This case report highlights the evolving understanding and management of Kienbock’s disease, emphasizing the importance of tailored treatment approaches based on disease stage and individual patient factors.
Dr. Shobhana Rajasekar, Department of Hand Surgery, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai - 600 116, Tamil Nadu, India. E-mail: drgowthamanc@gmail.com
Introduction: Kienbock’s disease is an avascular necrosis of the lunate. Although the etiology is not well known, the progression of the disease from ischemia to lunate collapse to arthritis is well documented. In the pre-collapse stages of Kienbock’s disease, procedures for joint leveling, unloading the lunate, and revascularization are performed. The aim was to analyze the usual presentation of patients with Kienbock’s disease clinically and radiologically to assess the ulnar variance, carpal alignment, carpal height preoperatively and postoperatively, and the outcome of the above-mentioned surgical procedure.
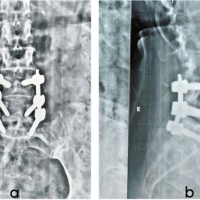
Case Report: Two cases of pre-collapse Kienbock’s disease were operated over a span of 1 year. The above-mentioned objectives were met in different surgical ways. Data recorded were pain scores, range of motion, grip strength, Quick DASH scores, Youm’s index, and scapholunate angle. X-rays were used to record Ulna variance, carpal alignment, and carpal height preoperatively and postoperatively. MRI of the wrist was also done. The mean follow-up was 12 years. The patients had almost complete resolution of pain. The range of dorsiflexion was 25°–40° and the range of palmar flexion was 25°–30°. The mean quick DASH score was significantly reduced. There was a significant improvement in grip strength. All patients had preservation of pre-operative carpal alignment. There was no further collapse of the lunate compared to pre-operative radiographs.
Conclusion: Lunate preservation, decompression, and bone grafting produce satisfactory outcomes. Even though there is a moderate restriction of range of motion at the wrist joint, it produces a painless and stable joint. There is a significant improvement in grip strength which helps patients to do all activities of daily living.
Keywords: Kienbock’s disease, vascularized bone grafting, unloading procedure, capitate osteotomy.
Kienbock’s disease is described as avascular necrosis of the lunate. The etiology remains unknown and controversial [1]. However, it is possible to determine factors that generally impact the risk of incidence. The anatomical risk factors include the shape of the lunate and distal radius, ulnar variance, the coverage of the lunate by radius, the blood supply, excessive intraosseous pressure, and venous stasis [2]. Personal factors include age and gender and the association with osteonecrosis of other carpal bones. Although there is no general agreement regarding radiocarpal anatomy and the development of Kienböck’s disease, there seems to be a relationship between unequal load distribution through the radiocarpal joint whereby the lunate loads an abnormal distribution of the force and the development of lunate osteonecrosis and collapse. This may explain the beneficial effect of joint leveling and decompression procedures, such as radial shortening and capitate shortening, either isolated or accompanied by capito-hamate fusion, in the management of the early stages of the disease [3]. At the earliest stage of Kienbock’s disease, the non-operative and unloading management is generally preferred. Several techniques of capitate shortening osteotomy were described to decompress the lunate in patients with neutral ulnar variance. The technique of capitate shortening was described for the treatment of patients with stage II and IIIA of the disease, and vascularized bone grafting (VBG) of the necrotic lunate has also been described [4-6]. By addressing both of the potential causative factors of the disease, surgical procedures aim to reduce the loading of the lunate and improve the lunate’s vascular supply. Combining revascularization with a joint-leveling procedure for Kienböck’s patients with the ulnar negative wrist has been reported by researchers to yield satisfactory results [7].
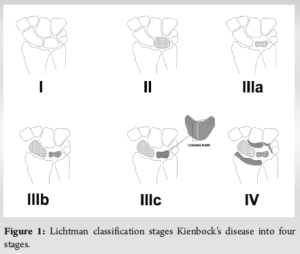
Based on radiographs and MRI, Lichtman classification stages Kienbock’s disease into four stages (Fig. 1).
Stage 1: Normal X-ray, lunate signal intensity changes on MRI.
Stage 2: X-ray – Lunate sclerosis with or without fracture lines. The lunate shape is normal.
