Management of terrible tetrad injury of the elbow requires meticulous surgery to achieve anatomic fracture fixation of the olecranon and coronoid, radial head fixation or replacement, and repair of the ligamentous injury, if any.
Dr. Kumar Keshav, Apex Trauma Centre, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Vrindavan Yojna, Raebareli Road, Lucknow - 226029, Uttar Pradesh., India. E-mail: keshav4700@yahoo.co.in
Introduction: The terrible triad of the elbow (TTE) is a well-described entity characterized by a triad of elbow dislocation, fractures of the radial head, and coronoid. Historically, these fractures gave poor clinical outcomes, and hence, the name “terrible triad.” There are many variants of TTE that may lead to poor prognosis if not adequately dealt with. One such variant is the association of TTE with olecranon fracture, which has not been adequately described in the literature. There have been just three papers (one case series and two case reports) on this variant of TTE, and the prognosis has been poor. We are describing one such case of “terrible tetrad of elbow.”
Case Report: A 44-years-old male patient presented at 3 weeks following a road traffic injury with a painful, swollen left elbow and gross instability. Radiography revealed a terrible triad injury of the left elbow along with an olecranon fracture. The radial head was unsalvageable and required replacement by Kocher’s approach. Flexor carpi ulnaris (FCU) split medial approach was used for coronoid fixation. The same skin incision was used to reach the olecranon through FCU-extensor carpi ulnaris (ECU) interval. The olecranon was fixed with a 3.5 mm pre-contoured plate and coronoid by 2 lag screws passed in a posteroanterior direction and a 2.7 mm buttress T-plate. Intraoperatively, after bony fixations, there was no varus-valgus instability, and hence ligaments did not require repair. Post-operatively, the elbow was kept immobilized for 3 weeks, following which physiotherapy was started. At the final follow-up at 18 months, the patient achieved an excellent functional outcome based on the mayo elbow performance index.
Conclusion: The Terrible tetrad of the elbow seems challenging to manage with a historically dismal prognosis. It is critical to pay close attention to each destabilizing feature of the injury, which places a great demand on the surgeon’s understanding of the anatomic intricacies of the elbow. Management of these complicated constellations of injuries requires anatomic fracture fixation of the olecranon and coronoid, radial head fixation or replacement, and ligamentous repair or reconstruction, if any.
Keywords: Elbow fracture, elbow instability, terrible triad, olecranon fracture, terrible triad of elbow, terrible tetrad.
The Terrible triad of the elbow (TTE) is a well-described entity characterized by a triad of elbow dislocation, fractures of the radial head, and coronoid. Historically, these fractures gave poor clinical outcomes, and hence the name “terrible triad” [1]. These fractures are relatively rare, and some of their described variants are even more rare. Medina et al. published a systematic review of the triad, associated ipsilateral upper limb injuries, and the variants of TTE in 2023 [2]. The rarity of the association of TTE with olecranon fracture can be gauged from the fact that it has been mentioned in just three papers [3-5]. Out of the overall nine cases described so far, seven have been mentioned as a case series by Cavigilia et al. Out of the seven patients that they operated on, four had to be reoperated, and the results were mostly fair or poor. Due to the complexity of the case, it was labeled as “Terrible Tetrad” by the authors [3]. Apart from this case series, there is just one more such case in a skeletally mature patient, published by Zha et al., who did not report a good functional outcome [4]. The last case was of a pediatric patient authored by Dailiana et al. [5] However, the “Terrible tetrad of elbow” case that we are going to describe had an excellent outcome, because of our strategy of addressing the individual injuries thoroughly, good fixation of the fractures and initiating early mobilization of the elbow.
History and clinical examination
A man in his mid-40s with a body mass index of 34.2 presented 3 weeks after a road traffic injury with a painful, swollen left elbow. This was initially managed with an arm pouch sling provided at a different healthcare facility. On physical examination of the elbow, there was tenderness, instability, and an inability to move the elbow due to pain. Pain over the radial head, varus-valgus instability, and anteroposterior (AP) instability in the flexed position of the elbow was enough to raise a suspicion of TTE.
Investigations
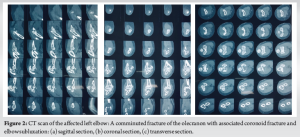
Standard AP and lateral radiographs of the left elbow (Fig. 1) revealed an olecranon fracture with a radial head fracture, which still did not explain the gross instability in both planes. Hence, a CT scan (Fig. 2) was done, which revealed a fracture of the coronoid (Regan and Morrey Type II, O’Driscoll Type II) along with elbow subluxation [6,7]. Ideally, an MRI should have been done to see the status of the ligaments, but we were unable to get one due to some logistic concerns at our institute. As the injury was already 3 weeks old and did not want to delay further, we decided to go ahead with the surgery, and had any ligamentous instability been found after bony fixations during the surgery, we would have repaired that by suture anchors. All of this was explained to the patient and then only he was posted for surgery.

