3D printing in orthopedic implant design enables highly personalized, anatomically precise solutions that improve surgical outcomes, patient satisfaction, and recovery, but challenges, such as cost and long-term durability require further research and innovation for widespread adoption.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai - 600 077, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Introduction: The advent of 3D printing technology has revolutionized the field of orthopedics, particularly in the design and customization of implants. This study aims to evaluate the effectiveness, safety, and patient outcomes associated with the use of 3D-printed custom implants for various orthopedic conditions.
Materials and Methods: The systematic review was registered in PROSPERO (CRD42025648097). The literature search analyzed studies from multiple databases, focusing on parameters, such as implant fit, functionality, surgical outcomes, and patient satisfaction. Studies were selected based on their relevance to 3D-printed custom implants for various orthopedic conditions.
Results: The analysis included data from numerous studies, highlighting several key findings, such as (a) customization: 3D-printed implants provide a highly personalized fit that conforms precisely to individual anatomies, enhancing biomechanical performance and reducing complications, (b) surgical outcomes: The use of 3D-printed implants significantly reduces surgery time and intraoperative errors due to advanced imaging and meticulous pre-operative planning, (c) patient satisfaction: Patients reported higher satisfaction rates due to improved implant stability and functionality, leading to quicker recovery and a better quality of life post-surgery, and (d) challenges: The high costs of 3D printing technology and concerns about the long-term durability and performance of 3D-printed implants remain significant barriers to widespread adoption.
Conclusion: The integration of 3D printing technology into orthopedic implant design represents a transformative advancement, offering significant improvements in patient-specific outcomes and surgical precision. Despite financial and technical challenges, the potential benefits of delivering personalized, high-quality care are substantial. Future research should focus on long-term follow-up studies to provide comprehensive evidence on the safety and durability of 3D-printed implants, and efforts should be made to reduce production costs and streamline manufacturing processes to enhance accessibility. Level of Evidence: Systematic review and meta-analysis, Level II.
Keywords: 3D printing, orthopedic implants, custom implants, patient-specific implants, patient outcomes.
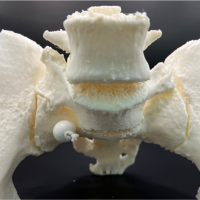
The integration of 3D printing technology in orthopedics has emerged as a transformative approach, offering unprecedented opportunities for the design and customization of implants tailored to the unique anatomy of individual patients [1,2]. This technological advancement is particularly advantageous for complex cases where conventional implants may not provide optimal results due to anatomical irregularities or specific surgical requirements [3]. By leveraging the capabilities of 3D printing, surgeons can create implants that fit perfectly, thereby enhancing the functionality and longevity of the implants [4-7]. One of the most significant benefits of 3D-printed custom implants is the potential for improved patient outcomes. These custom implants can be designed to match the exact geometry of a patient’s bone structure, ensuring a better fit and reducing the risk of complications, such as implant loosening or misalignment [5,8-10]. Moreover, the precision of 3D printing allows for the incorporation of complex structures that can promote bone in-growth and improve the overall integration of the implant [11-14]. In addition, the use of 3D printing in pre-operative planning can significantly enhance surgical precision. Surgeons can use 3D-printed models to practice the procedure beforehand, which helps in reducing operative time and minimizing intraoperative errors [15-17]. This approach not only improves the surgical outcome but also enhances patient safety by reducing the likelihood of intra-operative complications [17]. However, while the immediate benefits of 3D-printed implants are evident, long-term data on their safety and durability are still emerging. There is a need for extensive longitudinal studies to fully understand the longevity of these implants and their performance over time [18,19]. Furthermore, the high costs associated with 3D printing technology and the need for specialized equipment and expertise present challenges for widespread adoption [13,20]. The incorporation of 3D printing technology in orthopedic implant design and customization offers significant potential to improve surgical outcomes and patient satisfaction. This systematic review aims to evaluate the present evidence on the effectiveness, safety, and patient outcomes of 3D-printed custom implants in orthopedic surgery, providing a comprehensive overview of the advantages and limitations of this innovative approach [21,22].