Stage 3: Fragmentation of the lunate articular surface and collapse
3A- Lunate has collapsed, but its carpal height remains unchanged.
3B- with flexed and rotated scaphoid and loss of carpal height, proximal migration of capitate.
3C- with an associated coronal lunate fracture.
Stage 4: Stage 3B + radio-carpal or mid-carpal arthrosis (degenerative arthritis)
This study was conducted in the year 2024 in the Department of Hand Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, India. The patients who were diagnosed with pre-collapse stage Kienbock’s disease (Fig. 1 stage 1-3A) and underwent unloading the lunate and revascularization procedure were included. The aim was to analyze the usual presentation of patients with Kienbock’s disease clinically and radiologically by X-rays to assess the ulnar variance, carpal alignment, carpal height preoperatively and postoperatively, and the outcome of the above-mentioned surgical procedure. Retrospectively, data was collected from casesheets consisting of demographic data, history of presenting complaints including pain and swelling along with duration, local examination findings, pain score using Visual Analog Score (VAS), range of motion (ROM) of the affected wrist, grip strength of both the affected and unaffected wrist, Quick disabilities of the arm, shoulder, and hand (DASH) score, Youm index and scapholunate angle, radiological findings including X-ray and MRI of wrist.
Case 1
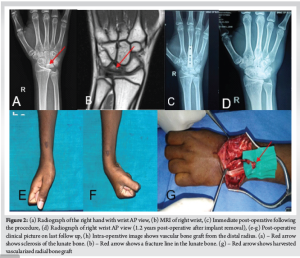

A 15-year-old male who is a kabaddi player with complaints of right dorsal wrist pain, which is insidious in onset and gradually progressive in nature, associated with scapholunate surface tenderness. A plain radiograph of the right wrist showed sclerosis of the lunate bone (Fig. 2A). MRI of the right wrist showed sclerosis of the lunate bone with fracture line, features suggestive of stage II Kienbock’s disease. Minimal effusion was also seen in the ulnar and ventral aspect of the wrist joint (Fig. 2B). Patient underwent right retrograde vascularized metaphyseal radial bone grafting of lunate + capitate resection osteotomy + capito third metacarpal fusion – plating (Fig. 2C). Table 1 summarizes the pre-operative findings of Quick dash score, VAS score, Grip strength of the affected and unaffected side, ROM of affected and unaffected wrist, Youm index and scapholunate angle at the time of presentation and post-operative findings on the last follow up.
Case 2

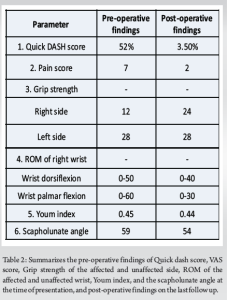
A 30-year-old female with complaints of right wrist pain for 1 year, which is insidious in onset, progressive in nature, and associated with tenderness at the radio lunate facet. A plain radiograph of the right wrist showed sclerosis and flattening of the articular surface in the lunate bone (Fig. 3A). MRI right wrist showed sclerosis, cortical irregularity with fragmentation of lunate articular surface, features suggestive of stage 3A Kienbock’s disease (Fig. 3B). Patient underwent right capitate shortening osteotomy + capitate hamate fusion + vascularized radial bone grafting (based on 4,5 extensor compartment artery) of lunate bone. Table 2 summarizes the pre-operative findings of the Quick dash score, VAS score, Grip strength of the affected and unaffected side, ROM of the affected and unaffected wrist, Youm index, and the scapholunate angle at the time of presentation, and post-operative findings on the last follow up. Both patients were put on a cast for four weeks postoperatively, and suture removal was done on post-operative day 12. Patients following the cast removal were put on a thermoplastic cockup splint. Wrist and finger mobilization exercises and grip strengthening exercises were started. The mean follow-up period was 12 years. Both patients had the right dominant hand involved. Both patients had almost complete resolution of pain and a significant reduction in the Quick DASH score. There was a significant improvement in grip strength, but some restriction of the range of movement at the wrist joint. Patients had preservation of pre-operative carpal alignment. There was no further collapse of the lunate compared to pre-operative X-rays.