Differential diagnosis
The injury pattern described above can fall into one of the three entities: (i) complex elbow fracture without dislocation, (ii) TTE with olecranon fracture (terrible tetrad of elbow), and (iii) trans-olecranon fracture dislocation [2-10]. In cases of complex elbow fracture without dislocation, the patient presents with a fracture involving the bones of the elbow joint without any accompanying dislocation of the joint. It’s a kind of multiple fractures of the radial head/neck and proximal ulna due to direct impact [9]. Second, the TTE with olecranon fracture, known as “terrible tetrad,” consists of a combination of four injuries: elbow dislocation, radial head fracture, coronoid fracture, and olecranon fracture. This complex presentation can lead to significant instability and functional impairment [3-5]. Finally, trans-olecranon fracture dislocation refers to a rare and severe injury, characterized by the simultaneous fracture of the olecranon and the dislocation of the elbow joint through the olecranon fracture. Unlike the terrible tetrad, the proximal part of the olecranon is in its native place [10]. Accurate diagnosis of these conditions is crucial for proper surgical planning and optimal patient outcomes. A thorough clinical evaluation and specialized imaging studies, such as CT scans to see the bony injuries and MRIs to assess the condition of ligaments, intra-articular cartilage, and associated inflammation/effusion are necessary to differentiate between these conditions and provide appropriate care.
Treatment
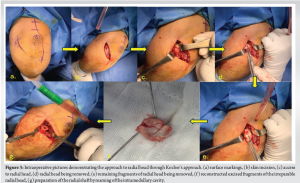
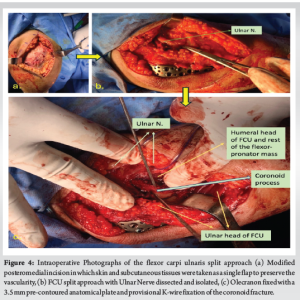
The goal of surgery was to achieve anatomical reduction and fixation of fractures, replacement of radial head, and repair of injured ligaments, if any, thereby achieving enough stability of the elbow for allowing early mobilization. We had 2.5 mm and 3.5 mm plating sets, radial head prosthesis, and suture anchors in our armamentarium before going in for surgery. The next issue in our planning was exposure since we had to address all three components of the TTE along with the olecranon. The radial head and lateral ulnar collateral ligament injury (if found to be present) would have required a lateral Kocher or Kaplan approach. Now, we would have been left with fixing olecranon and coronoid. Usually, for olecranon, the approach is pure posterior and for coronoid (and for addressing possible MCL injury), it is pure medial. Hence, to address both the fractures-olecranon and coronoid, the planned incision was midway, that is, posteromedial. The patient was operated in a lateral decubitus position with the arm supported over an arm holder. The surgery was done under a tourniquet. Kocher’s lateral approach was used to reach the radial head. It was found to be comminuted with multiple small irreparable fragments. The fragmented radial head was removed and a radial head arthroplasty (Fig. 3) was done. Next, a posteromedial incision was made, somewhere between the medial FCU split approach and the posterior approach between FCU and ECU for fixing olecranon. The skin and subcutaneous tissues were raised as a single flap to preserve the vascularity. On deeper dissection, we digressed on either side of the ulnar head of FCU. On the lateral side, the plane between FCU and ECU was used for fixing the olecranon. On the medial side of the ulnar head of the FCU, the ulnar nerve was isolated from between the two heads of the FCU. This FCU split approach was used to reach coronoid. The ulnar head of FCU had to be adequately mobilized for achieving this (Fig. 4). Olecranon plating was done using a 3.5 mm pre-contoured anatomical plate. The coronoid process, which is the key to elbow stability, was fixed through 2 large screws from posterior to anterior and buttressed by a 2.7 mm T-plate (Fig. 5). At this stage, AP and mediolateral stability of the elbow was assessed by fluoroscopy in the functional range of motion (ROM) of 30° to 130°. The elbow was found to be stable with no incongruency. Post-operatively, an above elbow slab was applied in 90° flexion and pronation for 3 weeks, following which active ROM exercises were started along with radiographic check X-rays at each visit to check for joint congruency and stability (Fig. 6).
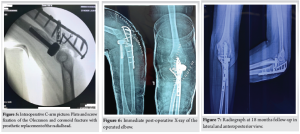
Outcome and follow-up
At the final follow-up at 18 months (Fig. 7), the patient was mostly pain-free and able to perform his normal routine activities. His elbow was stable, and the ROM in the flexion-extension arc was 10°–130°. The supination and pronation reached 80° each way (Fig. 8). The Carrying angle was around 10° of valgus in maximal supination. There was no evidence of heterotrophic ossification of the elbow leading to a limitation of movement. Based on these findings, the mayo elbow performance index (MEPI) [11] was calculated, and the functional outcome was found to be excellent.