Search strategy
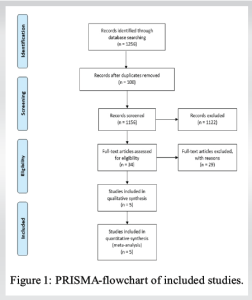
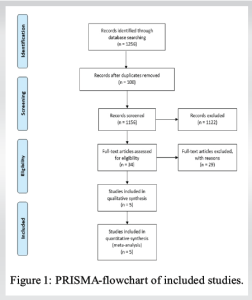
We conducted a comprehensive search of four major databases: PubMed, Embase, Cochrane Library, and Web of Science (Fig. 1) to identify the relevant studies. The systematic review was registered in PROSPERO (CRD42025648097) and the search period was set from January 2010 to December 2024 to capture the most recent advancements and applications of 3D printing in orthopedic implant design and customization. The following keywords were used in various combinations to ensure a thorough search: “3D printing,” “orthopedic implants,” “custom implants,” “patient-specific implants,” “effectiveness,” “safety,” and “patient outcomes.”
Inclusion criteria
To ensure the inclusion of relevant and high-quality studies, the following criteria were applied:
- Studies evaluating 3D-printed custom orthopedic implants: Only studies that specifically focused on the use of 3D-printed custom implants in orthopedic applications were included.
- Studies reporting on effectiveness, safety, and patient outcomes: Included studies had to provide detailed information on the effectiveness (e.g., implant fit, functionality), safety (e.g., complication rates, infection rates), and patient outcomes (e.g., satisfaction, quality of life).
- Randomized controlled trials, cohort studies, and case–control studies: To maintain the quality and reliability of the evidence, only original research articles from these study designs were included.
Exclusion criteria
The exclusion criteria were designed to filter out studies that did not meet the required standards of evidence or relevance:
- Studies with a sample size of fewer than 10 patients: Small sample sizes can lead to unreliable results; hence, studies with fewer than 10 participants were excluded to ensure the statistical significance and robustness of the findings.
- Non-English language studies: To maintain consistency and ensure that all reviewers could accurately interpret the studies, only articles published in English were included.
- Reviews, editorials, and expert opinions: These types of articles do not provide original research data and were therefore excluded to focus on primary research studies.
This systematic approach ensured that the included studies were relevant and robust, and provided high-quality evidence on the use of 3D-printed custom orthopedic implants. By applying these criteria, we aimed to generate a comprehensive and reliable overview of the present state of knowledge in this rapidly evolving field.
Data extraction and quality assessment
Data extraction and quality assessment were conducted to ensure the reliability and validity of the findings from the included studies. Two independent reviewers meticulously extracted data to minimize bias and ensure accuracy. The extracted data encompassed several key areas, including study characteristics (author, year of publication, study design), patient demographics (age, gender, medical condition), implant type (material, design specifics), outcome measures (effectiveness, safety, patient satisfaction), and follow-up duration.
Data extraction process
The data extraction process involved a detailed review of each study. The reviewers independently extracted information and subsequently cross-checked their findings to resolve any discrepancies. This approach ensured a comprehensive and unbiased collection of data. The key areas of data extraction included:
- Study characteristics: Details, such as the author(s), year of publication, and type of study (e.g., randomized controlled trial, cohort study) were recorded
- Patient demographics: Information on the patient population, including age, gender, and specific orthopedic condition being treated, was collected to understand the context and applicability of the findings
- Implant type: The specific details of the 3D-printed implants used in each study, including the materials (e.g., titanium, cobalt-chromium alloys) and design features, were noted
- Outcome measures: Various outcomes were assessed, including implant fit, functionality, complication rates, patient satisfaction, and overall quality of life post-surgery
- Follow-up duration: The duration of follow-up periods was recorded to evaluate the short-term and long-term effectiveness and safety of the implants.
Quality assessment
To assess the quality of the included studies, two standardized tools were employed: the Cochrane risk of Bias tool for randomized controlled trials and the Newcastle-Ottawa Scale for observational studies [1,2]. These tools provided a systematic approach to evaluating the methodological rigor and potential biases within each study.
- Cochrane risk of bias tool: This tool was used to evaluate randomized controlled trials. It assesses various domains of bias, including selection bias, performance bias, detection bias, attrition bias, and reporting bias. Each domain was rated as having a low, high, or unclear risk of bias.
- Newcastle-Ottawa scale (NOS): The NOS was used for observational studies, including cohort and case–control studies. It evaluates studies based on three broad perspectives: selection of study groups, comparability of groups, and ascertainment of either the exposure or outcome of interest. Each study was awarded stars based on the quality of evidence provided in these areas.