Despite the numerous treatments for Kienböck’s disease, no standardized approach exists. In the early stages (Lichtman stages I, II, and IIIA), where carpal alignment remains unchanged, treatment focuses on preserving the lunate’s integrity and carpal kinematics [7]. The primary treatment objectives for stage II include lunate unloading, lunate decompression, and lunate revascularization. Treatment methods should be tailored to each patient with stage II, based on their individual needs [8]. Apart from lunate unloading and lunate decompression, revascularization procedures. Play a vital role in treating stage II. The purpose of distal capitate shortening combined with fusion to the base of the third metacarpal is to relieve pressure on the lunate and prevent the capitate bone from moving proximally. Shortening the capitate will relieve the pressure on the lunate, and fusing the capitate to the third metacarpal base will stop the capitate from moving upward and prevent further collapse of the wrist bones [9]. The theoretical basis for this osteotomy technique is the vascular structure around the capitate bone. Studies have shown that a branch of the anterior interosseous artery supplies blood to the proximal capitate, so it is recommended to perform the osteotomy 2 mm proximal to the distal surface of the capitate [10]. In an anatomical study, significant load reduction on the lunate was evident in all specimens after capitate shortening in cases of neutral ulnar variance. The larger the angle between the capitate and scaphoid, the greater the decrease in pressure [11]. In the early stages, non-operative management is often preferred, especially for patients with negative ulnar variance. However, as the disease progresses to stages III and IV, surgical interventions become necessary. Techniques such as radial shortening osteotomy, capitate shortening osteotomy, and vascularized bone grafting have shown promise in managing the condition [12]. Several studies combined revascularization with additional procedures to unload the lunate, such as capitate shortening osteotomy or radius osteotomy [11,13,14]. Direct vascularization of the lunate can be achieved with a pedicled graft or free vascularized bone graft (VBG) [15]. The most popular VBG technique among American hand surgeons is VBG using the fourth and fifth extensor compartment arteries (ECA) [16]. Daecke et al., in their study of 23 patients with a mean follow-up of 12 years, revealed excellent results from this procedure. In 20 out of 23 patients, there was a significant decrease in pain [5]. In the most recent systematic review, which included 92 VBG-treated patients with Kienbock disease, all subjects achieved improvement in grip strength and pain with no effect on the range of motion [17]. The case studies highlight the usual presentation of patients with Keinbock’s disease, clinically and radiologically, as well as the treatment outcomes. In the first case, a 15-year-old male kabaddi player with stage II Kienböck’s disease underwent a combination of vascularized bone grafting and distal capitate resection osteotomy with capito-third metacarpal fusion, resulting in significant pain relief and improved grip strength. The patient, who was not able to play Kabaddi because of his pain, went back to his sports activity following surgery and rehabilitation with hand therapy. Similarly, a 30-year-old female homemaker with stage IIIA disease who was not able to do her daily household activities and kitchen chores showed marked improvement following capitate shortening osteotomy with capito-hamate fusion and vascularized bone grafting and was able to resume all her activities. These findings show the competence of the surgical treatment plan of unloading the lunate bone and revascularization procedure in alleviating the pain and producing stable and painless joints with improved grip strength. Further research is needed to refine these surgical techniques and explore new therapeutic options to improve outcomes with respect to the range of motion in affected wrist joints of patients with Kienböck’s disease. This study had a few limitations: first, it was a retrospective study, and second, it was a small sample size study. This study didn’t achieve adequate power for statistical analysis. A prospective study with a bigger sample size can yield more concrete conclusions.
Lunate preservation, unloading, and bone grafting produce satisfactory outcomes. Even though there is a moderate restriction of motion at the wrist joint, there is a significant improvement in grip strength. These procedures resulted in painless, stable joints which helped patients to do all activities of daily living.
Effective management of Kienbock’s disease requires a stage-specific, individualized approach. Early stages may benefit from non-operative treatment, whereas advanced stages often need surgical intervention such as capitate shortening osteotomy and vascularized bone grafting to reduce lunate load and enhance revascularization. Personalizing treatment based on anatomical and patient-specific factors can significantly improve pain relief and wrist function. Further research is essential to refine surgical techniques and explore innovative therapies for better long-term outcomes.