The elbow is the second most common dislocated joint in adults. Between 5 and 20% are associated with a fracture, and this combination is often found to complicate recovery. The study of these complex fractures led to the description of the TTE in 1966 by Hotchkiss [1]. During a TTE, energy usually dissipates in a sequential pattern from the lateral to the medial side known as the circle of Horii. Factors that may lead to other associated injuries include the position of the elbow at the time of impact and the severity of injury [12,13]. One such example of a concomitant injury is that seen in our case study, which includes TTE with fracture of the olecranon process. While researching for data relevant to our case, we realized the paucity of literature on variants of TTE. We found a single recent systematic review published in 2021 by Medina et al. from Boston, USA, analyzing the concomitant ipsilateral upper extremity injuries associated with TTE and variants of typical TTE [2]. Although the most common variant was found to be TTE with olecranon fracture (27% of all TTE variants), there are only three papers mentioning this variant. Caviglia et al. emphasized that such associated injuries may go unnoticed if the surgeon is not actively looking for them, as seen in their case, where only an olecranon fracture and elbow subluxation were identified in the right upper limb, and post-operative radiographs discovered radial head and coronoid fractures [3]. This reinforces our opinion of identifying olecranon fracture as a known variant of TTE and including it as a “tetrad” of the elbow so that future misdiagnosis of such complications is avoided. A positive advancement in this direction is the recent classification of elbow fracture-dislocation introduced by Wrightington in June 2021. It focuses on the three-column concept of elbow joint stability and includes TTE with olecranon fracture as type B+. These fractures, like the one seen in our case, are three-column fracture dislocations with poor prognosis. This classification attempts to alleviate the inter- and intra-observer bias and dictate a specific management plan. Type B+ fractures are the most unstable as per this classification. As far as lateral ligament repair or reconstruction is concerned, it should be done after the medial and lateral columns have been restored [14]. In our case, since there was no instability following fixation of bony injuries and no obvious injury visible during surgery, it did not need any repair or reconstruction. However, we had to keep the patient’s elbow immobilized for 3 weeks, and that could have some effect on improving the clinical outcome. It must be mentioned here that the lateral collateral ligament (LCL) contributes between 9 and 14% of varus stability when going from 90° to flexion to full extension [15]. The major stakeholders in the varus stability of the elbow are bony articular surfaces and the anterior capsule. However, considering the Hori cycle of typical TTE, a pre-operative MRI to evaluate the status of LCL should have been done, and had any injury been found, it should have been addressed. Functional outcomes in terrible tetrad can be quite variable, which depends on the severity of injuries and adequacy of treatment. The multiple bony injuries in “terrible tetrad” with or without ligamentous injuries warrant proper surgical planning and execution to achieve a good to excellent functional outcome. All the injuries must be addressed in such a way that early physiotherapy can be started. Timely initiation of ROM exercises will decrease the chances of development of stiffness considerably. Children tolerate immobilization for longer periods compared to adults. This has been seen in the terrible triad variant in a 4.5-year-old female as described by Dailiana et al., where the authors could achieve a good function despite non-rigid fixation but prolonged immobilization. Adults, however, require rigid fixation to initiate early mobilization [5]. Heterotrophic ossification may be encountered in cases where dead necrotic tissue has not been debrided adequately and in cases where the surgical dissection was not meticulous. Our result was far superior compared to the cases reported before. Zha et al. had a MEPI of 80, implying good outcome, and that too in a variant having two of the three components of a triad, indicating less severe injury [4]. Caviglia et al. used DASH as a functional outcome measure and hence cannot be compared to our result directly [3,16]. However, out of their 7 cases, 4 had to be reoperated for issues, such as non-union, residual instability, loosening of prosthesis, etc. They had a fair outcome as per the Broberg and Morrey scale [17]. Although the treatment of the Terrible triad of elbow follows standard protocol, it is difficult to do the same generalization for the “terrible tetrad.” The radial head has to be obviously preserved or replaced depending upon the severity of the injury but cannot be simply excised. Unlike a TTE injury, where the coronoid can be fixed against a stable ulna, in terrible tetrad, olecranon/proximal ulna is also damaged precluding coronoid fixation. Hence, the olecranon should be fixed first and then only the coronoid can be fixed. The stability of the elbow should be assessed intraoperatively. In cases of ligamentous insufficiency, it should either be repaired by suture anchors or reconstructed by tendon graft(s). The above approach is a rough guideline based on available literature and our own experience with the case. The injury must be thoroughly evaluated on an individual basis before surgical intervention. The clinical outcome of our case and any generalization of this treatment modality should be done with caution. We did not adopt any patient-reported outcome measure (PROM) or biomechanical assessment for elbow strength and stability. The follow-up period was of 1½ years. Over a long term, due to the severity of injury and cartilage damage, secondary osteoarthritis, late instability or implant-related complications are possible. There have been very few case reports and hence our modality, which is different from those reported earlier, may not be generalizable in every “Terrible Tetrad”.
