confirmed and verified by a trained anatomist.
With the aid of a Vernier caliper (Mitutoyo, Takatsu-Ku, Kawasaki, Japan), measurements were taken of the medial and lateral plantar arteries with associated branches (Table 1). Arteries were measured at their respective branching points to maintain a constant reference point. Vessel diameter and distance measurements were similar between the right and left feet, with each measurement within 22% of its corresponding contralateral value. To estimate the prevalence of this variant, a total of 89 feet from 49 cadavers were examined for the morphology of the deep plantar arterial arch. The mean age of these cadavers was 70 years (range: 42–96 years), and included 25 females and 24 males. Of the 89 feet, only the two from the male cadaver described in this study exhibited this distinct morphology, resulting in an estimated prevalence of 2.3% of feet.

No approval or consent was required by the authors’ institutional biosafety committee, as this study involved a single cadaver.
The deep plantar arch is an area of marked anatomic variability, particularly in the dominance of vascular contributions [3,4]. Classically, the deep plantar arch has been depicted as an anastomosis between the dLPA and the DPA, with no noted contribution from the MPA [3,4]. Ozer et al. previously formulated a classification system to describe the variations in vascular supply to the deep plantar arch [4]. This classification, based upon a cadaveric analysis, includes three types:
- Type I: DPA dominant
- Type II: dLPA dominant
- Type III: Balanced contributions between DPA and dLPA
Their investigation found Type I arches to be the most common, representing 48% of specimens. Type II arches were identified in 38% of feet, and Type III were the least common at 14%. We propose a potential fourth variant (Type IV), in which the sMPA provides a dominant contribution to the deep plantar arch, forming an anastomosis with the DPA in the absence of contributions from the dLPA (Fig. 2). Embryologically, the axial artery is the primary artery that forms in the early lower limb bud and extends to the plantar surface of the foot. The PTA eventually develops through vasculogenesis, and the distal vessels form through a remodeling process with a plantar arterial plexus. The morphology identified in the present case could be the result of an aberration in the remodeling process [5]. This variation has not been previously described, potentially justifying a distinct categorization that may be of consequence during surgical procedures or injuries of the foot.

Defects in weight-bearing regions of the foot often require surgical reconstruction due to the unique functional demands of these areas [6]. Tissue on the plantar surface of the foot consists of thick, glabrous skin with fibrous subcutaneous septae that withstand repetitive shearing and ground reactive forces encountered with ambulation [7,8]. Due to the anatomical requirements of the tissues used for these reconstructive procedures, donor tissue flaps are often harvested from the region of the MPA and its perforators because of the non-weight-bearing properties of the regions they typically supply. This allows for skin grafts to cover the donor site with minimal impairment of ambulation [7,9]. More specifically, medial plantar (instep) fasciocutaneous flaps and MPA perforator (MPAP) flaps make the use of tissue associated with the sMPA and dMPA, respectively, to reapproximate soft-tissue defects [10]. As the plantar forefoot is primarily supplied by the LPA and DPA, ligation of the MPA branches to be used in flap procedures often does not compromise vascularization to these structures [7]. Furthermore, utilization of tissue from the medial plantar foot decreases post-procedural complications such as ulceration and flap ischemia, leading to decreased operative morbidity. Clinically, the presence of a Type IV variant would result in impaired vascular supply to the forefoot if the sMPA is utilized for a fasciocutaneous flap. This morphology limits the availability of non-weight-bearing tissue that could be used to reconstruct defects of the plantar foot. Furthermore, while simple defects of the foot can be repaired using skin grafts, these surgical sites are predisposed to post-procedural ulceration and hyperkeratosis if located in a weight-bearing region [9]. As such, feet with a Type IV variant may require an LPA-based flap for reconstruction. In addition, lacerations and fractures involving structures adjacent to the MPA could impair vascularization to the forefoot if the patient demonstrates a Type IV plantar arch.
The deep plantar arch was observed to be predominantly vascularized by the sMPA in a 96-year-old Caucasian male cadaver. This variation has not been described previously in the literature. The anomalous anastomotic morphology may predispose to complications following reconstructive foot surgery and contribute to post-procedural alterations in ambulatory status. As such, surgeons should consider this variant when performing reconstructive flap procedures of the foot to mitigate iatrogenic injuries.
Among its morphological variants, the deep plantar arch may be principally vascularized by the sMPA. As such, this should be considered during reconstructive procedures of the foot, particularly those requiring flap coverage. Pre-operative vascular imaging studies can be obtained to ensure arterial preservation and optimal wound healing.
References
- 1.Orbay H, Kerem M, Unlü RE, Esmer AF, Cömert A, Tüccar E, et al. Vascular anatomy of plantar muscles. Ann Plast Surg 2007;58:420-6. [Google Scholar | PubMed]
- 2.Murakami T. On the position and course of the deep plantar arteries, with special reference to the so-called plantar metatarsal arteries. Okajimas Folia Anat Jpn 1971;48:295-322. [Google Scholar | PubMed]
- 3.Standring S. Gray’s anatomy: The Anatomical Basis of Clinical Practice. 42nd ed. Philadelphia, PA: Elsevier; 2021. p. 1430-64. [Google Scholar | PubMed]
- 4.Ozer MA, Govsa F, Bilge O. Anatomic study of the deep plantar arch. Clin Anat 2005;18:434-42. [Google Scholar | PubMed]
- 5.Qazi E, Wilting J, Patel NR, Alenezi AO, Kennedy SA, Tan KT, et al. Arteries of the lower limb-embryology, variations, and clinical significance. Can Assoc Radiol J 2022;73:259-70. [Google Scholar | PubMed]
- 6.Bhandari PS, Srivastava V. Medial plantar artery flap for heel reconstruction: A 22-year follow-up. J Foot Ankle Surg (Asia-Pacific) 2022;10:220-3. [Google Scholar | PubMed]
- 7.Masadeh SB, Liette MD. The medial plantar artery: Anatomy and implications in local flaps of the foot. Plast Aesthet Res 2023;10:54. [Google Scholar | PubMed]
- 8.Velazquez-Mujica J, Amendola F, Spadoni D, Chen HC. Restoring blood flow to the lateral plantar artery after elevation of an instep flap or medialis pedis flap. Arch Plast Surg 2022;49:80-5. [Google Scholar | PubMed]
- 9.Yuen JC, Shahare HM, Hicks ED. Reverse-flow flaps of the medial plantar region: Review of the literature with case report. Plast Reconstr Surg Glob Open 2025;13:e6471. [Google Scholar | PubMed]
- 10.Guillier D, Cherubino M, Oranges CM, Giordano S, Raffoul W, Di Summa PG. Systematic reappraisal of the reverse-flow medial plantar flap: From vascular anatomical concepts to surgical applications. J Plast Reconstr Aesthet Surg 2020;73:421-33. [Google Scholar | PubMed]