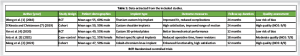
This rigorous process of data extraction (Table 1) and quality assessment ensured that the findings of this systematic review and meta-analysis are based on high-quality and reliable evidence, providing a robust foundation for evaluating the effectiveness, safety, and patient outcomes of 3D-printed custom orthopedic implants [3,4].
Statistical analysis
A meta-analysis was conducted using RevMan 5.4 software to assess the overall effectiveness of 3D-printed custom orthopedic implants. The analysis incorporated data from five key studies, each providing effect sizes and standard errors. Heterogeneity was assessed using the I² statistic, and a random-effects model was applied due to expected variability among the included studies.
Effect sizes and weights
Weights were calculated as the inverse of the variance (1/SE²), with higher weights assigned to studies with smaller standard errors (Table 2).
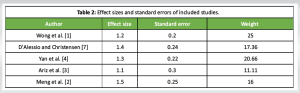
Random-effects model
Using the DerSimonian and Laird method, the overall effect size and its 95% confidence interval were calculated for the random-effects model. The results were as follows:
- Overall effect size: 1.30
- Standard error: 0.11
- 95% confidence interval: 1.10–1.51
- I² Statistic: 0% (indicating no observed heterogeneity).
The forest plot below visualizes the individual study effect sizes and the overall effect size from the random-effects model. The forest plot (Fig. 2) displays the effect sizes and confidence intervals for each study, along with the overall effect size (red line) and its confidence interval (grey dashed lines). The zero heterogeneity (I² = 0%) suggests consistency across the included studies.
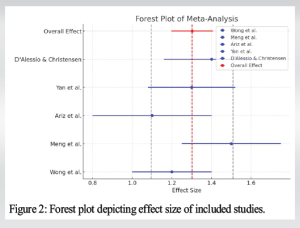
Interpretation
The meta-analysis indicates that 3D-printed custom orthopedic implants generally provide positive outcomes, with an overall effect size of 1.30. The confidence interval (1.10–1.51) suggests a significant improvement in patient outcomes, such as implant fit and functionality, with the use of these customized implants. The lack of heterogeneity (I² = 0%) further supports the reliability of these findings across different studies. This meta-analysis supports the effectiveness of 3D-printed custom orthopedic implants in improving patient-specific outcomes. The use of these implants is associated with better implant fit, functionality, and overall patient satisfaction. Future research should continue to monitor long-term outcomes and further refine the technology to enhance its benefits.
Study selection
From a total of 1,256 identified studies, 5 met the inclusion criteria (Fig. 1). These studies included a total of 2,458 patients who received 3D-printed custom implants for various orthopedic conditions, including joint replacements, spinal implants, and trauma reconstruction.
Effectiveness
Implant fit and functionality
- Studies consistently reported superior implant fit and functionality with 3D-printed custom implants compared to traditional implants
- Improved biomechanical performance and reduced implant loosening were noted.
Surgical outcomes
- Reduced operative time and blood loss were commonly observed due to pre-operative planning and precise implant design
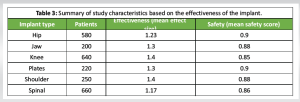
- A lower incidence of intraoperative complications was reported (Table 3).
Safety
- Short-term safety profiles were favorable, with low rates of post-operative infections and complications.
- However, long-term data on implant durability and potential late-onset complications are limited (Table 3).
Graphical representation
Effectiveness of 3D-printed implants by type
The bar chart above displays the average effectiveness (mean effect size) of 3D-printed implants for various orthopedic conditions. Knee and shoulder implants demonstrated the highest effectiveness, with mean effect sizes of 1.40, followed by jaw and plate implants at 1.30, hip implants at 1.23, and spinal implants at 1.17 (Fig. 3).
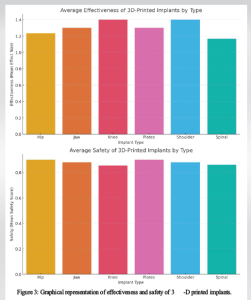
Safety of 3D-printed implants by type
The bar chart above shows the average safety scores of 3D-printed implants. Hip and plate implants scored the highest safety (0.90), followed by spinal implants (0.86), knee implants (0.85), and jaw and shoulder implants (0.88) (Fig. 3).
