For a case of advanced knee OA with patellar non-union after ORIF, simultaneous TKA and revision ORIF with bone grafting using resected bone from TKA offered a less invasive treatment.
Masaki Nagashima, Department of Orthopaedic Surgery, International University of Health and Welfare Mita Hospital, 1-4-3 Mita, Minato-ku, Tokyo 108-8329, Japan. E-mail: masakin@iuhw.ac.jp
Introduction: Treatment of advanced knee osteoarthritis (OA) with periarticular fractures is challenging, particularly when accompanied by non-union of patellar fractures. In the elderly, multiple surgeries pose disadvantages because they increase the anesthetic risk and the incidence of perioperative complications and prolong the time required for functional recovery. We report a case of advanced knee OA with non-union of a patellar fracture after open reduction and internal fixation (ORIF) that was treated with one-stage total knee arthroplasty (TKA) together with bone grafting.
Case Report: An 85-year-old female with advanced OA of the left knee presented with the treatment of non-union of a left patellar fracture following ORIF. Conservative treatment using low-intensity pulsed ultrasound and teriparatide for 1 year proved ineffective, prompting us to perform simultaneous TKA and ORIF of the patellar non-union. One year postoperatively, the patient achieved a favorable outcome.
Conclusion: We performed simultaneous left TKA and ORIF with bone grafting in a patient with knee OA and non-union of a patellar fracture. This procedure allowed the bone resected during TKA to be used for bone grafting at the pseudarthrosis site.
Keywords: Total knee arthroplasty, Non-union of patellar fracture, Single-stage fixation
Total knee arthroplasty (TKA) is a well-established treatment for advanced knee osteoarthritis (OA), and the surgical procedures are well-established. However, treatment of advanced knee OA with periarticular fractures can be challenging, particularly when accompanied by non-union of a patellar fracture, which is part of the extensor mechanism. The significant strain on the extensor mechanism, including the patella, during TKA procedures and rehabilitation is a major concern. In a patient with OA of the knee and patellar fracture or its non-union, it may be safe to conduct open reduction and internal fixation (ORIF) of the fracture as a first step and perform TKA after bony fusion is achieved, rather than treating the fracture and performing TKA simultaneously. However, undergoing multiple surgeries has the disadvantage of increasing the risk of anesthesia and perioperative complications, especially in the elderly, in addition to prolonging functional recovery [1-3]. A literature review revealed several case reports of simultaneous ORIF of patellar fracture and TKA [1-4]. However, no paper has reported a case of advanced knee OA with patellar non-union after ORIF that was treated with simultaneous TKA and ORIF of the patellar non-union. Furthermore, this method would have the advantage that the resected bone during TKA can be grafted at the patellar non-union site, but has not been previously reported. Here, we report a case of advanced knee OA with non-union of patellar fracture after ORIF that was treated with TKA and simultaneous ORIF with bone grafting.
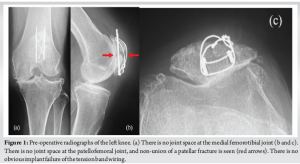
An 85-year-old female visited our hospital complaining of left knee pain. She had undergone ORIF with tension band wiring (TBW) for a left patellar fracture 7 months previously at a different hospital. However, bone union of the patellar fracture had not been achieved and the left knee pain persisted. She had a history of right patellar fracture and fractures of both ankles. Her body mass index was 25.6 kg/m2 (height, 157 cm; weight, 63.0 kg). Because of the left knee pain, she needed support for walking indoors and used a wheelchair outdoors. On physical examination, the range of motion (ROM) of the left knee was 0–120°. The pain was present at the medial joint space and around the patella, where it was particularly severe, with a Numerical Rating Scale (NRS; 0–10) of 8. Both of these areas were tender on palpation. No ligamentous instability was observed. Her Knee Society (KS) knee score was 53, and her KS function score was 40. Bone mineral density of the lumbar spine and proximal femur were 1.305 g/cm² and 0.678 g/cm², respectively. Radiographs of the left knee showed non-union of the patellar fracture, no joint space at the patellofemoral or medial femorotibial joints, and evidence of OA at the level of Kellgren–Lawrence classification stage IV at both of these sites (Fig. 1). Computed tomography (CT) of the left knee also showed non-union at the middle of the patella (Fig. 2). The femorotibial angle was 179°. There was no obvious implant failure of TBW. The diagnosis was severe knee OA with patellar non-union after a previous ORIF. As treatment for the patellar non-union and bone fragility, we initially treated the patient with low-intensity pulsed ultrasound (LIPUS) (Exogen Ultrasound Bone Healing System; Bioventus, Durham, NC) and teriparatide injection (Teribone; Asahi Kasei Pharma, Tokyo, Japan). LIPUS (1.5 MHz) was applied to the affected area for 15 min every day. As there was insufficient improvement in both the subjective symptoms and imaging findings in the left knee after 1 year of treatment, we decided to perform TKA and surgery for non-union of the patella in a one-stage procedure.