References
- 1.Chojnowski K, Opiełka M, Piotrowicz M, Sobocki BK, Napora J, Dąbrowski F, et al. Recent advances in assessment and treatment in Kienböck’s disease. J Clin Med 2022;11:664. [Google Scholar | PubMed]
- 2.Fontaine C. Kienböck’s disease. Chir Main 2015;34:4-17. [Google Scholar | PubMed]
- 3.Al-Ashhab M, Farag H. Kienböck’s diseases treatment. A novel technique via distal capitate shortening accompanied by 3rd metacarpal base fusion in neutral variance ulna. Benha Med J 2021;38:22-33. [Google Scholar | PubMed]
- 4.Hegazy G, Seddik M, Massoud AH, Imam R, Alshal E, Zayed E, et al. Capitate shortening osteotomy with or without vascularized bone grafting for the treatment of early stages of Kienböck’s disease. Int Orthop 2021;45:2635-41. [Google Scholar | PubMed]
- 5.Daecke W, Lorenz S, Wieloch P, Jung M, Martini AK. Vascularized os pisiform for reinforcement of the lunate in Kienböck’s disease: An average of 12 years of follow-up study. J Hand Surg Am 2005;30:915-22. [Google Scholar | PubMed]
- 6.Delaere O, Dury M, Molderez A, Foucher G. Conservative versus operative treatment for Kienböck’s disease. A retrospective study. J Hand Surg Br 1998;23:33-6. [Google Scholar | PubMed]
- 7.Waitayawinyu T, Chin SH, Luria S, Trumble TE. Capitate shortening osteotomy with vascularized bone grafting for the treatment of Kienböck’s disease in the ulnar positive wrist. J Hand Surg 2008;33:1267-73. [Google Scholar | PubMed]
- 8.Beredjiklian PK. Kienböck’s disease. J Hand Surg Am 2009;34:167-75. [Google Scholar | PubMed]
- 9.Fouly EH, Sadek AF, Amin MF. Distal capitate shortening with capitometacarpal fusion for management of the early stages of Kienböck’s disease with neutral ulnar variance: Case series. J Orthop Surg Res 2014;9:86. [Google Scholar | PubMed]
- 10.Li J, Pan Z, Zhao Y, Hu X, Zhao X. Capitate osteotomy and transposition for type III Kienböck’s disease. J Hand Surg Eur Vol 2018;43:708-11. [Google Scholar | PubMed]
- 11.Quenzer DE, Dobyns JH, Linscheid RL, Trail IA, Vidal MA. Radial recession osteotomy for Kienböck’s disease. J Hand Surg 1997;22:386-95. [Google Scholar | PubMed]
- 12.Nakagawa M, Omokawa S, Kira T, Kawamura K, Tanaka Y. Vascularized bone grafts from the dorsal wrist for the treatment of Kienböck disease. J Wrist Surg 2016;5:98-104. [Google Scholar | PubMed]
- 13.Werber KD, Schmelz R, Peimer CA, Wagenpfeil S, Machens HG, Lohmeyer JA. Biomechanical effect of isolated capitate shortening in Kienböck’s disease: An anatomical study. J Hand Surg Eur Vol 2013;38:500-7. [Google Scholar | PubMed]
- 14.Moran SL, Cooney WP, Berger RA, Bishop AT, Shin AY. The use of the 4 + 5 extensor compartmental vascularized bone graft for the treatment of Kienböck’s disease. J Hand Surg Am 2005;30:50-8. [Google Scholar | PubMed]
- 15.Schmitt R, Heinze A, Fellner F, Obletter N, Strühn R, Bautz W. Imaging and staging of avascular osteonecroses at the wrist and hand. Eur J Radiol 1997;25:92-103. [Google Scholar | PubMed]
- 16.Kolovich GP, Kalu CM, Ruff ME. Current trends in treatment of Kienböck disease: A survey of hand surgeons. Hand (N Y) 2016;11:113-8. [Google Scholar | PubMed]
- 17.Tsantes AG, Papadopoulos DV, Gelalis ID, Vekris MD, Pakos EE, Korompilias AV. The efficacy of vascularized bone grafts in the treatment of scaphoid nonunions and Kienbock disease: A systematic review in 917 patients. J Hand Microsurg 2019;11:6-13. [Google Scholar | PubMed]