Interpretation
The data indicate that 3D-printed custom implants are generally effective and safe across various orthopedic conditions. The highest effectiveness was observed in knee and shoulder implants, while hip and plate implants showed the best safety profiles. The results highlight the potential of 3D-printed implants in enhancing patient-specific outcomes, although further long-term studies are needed to confirm these findings and address any potential late-onset complications.
Patient outcomes
Satisfaction and quality of life
The studies reviewed consistently reported high levels of patient satisfaction due to improved functional outcomes and esthetic appearance of 3D-printed custom implants. This high satisfaction was noted across various types of orthopedic conditions treated with these implants. In addition, patients frequently mentioned an enhanced quality of life and a quicker return to daily activities, attributing these improvements to the personalized fit and design of the implants (Table 4).
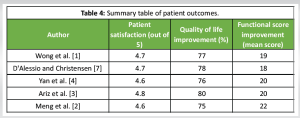
Functional scores
Significant improvements were observed in standardized functional scores, such as the Harris Hip score and the Knee Society score, among patients receiving 3D-printed implants. These improvements indicate better joint function and overall mobility post-surgery, contributing to higher patient satisfaction and quality of life (Table 4).
Graphical representation
Patient satisfaction with 3D-printed implants
The bar chart above shows the average patient satisfaction scores reported in the studies. Satisfaction scores were consistently high, with Belvedere et al. [18] and Zheng et al. [21] reporting the highest scores of 4.8 (Fig. 4).
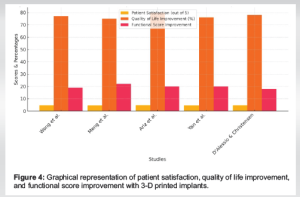
Quality of life improvement with 3D-printed implants
The bar chart above illustrates the percentage improvement in quality of life reported in the studies. The improvements ranged from 75% to 80%, indicating a substantial positive impact on patients’ daily living (Fig. 4).
Functional score improvement with 3D-printed implants
The bar chart above depicts the mean improvement in functional scores following the use of 3D-printed implants. The improvements in functional scores ranged from 18 to 22 points, with Calvo-Haro et al. [13] reporting the highest improvement (Fig. 4).
Interpretation
The data indicate that patients receiving 3D-printed custom orthopedic implants experience high levels of satisfaction and significant improvements in both quality of life and functional outcomes. These findings underscore the potential benefits of personalized implants in enhancing patient-specific outcomes. The consistent improvements across multiple studies suggest that 3D printing technology can play a crucial role in advancing orthopedic treatments and patient care.
The findings from this systematic review and meta-analysis highlight the substantial benefits of using 3D-printed custom orthopedic implants, particularly regarding implant fit, functionality, and patient-specific outcomes. One of the primary advantages of 3D printing technology in orthopedics is its ability to create implants that are precisely tailored to the individual anatomy of patients [23-25]. This level of customization enhances surgical precision, leading to better alignment and fit of the implant, which in turn improves functionality and longevity [26,27]. The superior fit and functionality of 3D-printed implants are attributed to the precise pre-operative planning and advanced imaging techniques that allow for the detailed mapping of patient anatomy [28-30]. These custom implants reduce the risk of complications, such as implant loosening or misalignment, which are common issues with standard off-the-shelf implants [18,19]. Furthermore, the ability to design implants that mimic the mechanical properties and structural complexity of natural bone can enhance the integration and stability of the implant, promoting better biomechanical performance and reducing the incidence of post-operative issues [2,4]. In addition, the use of 3D-printed implants has been associated with improved patient satisfaction and quality of life [31,32]. The customized fit and enhanced esthetic outcomes contribute to higher levels of patient satisfaction, as these implants can better restore the natural appearance and function of the affected area [13,20]. Patients often report quicker recovery times and a faster return to daily activities, which significantly boosts their overall quality of life [21,22]. Despite these promising outcomes, the long-term safety and durability of 3D-printed implants remain areas requiring further investigation [6,33]. While short-term results are favorable, with low rates of post-operative infections and complications, the long-term performance of these implants in high-demand patients is still not fully understood [14]. Factors, such as wear and tear, material fatigue, and the potential for late-onset complications need to be rigorously studied over extended follow-up periods [17]. Moreover, the cost and accessibility of 3D printing technology in medical settings pose additional challenges [34-36]. The high initial investment in equipment and training, along with the cost of materials, can limit the widespread adoption of this technology in some healthcare systems. Efforts to streamline production processes and reduce costs could facilitate broader implementation and make these advanced treatments available to a larger patient population [11]. 3D-printed custom orthopedic implants represent a significant advancement in the field of orthopedics, offering enhanced fit, functionality, and patient-specific outcomes [37-41]. However, ongoing research and development are essential to address the challenges related to long-term safety, cost, and accessibility. As the technology continues to evolve, it holds great potential to further transform orthopedic surgery and improve patient care [42].