Surgical procedure
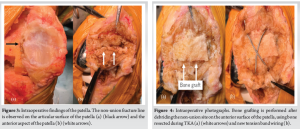
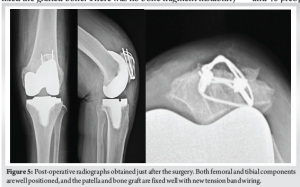
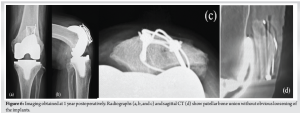
Surgery was performed under general anesthesia with a tourniquet. The previous skin incision was used and extended, and a medial parapatellar arthrotomy was performed. First, the femoral and tibial implants were replaced. An Attune knee system (DePuy Synthes, Warsaw, IN) with a fixed-bearing posterior cruciate-stabilizing prosthesis was used. The surgical epicondylar axis was used as the index for the rotation of the femoral component, and the Akagi line for the rotation of the tibial component. The cartilage of the patellofemoral joint was completely absent. The non-union fracture line was observed on the articular surface of the patella (Fig. 3). Next, surgery for non-union of the patella was performed. We removed the surgical wires of TBW, leaving the straight steel wires in place, and debrided the pseudarthrosis on the anterior surface of the patella using a Surgairtome. The debrided area of the pseudarthrosis was 10 × 20 mm. We transplanted autograft bone obtained from the TKA resection into this defect and performed a new TBW (AI-Wiring System; Aimedec MMT, Tokyo, Japan) (Fig. 4). The surgical wire used in the TBW firmly fixed the grafted bone. There was no bone fragment instability of the treated patellar non-union through 90° of knee flexion, and patellar tracking was acceptable. We decided not to perform patellar replacement because of concerns about bone loss due to OA and instability around the patellar non-union, even after the ORIF with bone grafting. To prevent ischemia of the patella, we also did not perform lateral release or lateral patellar facetectomy [5] (Fig. 5). Postoperatively, full weight-bearing walking was started 1 day after surgery. Knee immobilization with a brace was applied for 1 week. From the 2nd to 3rd week, the range of flexion gradually increased to 90°. After 3 post-operative weeks, the patient was allowed full ROM. At the 1-year follow-up, the patient was able to walk with a cane and the ROM of the left knee was 0–125° (0–120° preoperative). Her left knee pain decreased to 1 (8 preoperative) on the NRS. Patellar bone union was observed without obvious loosening of the implants (Fig. 6), and the KS knee score and function score had improved to 89 and 65 (53 and 40 preoperative), respectively. At the 2-year follow-up, her left knee pain was 0 on the NRS, and the KS knee score and function score were maintained.
