Limb hypertrophy associated with syndromes can lead to biomechanical instability and ligament injuries.
Dr. Anand Raj Rajendrababu, Department of Orthopaedics, Government Medical College Kannur, Kerala, India. E-mail: dranandrajr@gmail.com
Introduction: Klippel–Trenaunay syndrome is a rare congenital disorder. Injuries involving the posterior cruciate ligament (PCL) may occur independently following trauma. We’re reporting this rarest combination, the first case reported in literature, where these two conditions occur in the same limb.
Case Report: We present a 23-year-old male with sports injury to the right knee 3 years back who was diagnosed with PCL injury clinicoradiologically. Port wine stain, limb hypertrophy, and varicose veins were noticed in the affected limb and were diagnosed as Klippel–Trenaunay syndrome. He underwent arthroscopic PCL reconstruction.
Conclusion: There is limited direct evidence of PCL injuries specifically in Klippel–Trenaunay patients, but given the limb overgrowth and potential instability associated with the syndrome, knee injuries such as PCL tears may be more likely.
Keywords: Posterior cruciate ligament, Klippel–Trenaunay syndrome, arthroscopic reconstruction.
Klippel–Trenaunay syndrome (KTS) is a rare congenital condition characterized by vascular malformations (port-wine stain), limb hypertrophy, and varicose veins [1]. Injuries involving the posterior cruciate ligament (PCL), however, are typically related to sports or trauma and may occur independently of the syndrome [2]. In individuals with KTS, orthopaedic issues are common due to limb size discrepancies, venous abnormalities, and potential bone overgrowth. This overgrowth can lead to limb length discrepancies, scoliosis, and difficulty with mobility. A possible association between mild limb length discrepancy (>5 mm) and anterior cruciate ligament (ACL) injuries in the shorter leg, especially in active, growing athletes, has been reported [3]. However, no correlation has been so far reported linking limb length discrepancy and PCL injuries in the literature. We are reporting a 2-year follow-up of a rare case of a young male with PCL rupture with KTS affecting the same limb.
A 23-year-old male with no known comorbidities presented with complaints of pain, swelling, and instability over the right knee following twisting injury while playing football 3 years back. On examination of the knee, there was no healed scar suggestive of any external injury. There was minimal swelling of the right knee and varicose veins all over the right lower limb. The right lower limb was found to be 1 cm longer than the left, accounted by 0.5 cm in the femur and 0.5 cm in tibia. The bulk of the thigh and leg was larger by 1.5 cm on the right side compared to the left side (Fig. 1 is self-explanatory). There was a port-wine stain over the lateral aspect of the right thigh (Fig. 2). He did not have any features suggestive of ligamentous laxity. The knee range of movement was full. Posterior sag sign was present. The posterior drawer test was positive. Varus and Valgus stress tests were negative. The McMurray test for both menisci was negative. Dial test and pivot shift test were negative. Tests for ACL insufficiency were negative. X-ray standing anterior–posterior (Fig. 3), 45° flexion, weight bearing, and merchant patellar views were taken with contralateral view for comparison. This showed a positive sag compared to the contralateral knee.

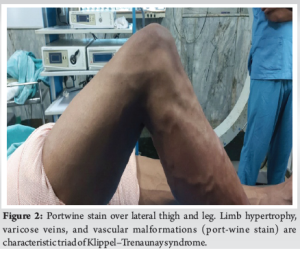
Magnetic resonance imaging of the right knee was taken, which showed altered marrow edema within both condyles of femur and tibia, suggestive of marrow contusion. Complete rupture of PCL (Fig. 4) and focal radial tear of the posterior horn of medial meniscus at the periphery. Also showed a moderate knee joint effusion with a small Baker’s cyst. Doppler study of the right lower limb was done, which showed multiple incompetent perforators in the leg. There was no evidence of deep vein thrombosis. An ultrasound study of the abdomen was done to rule out abnormalities in the abdomen or pelvis. Systemic examination of the cardiovascular system and other systems did not reveal any abnormalities. Based on the clinical triad, diagnosis of KTS was made.