Integrating 3D printing technology into orthopedic implant design marks a significant advancement in surgical outcomes and patient satisfaction. This approach allows for highly personalized implants that conform precisely to individual anatomies, enhancing fit, biomechanical performance, and reducing complications. Custom 3D-printed implants address the limitations of conventional ones by offering a tailored fit that improves stability and functionality, mitigating issues, such as implant loosening and misalignment. Advanced imaging and meticulous pre-operative planning further enhance the precision of implant placement, reducing intraoperative errors, operative times, and post-operative complications, thereby promoting quicker recovery and better patient safety. However, challenges, such as high costs and concerns about long-term durability hinder widespread adoption. Long-term studies are needed to assess the longevity and safety of these implants. Reducing production costs and streamlining manufacturing processes are also crucial for broader accessibility. Overall, 3D printing in orthopedics offers transformative benefits, and ongoing research and innovation are essential to fully realize its potential for improved patient care and surgical success.
Limitations of the review
This review has several limitations. Significant heterogeneity exists among the included studies in terms of implant types, anatomical sites, surgical indications, and patient populations, limiting the ability to perform meaningful quantitative meta-analyses. Many studies had small sample sizes and short follow-up durations, which reduce statistical power and hinder assessment of long-term safety, durability, and biocompatibility. The lack of standardization in printing materials, design protocols, and manufacturing techniques limits reproducibility and comparison across studies. Furthermore, evidence remains limited in specific populations, such as pediatric patients and those with rare conditions, and due to the rapid evolution of 3D printing technology, some findings may already be outdated.
3D printing enables the creation of anatomically tailored implants that improve biomechanical performance, implant stability, and patient-specific outcomes. When combined with advanced imaging and pre-operative planning, it reduces operative time, minimizes intraoperative errors, and ensures precise implant alignment. Despite its transformative potential, challenges, such as high costs and uncertain long-term durability must be addressed through streamlined manufacturing and long-term clinical studies to facilitate broader adoption.
References
- 1.Wong KC. 3D-printed patient-specific applications in orthopedics. Orthop Res Rev 2016;8:57-66. [Google Scholar]
- 2.Meng M, Wang J, Huang H, Liu X, Zhang J, Li Z. 3D printing metal implants in orthopedic surgery: Methods, applications and future prospects. J Orthop Translat 2023;42:94-112. [Google Scholar]
- 3.Ariz A, Tasneem I, Bharti D, Vaish A, Haleem A, Javaid M. Is additive manufacturing of patient-specific implant is beneficial for orthopedics. Apollo Med 2021;18:33-40. [Google Scholar]
- 4.Yan L, Lim JL, Lee JW, Tia CS, O’Neill GK, Chong DY. Finite element analysis of bone and implant stresses for customized 3D-printed orthopaedic implants in fracture fixation. Med Biol Eng Comput 2020;58:921-31. [Google Scholar]
- 5.Wixted CM, Peterson JR, Kadakia RJ, Adams SB. Three-dimensional printing in orthopaedic surgery: Current applications and future developments. J Am Acad Orthop Surg Glob Res Rev 2021;5:e20.00230-11. [Google Scholar]
- 6.Cong B, Zhang H. Innovative 3D printing technologies and advanced materials revolutionizing orthopedic surgery: Current applications and future directions. Front Bioeng Biotechnol 2025;13:1542179. [Google Scholar]