Treatment of advanced knee OA complicated by periarticular fractures is challenging and can be associated with various complications [6]. It is well known that fractures of the distal femur and proximal tibial adversely affect outcomes of TKA. In addition, previous studies have shown that TKA following fracture fixation around the knee is associated with a significantly higher risk of post-operative infection [7]. Regarding the patella, Houdek et al. [8] reported the effects of a previous patellar fracture on the outcome of TKA. They found that a previous fracture of the patella had no significant impact on the overall revision-free survival of TKA. However, compared to TKA without a previous patellar fracture, TKA with a previous patellar fracture was significantly associated with a higher rate of manipulation under anesthesia, limited ROM, and arthrofibrosis in the long term. Achieving bony union and restoring the extensor mechanism are key objectives in managing patellar fractures. In addition, the functional extensor mechanism of the knee is crucial for TKA. When a patellar fracture or non-union is present in a patient with advanced OA, it is controversial whether treatment of the patella should be the first step with TKA conducted after bony fusion has been achieved, or if a one-stage procedure should be undertaken. There are only a few case reports of simultaneous ORIF of patellar fracture and TKA [1,2,3,4], all of which obtained favorable results. However, all of the fractures in these studies were either fresh or untreated, and there were no reports of non-union of a patellar fracture after ORIF. Here, we report the first case of advanced knee OA with non-union of patellar fracture after ORIF, in which a good outcome was obtained after simultaneous TKA and ORIF with bone grafting. While a staged approach, performing ORIF for the patella fracture followed by TKA after achieving union, is commonly recommended, it has several limitations. First, it requires two separate surgeries, increasing the total anesthetic exposure and surgical burden. In elderly patients, prolonged treatment courses and repeated hospitalization can increase the risk of systemic complications and delay overall functional recovery. In contrast, a one-stage procedure eliminates the need for a second surgery and allows for earlier mobilization. This approach reduces the cumulative rehabilitation time and may improve quality of life, especially in frail patients. Nonetheless, simultaneous surgery requires careful intraoperative fixation to ensure adequate stability of the patella, allowing safe and effective post-operative rehabilitation. The incidence of non-union or delayed union of patellar fracture is reported to be 2.7–12.5% [9]. The risk factors for the development of non-union or delayed union are not clearly defined. However, open fractures, transverse fractures with large displacement, and improper immobilization during conservative fracture management appear to have higher risk [9]. Regarding conservative treatment of non-union of the patella, LIPUS is an option, and its efficacy has been shown by Bashardoust et al. [10]. In addition, several studies have reported the effects of teriparatide for the treatment of non-union, in addition to its effect on increasing bone mineral density for patients with osteoporosis [11]. Therefore, we administered teriparatide with the expectation of its effects on the non-union. In this case, the history of multiple previous fractures suggested bone fragility, and even without non-union of the patella, teriparatide would have been indicated. Various surgical techniques have been described for the treatment of displaced patellar fractures, among which TBW is a good option as it enables early knee mobilization [2,3]. Alternatively, some reports have suggested the use of a non-absorbable polyester suture, such as FiberWire (Arthrex, Naples, FL), and fiber tapes instead of hardware. These may be preferable for avoiding complications related to hardware, which include pain from protruding pins, the need for removal of the implant, and infection [3,4]. Although surgery for patellar non-union included TBW, cerclage wiring, and screw fixation, TBW was reported to be the predominant modality [9]. A recent case series of patellar non-union reported that bone grafting was performed in patients with non-articular bone defects and that TBW achieved the best results overall. In addition, they described that the need for bone grafting should be assessed intraoperatively on a case-by-case basis [12]. In the present case, pre-operative imaging revealed bone defects at the non-union site, and we thus considered that bone grafting was necessary. A new TBW was performed because strong fixation between the non-union site and the bone graft was needed, as previous TBW bone holes were already present. We could also effectively utilize bone that had been resected during TKA for the subsequent bone grafting. This method is less invasive for the patient as it does not require harvesting bone from other sites. A limitation of the procedure is that patellar resurfacing is difficult even in the presence of cartilage defects in the patella. This is because additional bone loss can occur in the case of non-union of the patella, which requires continued careful monitoring of patellofemoral arthritis in the future. If patellar tracking is poor, lateral release and/or lateral patellar facetectomy is required. However, if lateral release were performed in the present patient, we would expect impairment of blood flow to the patella from the lateral side, which would have a negative effect on bone fusion and may also be a risk for the development of avascular necrosis of the patella [13]. Lateral patellar facetectomy [5] may also affect bone healing because of the additional bone loss. Care is needed in the rotational placement of the femoral and tibial components to obtain good patellar tracking, which in the present patient resulted in satisfactory patellar tracking without lateral release or lateral patellar facetectomy.