Altered kinematics leading to femoro-tibial arthrosis in a PCL-deficient knee support operative management. Due to the chronicity of the injury and as the patient was persistently symptomatic with the PCL deficient knee, he underwent Arthroscopic PCL reconstruction with quadrupled hamstring graft (semitendinosis and gracilis) under general anaesthesia using tibial tunnel technique with fluoroscopic and arthroscopic guidance (Fig. 5). Skin incisions were marked before inflation of the tourniquet to avoid injury to the enlarged tortuous veins. Meniscal lesions were found to be healed. Immediate post-operative period was uneventful and he was started on regular physiotherapy. He was started on isometric quadriceps strengthening exercises, knee range of motion in prone position, weight-bearing mobilization with walker support, and active toe and ankle movements during the 1st month postoperatively, and regular physical therapy protocols were followed thereafter. Limb length discrepancy is addressed by heel rise footwear modification to prevent any recurrence. Two years postoperatively, he is asymptomatic and is actively involved in sports activities.
PCL is one of the four major ligaments of the knee joint that function to stabilize the tibia on the femur, originating from the anterolateral aspect of medial femoral condyle and inserting into the posterior aspect of tibial plateau. It prevents the posterior translation of tibia on femur [4-6]. The previous studies have reported an incidence between 1 and 47% for PCL injuries in acute knee ligament injuries [7-9]. Klippel–Trenaunay–Weber syndrome is associated with soft tissue and osseous hypertrophy, cutaneous hemangiomas, and vascular malformations. Varicose veins, cutaneous hemangiomas, and hypertrophy of soft tissue and bone are commonly used diagnostic criteria [5]. Its incidence is 1 in 30,000 live births. There is limited direct evidence of PCL injuries specifically in KTS patients, but given the limb overgrowth and potential instability associated with the syndrome, knee injuries such as PCL tears may be more likely. For instance, hypertrophy of the affected limb can lead to abnormal biomechanics and joint instability, increasing the risk of PCL injuries. A limited volume of data from the existing literature estimates the rate of short- to mid-term surgical failure after primary isolated PCL-R to be as frequent as 3–12.6% [4,7,10], but no consistent data of recurrence is available in current literature regarding the injury in KTS patients. In addition, the venous and vascular malformations associated with KTS may complicate surgical repair or post-injury rehabilitation due to an increased risk of bleeding or thrombosis [1].
KTS is a rare condition. We present this case to showcase this rarest combination occurring in the same limb. Further studies maybe conducted to correlate between KTS, limb length discrepancy, and PCL injuries.
Limb length discrepancy can lead to abnormal biomechanics and joint instability increasing the risk of PCL injuries. Adequate footwear modifications to correct limb length discrepancy and structured rehab protocols may be initiated in these patients to prevent these injuries and their recurrence.
References
- 1.Shakir DK, Arafa SO. Klippel-Trenaunay syndrome-case report and review of the literature. Int J Angiol 2005;14:147-50. [Google Scholar | PubMed]
- 2.Raj MA, Mabrouk A, Varacallo M. Posterior cruciate ligament knee injuries. In: StatPearls. Treasure Island, FL: StatPearls; 2023. [Google Scholar | PubMed]
- 3.Lazaro LE, van der List JP, Cordasco FA, Green DW. Is pre-injury leg length discrepancy a risk factor for anterior cruciate ligament injury in the skeletally immature athlete? Orthop J Sports Med 2017 Jul 31;5(7 suppl6) [Google Scholar | PubMed]
- 4.Freychet B, Desai VS, Sanders TL, Kennedy NI, Krych AJ, Stuart MJ, et al. All-inside posterior cruciate ligament reconstruction: Surgical technique and outcome. Clin Sports Med 2019;38:285-95. [Google Scholar | PubMed]
- 5.Zacharia B, Alex J, Rajmohan A. Klippel-Trénaunay syndrome and developmental coxa vara in the same limb: A case report with a review of the literature. Int J Angiol 2023;32:292-5. [Google Scholar | PubMed]
- 6.LaPrade RF, Floyd ER, Falaas KL, Ebert NJ, Struyk GD, Carlson GB, et al. The posterior cruciate ligament: Anatomy, biomechanics, and double-bundle reconstruction. J Arthrosc Surg Sports Med 2021;2(2):94-107. [Google Scholar | PubMed]
- 7.Marom N, Ruzbarsky JJ, Boyle C, Marx RG. Complications in posterior cruciate ligament injuries and related surgery. Sports Med Arthrosc Rev 2020;28:30-3. [Google Scholar | PubMed]
- 8.Keller PM, Shelbourne KD, McCarroll JR, Rettig AC. Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med 1993;21:132-6. [Google Scholar | PubMed]
- 9.Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg 2003;123:186-91. [Google Scholar | PubMed]
- 10.Sekiya JK, West RV, Ong BC, Irrgang JJ, Fu FH, Harner CD. Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy 2005;21:1042-50. [Google Scholar | PubMed]