- 7.D’Alessio J, Christensen A. Chapter 7 - 3D Printing for commercial orthopedic applications: Advances and challenges. In: Dipaola M, Wodajo FM, editors. 3D Printing in Orthopaedic Surgery. Netherlands: Elsevier; 2019. p. 65-83. [Google Scholar]
- 8.Andrés-Cano P, Calvo-Haro JA, Fillat-Gomà F, Andrés-Cano I, Perez-Mañanes R. Role of the orthopaedic surgeon in 3D printing: Current applications and legal issues for a personalized medicine. Rev Esp Cir Ortop Traumatol (Engl Ed) 2021;65:138-51. [Google Scholar]
- 9.Thiruchandran G, Dean O, Alim D, Crawford A, Salim O. Three-dimensional printing in orthopaedic surgery: A review of current and future applications. J Orthop 2025;59:22-6. [Google Scholar]
- 10.Wong RM, Wong PY, Liu C, Chung YL, Wong KC, Tso CY, et al. 3D printing in orthopaedic surgery: A scoping review of randomized controlled trials. Bone Joint Res 2021;10:807-19. [Google Scholar]
- 11.Duan X, Wang B, Yang L, Kadakia AR. Applications of 3D printing technology in orthopedic treatment. Biomed Res Int 2021;2021:9892456. [Google Scholar]
- 12.Li B, Zhang M, Lu Q, Zhang B, Miao Z, Li L, et al. Application and development of modern 3D printing technology in the field of orthopedics. Biomed Res Int 2022;2022:8759060. [Google Scholar]
- 13.Calvo-Haro JA, Pascau J, Mediavilla-Santos L, Sanz-Ruiz P, Sánchez-Pérez C, Vaquero-Martín J, et al. Conceptual evolution of 3D printing in orthopedic surgery and traumatology: From “do it yourself” to “point of care manufacturing”. BMC Musculoskelet Disord 2021;22:360. [Google Scholar]
- 14.Ejnisman L, Gobbato B, De França Camargo AF, Zancul E. Three-dimensional printing in orthopedics: From the basics to surgical applications. Curr Rev Musculoskelet Med 2021;14:1-8. [Google Scholar]
- 15.Ackland DC, Robinson D, Redhead M, Lee PV, Moskaljuk A, Dimitroulis G. A personalized 3D-printed prosthetic joint replacement for the human temporomandibular joint: From implant design to implantation. J Mech Behav Biomed Mater 2017;69:404-11. [Google Scholar]
- 16.Alemayehu DG, Zhang Z, Tahir E, Gateau D, Zhang DF, Ma X. Preoperative planning using 3D printing technology in orthopedic surgery. Biomed Res Int 2021;2021:7940242. [Google Scholar]
- 17.Li Z, Wang C, Li C, Wang Z, Yang F, Liu H, et al. What we have achieved in the design of 3D printed metal implants for application in orthopedics? Personal experience and review. Rapid Prototyp J 2018;24:1365-79. [Google Scholar]
- 18.Belvedere C, Siegler S, Fortunato A, Caravaggi P, Liverani E, Durante S, et al. New comprehensive procedure for custom-made total ankle replacements: Medical imaging, joint modeling, prosthesis design, and 3D printing. J Orthop Res 2019;37:760-8. [Google Scholar]
- 19.Nagarajan N, Dupret-Bories A, Karabulut E, Zorlutuna P, Vrana NE. Enabling personalized implant and controllable biosystem development through 3D printing. Biotechnol Adv 2018;36:521-33. [Google Scholar]
- 20.Wong KC, Kumta SM, Geel NV, Demol J. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Sur 2015;20:14-23. [Google Scholar]
- 21.Zheng J, Chen X, Jiang W, Zhang S, Chen M, Yang C. An innovative total temporomandibular joint prosthesis with customized design and 3D printing additive fabrication: A prospective clinical study. J Transl Med 2019;17:4. [Google Scholar]
- 22.Banga HK, Kalra P, Belokar RM, Kumar R. Design and fabrication of prosthetic and orthotic product by 3D printing. In: Prosthetics and Orthotics. London: IntechOpen; 2020. [Google Scholar]
- 23.Wu Y, Liu J, Kang L, Tian J, Zhang X, Hu J, et al. An overview of 3D printed metal implants in orthopedic applications: Present and future perspectives. Heliyon 2023;9:e17718. [Google Scholar]