The present case of knee OA with patellar non-union after previous ORIF was treated with simultaneous TKA and ORIF with bone grafting, and a favorable outcome was obtained. This procedure allows bone resected during TKA to be used for bone grafting at the pseudarthrosis site. We consider that this option is particularly useful in elderly patients, as it avoids multiple surgeries and the morbidity associated with bone harvesting from another site.
This is the first report of simultaneous TKA and ORIF with bone grafting for the treatment of advanced knee OA with patellar non-union after previous ORIF. This procedure enables the bone resected during TKA to be used for bone grafting and does not require harvesting graft bone from other sites. It is, therefore, less invasive for the patient and can help avoid complications associated with multiple surgeries.
References
- 1.Rao SS, Sonawane CS, Wakankar HM, Kulkarni MM. Knee osteoarthritis with old untreated patella fracture treated with single stage total knee arthroplasty - a case series of two cases. J Orthop Case Rep 2022;12:75-8. [Google Scholar | PubMed]
- 2.Surendran S, Pengatteeri YH, Park SE, Gopinathan P, Chang JD, Han CW. Osteoarthritis knee with patellar fracture in the elderly: Single-stage fixation and total knee arthroplasty. J Arthroplasty 2007;22:1070-3. [Google Scholar | PubMed]
- 3.Patel KH, Reddy AV, Eachempati K, Muralidhar S, Jungele A. A patient with osteoarthritis knee and prior patella fracture: Single stage fixation and total knee arthroplasty: A case report. J Orthop Case Rep 2018;8:67-70. [Google Scholar | PubMed]
- 4.Tomar L, Govil G, Gupta N. Management of a complex extensor mechanism injury in a rheumatoid knee- a case report with literature review. J Orthop Rep 2023;2:100221. [Google Scholar | PubMed]
- 5.Nagashima M, Otani T, Harato K, Sasaki R, Seki H, Takeshima K, et al. Lateral patellar facetectomy reduces the incidence of anterior knee pain in patellar resurfaced total knee arthroplasty. J Knee Surg 2023;36:773-8. [Google Scholar | PubMed]
- 6.McCormick BP, Sequeira SB, Hasenauer MD, McKinstry RP, Ebert FR, Boucher HR. Outcomes after total knee arthroplasty in patients with a history of patella fracture: A propensity score-matched analysis. J Am Acad Orthop Surg Glob Res Rev 2024;8:e24.00007. [Google Scholar | PubMed]
- 7.Suzuki G, Saito S, Ishii T, Motojima S, Tokuhashi Y, Ryu J. Previous fracture surgery is a major risk factor of infection after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2011;19:2040-4. [Google Scholar | PubMed]
- 8.Houdek MT, Shannon SF, Watts CD, Wagner ER, Sems SA, Sierra RJ. Patella fractures prior to total knee arthroplasty: Worse outcomes but equivalent survivorship. J Arthroplasty 2015;30:2167-9. [Google Scholar | PubMed]
- 9.Nathan ST, Fisher BE, Roberts CS, Giannoudis PV. The management of nonunion and delayed union of patella fractures: A systematic review of the literature. Int Orthop 2011;35:791-5. [Google Scholar | PubMed]
- 10.Bashardoust Tajali S, Houghton P, MacDermid JC, Grewal R. Effects of low-intensity pulsed ultrasound therapy on fracture healing: A systematic review and meta-analysis. Am J Phys Med Rehabil 2012;91:349-67. [Google Scholar | PubMed]
- 11.Puvvada CS, Soomro FH, Osman HA, Haridi M, Gonzalez NA, Dayo SM, et al. Efficacy and safety of teriparatide in improving fracture healing and callus formation: A systematic review. Cureus 2023;15:e37478. [Google Scholar | PubMed]
- 12.Harna B, Gupta P, Singh J, Rousa S, Gupta A. Surgical management of non-union patella fracture: A case series and review of the literature. Arch Bone Jt Surg 2021;9:554-8. [Google Scholar | PubMed]
- 13.Bourke MG, Sclavos EK, Jull GA, Buttrum PJ, Dalton PA, Russell TG. A comparison of patellar vascularity between the medial parapatellar and subvastus approaches in total knee arthroplasty. J Arthroplasty 2012;27:1123-7.e1. [Google Scholar | PubMed]