A terrible tetrad of elbow seems challenging to manage with a historically dismal prognosis. It is critical to pay close attention to each destabilizing feature of the injury pattern, which places a great demand on the surgeon’s understanding of the anatomy of the elbow. Proper imaging studies, including CT scans and MRIs, should be done for surgical planning. Management of these complicated constellations of injuries requires anatomic fracture fixation of the olecranon and coronoid, radial head fixation or replacement, and ligamentous repair or reconstruction, if any.
A proper clinical and radiological evaluation of each destabilizing injury pattern – whether bony or ligamentous – is essential for proper pre-operative planning. Inadequately managed injuries will invariably give poor results. Hence, all the individual components of the injury must be managed meticulously.
References
- 1.Hotchkiss RN. Fractures and dislocations of the elbow. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD, editors. Rockwood and Green’s Fractures in Adults. 4thed. Philadelphia, PA: Lippincott-Raven; 1996. p. 929-1024. [Google Scholar | PubMed]
- 2.Medina G, Keller RE, Sabbag OD, Oh LS. Terrible triad of the elbow and associated variants: A systematic review. JSES Rev Rep Tech 2022;2:205-13. [Google Scholar | PubMed]
- 3.Caviglia HA, Pemoff AB, Blanchetiere HE, Cuestas NG, Alvarez R, Vergara MS. Fracture-dislocation of the distal elbow complex: is the terrible tetrad a new entity? Rev Latinoam Cirug Ortop 2016;1:14-20. [Google Scholar | PubMed]
- 4.Zha G, Niu X, Yu W, Xiao L. Severe injury of bilateral elbow joints with unilateral terrible triad of the elbow and unilateral suspected terrible triad of the elbow complicated with olecranon fracture: One case report. Int J Clin Exp Med 2015;8:14214-20. [Google Scholar | PubMed]
- 5.Dailiana ZH, Papatheodorou LK, Michalitsis SG, Varitimidis SE. Pediatric terrible triad elbow fracture dislocations: Report of 2 cases. J Hand Surg Am 2013;38:1774-8. [Google Scholar | PubMed]
- 6.O’Driscoll SW. Elbow dislocations. In: Morrey BF, Sanchez-Sotelo J, editors. The Elbow and its Disorders. 4th ed. Philadelphia, PA: Saunders Elsevier; 2009. p. 436-49. [Google Scholar | PubMed]
- 7.Li S, Li X, Lu Y. Analysis of radial head and coronoid process fractures in terrible triad of elbow. Eur J Orthop Surg Traumatol 2019;29:775-84. [Google Scholar | PubMed]
- 8.Chan K, King GJ, Faber KJ. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskelet Med 2016;9:185-9. [Google Scholar | PubMed]
- 9.Ring D, Jupiter JB, Sanders RW, Mast J, Simpson NS. Transolecranon fracture-dislocation of the elbow. J Orthop Trauma 1997;11:545-50. [Google Scholar | PubMed]
- 10.Huh J, Krueger CA, Medvecky MJ, Hsu JR, Skeletal Trauma Research Consortium. Medial elbow exposure for coronoid fractures: FCU-split versus over-the-top. J Orthop Trauma 2013;27:730-4. Erratum in: J Orthop Trauma 2014;28:611. [Google Scholar | PubMed]
- 11.Morrey BF, An KN, Chao EY. Functional evaluation of the elbow. In: Morrey BF, editor. The Elbow and its Disorders. 2nded. Philadelphia, PA: WB Saunders Company Inc.; 1993. p. 95. [Google Scholar | PubMed]
- 12.O’Driscoll SW, Morrey BF, Korinek S, An KN. Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res 1992;280:186-97. [Google Scholar | PubMed]
- 13.O’Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect 2001;50:89-102. [Google Scholar | PubMed]
- 14.Watts AC, Singh J, Elvey M, Hamoodi Z. Current concepts in elbow fracture dislocation. Shoulder Elbow 2021;13:451-8. [Google Scholar | PubMed]
- 15.Phillips BB. Recurrent dislocations. In: Azar FM, Beaty JH, editors, Campbell’s Operative Orthopaedics. 14thed. Philadelphia, PA: Elsevier, Inc.; 2021. p. 2463-78. [Google Scholar | PubMed]
- 16.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The upper extremity collaborative group (UECG). Am J Ind Med 1996;29:602-8. [Google Scholar | PubMed]
- 17.Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am 1986;68:669-74. [Google Scholar | PubMed]