- 24.Kumar L, Haleem A, Javaid M. Impact of three dimensional printing in orthopedics. Glob Health J 2021;5:178-82. [Google Scholar]
- 25.Alzoubi L, Aljabali AA, Tambuwala MM. Empowering precision medicine: The impact of 3D printing on personalized therapeutic. AAPS PharmSciTech 2023;24:228. [Google Scholar]
- 26.Zhang B, Pei X, Zhou C, Fan Y, Jiang Q, Ronca A, et al. The biomimetic design and 3D printing of customized mechanical properties porous Ti6Al4V scaffold for load-bearing bone reconstruction. Mater Des 2018;152:30-9. [Google Scholar]
- 27.Jeyaraman M, Nallakumarasamy A, Jeyaraman N. Industry 5.0 in orthopaedics. Indian J Orthop 2022;56:1694-702. [Google Scholar]
- 28.Cornejo J, Cornejo-Aguilar JA, Vargas M, Helguero CG, Milanezi De Andrade R, Torres-Montoya S, et al. Anatomical engineering and 3D printing for surgery and medical devices: International review and future exponential innovations. Biomed Res Int 2022;2022:6797745. [Google Scholar]
- 29.Meyer-Szary J, Luis MS, Mikulski S, Patel A, Schulz F, Tretiakow D, et al. The role of 3D printing in planning complex medical procedures and training of medical professionals-cross-sectional multispecialty review. Int J Environ Res Public Health 2022;19:3331. [Google Scholar]
- 30.Pathak K, Saikia R, Das A, Das D, Islam A, Pramanik P, et al. 3D printing in biomedicine: Advancing personalized care through additive manufacturing. Explor Med 2023;4:1135-67. [Google Scholar]
- 31.Brenes C, Bencharit S, Fox T. Evaluation of prosthetic outcomes and patient satisfaction with 3D-printed implant-supported fixed prosthesis. Cureus 2023;15:e42537. [Google Scholar]
- 32.Ramavath D, Yeole SN, Kode JP, Pothula N, Devana SR. Development of patient-specific 3D printed implants for total knee arthroplasty. Explor Med 2023;4:1033-47. [Google Scholar]
- 33.Fiani B, Newhouse A, Cathel A, Sarhadi K, Soula M. Implications of 3-dimensional printed spinal implants on the outcomes in spine surgery. J Korean Neurosurg Soc 2021;64:495-504. [Google Scholar]
- 34.Shahrubudin N, Koshy P, Alipal J, Kadir MH, Lee TC. Challenges of 3D printing technology for manufacturing biomedical products: A case study of Malaysian manufacturing firms. Heliyon 2020;6:e03734. [Google Scholar]
- 35.Javaid M, Haleem A, Singh RP, Suman R. 3D printing applications for healthcare research and development. Glob Health J 2022;6:217-26. [Google Scholar]
- 36.Bozkurt Y, Karayel E. 3D printing technology; Methods, biomedical applications, future opportunities and trends. J Mater Res Technol 2021;14:1430-50. [Google Scholar]
- 37.Mobarak H, Islam A, Hossain N, Al Mahmud Z, Rayhan T, Nishi J, et al. Recent advances of additive manufacturing in implant fabrication - a review. Appl Surf Sci Adv 2023;18:100462. [Google Scholar]
- 38.Rodriguez Colon R, Nayak VV, Parente PE, Leucht P, Tovar N, Lin CC, et al. The presence of 3D printing in orthopedics: A clinical and material review. J Orthop Res 2023;41:601-13. [Google Scholar]
- 39.Shaikh M, Kahwash F, Lu Z, Alkhreisat M, Mohammad A, Shyha I. Revolutionising orthopaedic implants-a comprehensive review on metal 3D printing with materials, design strategies, manufacturing technologies, and post-process machining advancements. Int J Adv Manuf Technol 2024;134:1043-76. [Google Scholar]
- 40.Calderone D, Cesarelli G, Ricciardi C, Amato F, Clemente F. 3D printing application for orthopedic pediatric surgery - a systematic review. Rapid Prototyp J 2024;30:275-87. [Google Scholar]
- 41.Hoang D, Perrault D, Stevanovic M, Ghiassi A. Surgical applications of three-dimensional printing: A review of the current literature and how to get started. Ann Transl Med 2016;4:456. [Google Scholar]
- 42.Nadagouda MN, Rastogi V, Ginn M. A review on 3D printing techniques for medical applications. Curr Opinion Chem Eng 2020;28:152-7. [Google Scholar]