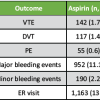
This case report provides an insight into the management of chronic locked posterior dislocation of shoulder with a large humeral head defect in a young adult managed by the Modified Mclaughlin procedure.
Dr. Naman K. Parakh, Assistant Professor, Department of Orthopedics, Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India namanparakh1604@gmail.com
Introduction: Chronic locked posterior dislocation (CLPD) of the shoulder presents a big challenge to the orthopedic surgeon due to the progressive damage to the glenohumeral articulation and increase in size of the reverse Hill-Sachs lesion (RHSL). Multiple treatment strategies have been postulated depending upon the size of the humeral head defect and the RHSL.
Case Report: A 35-year-old Indian male patient presented to our Outpatient Department with complaints of pain and restriction in the range of motion over the right shoulder since suffering an injury over the shoulder 6 months back. Clinical examination revealed a bony restriction particularly in external rotation, flexion, and abduction of the right shoulder. The radiographs were suggestive of CLPD of the right shoulder with a large sized humeral head defect. An magnetic resonance imaging of the right shoulder was done to quantify the defect and reveal the anatomical status of the shoulder joint. After proper planning and workup, the patient was managed surgically with the modified McLaughlin procedure. Proper rehabilitation and regular follow-ups were done and the patient showed significant functional improvement of the right shoulder at 2-year follow-up.
Conclusion: The treatment of CLPD varies according to the size of the humeral head defect and the functional demand of the patient. The modified McLaughlin procedure is an excellent option in mild to moderate-sized defects. The results of the procedure are also affected by the delay in treatment since the time of injury.
Keywords: Chronic locked posterior dislocation, reverse Hill-Sachs lesion, modified McLaughlin procedure.
Posterior shoulder dislocations are relatively rare in occurrence and may lead to impression fractures or defects over the humeral head. This later leads to recurrent or chronic instability over the affected shoulder, thereby causing movement restriction, joint destruction, and osteoarthritis [1]. These lead to defects on the anteromedial part of the humeral head, also known as reverse Hill-Sachs lesions (RHSL) [2]. Management of these cases can be done conservatively if presenting early in the acute stages. If untreated, they lead to chronic locked posterior dislocation of the shoulder wherein the humeral head gets locked posteriorly in the glenoid at the level of the defect. This causes progressive joint destruction, increase in defect size, and severe restriction of shoulder movements [3]. Chronic, neglected cases warrant surgical intervention which could be anatomical or non-anatomical. The former focuses on restoring the native humeral head shape, whereas the latter focuses on restoring stability of the shoulder [4]. The choice of surgical procedure depends on factors such as the time from injury, size of RHSL, functional requirement, and the associated injuries or fractures, if any [1]. The Neer and Hawkins modification of the McLaughlin procedure (modified McLaughlin procedure) is the surgery of choice in RHSL of size 20–45% of the humeral head. The procedure involves the transfer of the lesser tuberosity (LT) along with the subscapularis tendon into the humeral head defect [2]. This case report highlights the effectiveness of this procedure and its functional outcomes in a CLPD patient.
A 35-year-old male patient arrived at the outpatient department with complaints of severe restriction in shoulder movement since suffering a fall on the right shoulder after an episode of seizure 6 months back. The patient did not have any episode of seizure before or after the incident. He had also visited multiple doctors for the complaints but no clinical improvement was obtained. Clinical examination revealed a loss of normal shoulder contour, a prominent coracoid process, and severe wasting of the muscles around the right shoulder. The right upper limb was in internal rotation at the shoulder with a bony restriction in external rotation, flexion, and abduction movements. An anteroposterior and axillary view of the right shoulder was advised.
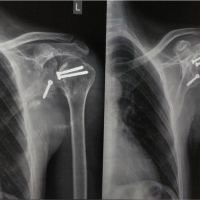
Radiographic findings showed:
- Typical light bulb sign of the humeral head denoting posterior dislocation of the shoulder
- Loss of normal humeral head shape and anatomy
- RHSL which was roughly one-third of the size of the humeral head
- Reduced acromio-humeral distance (Fig. 1a and b).

We confirmed the diagnosis of CLPD of the right shoulder. We scheduled a computed tomography (CT) scan of the right shoulder to further quantify the humeral head defect by the method described by Gerber et al. and Moroder et al. and explore the glenohumeral anatomy more extensively [5,6].
The RHSL size was measured to be 39%, whereas the alpha angle was also calculated which was 62° (Fig. 2a and b).

The modified McLaughlin procedure was chosen as the treatment option after considering the size of the RHSL, the duration since injury and the degree of instability over the right shoulder.
After routine pre-operative workup, the patient was posted for surgical intervention. The surgery was done in a beach chair position under general anesthesia and the shoulder was exposed using the deltopectoral approach. The arm was externally rotated and the lower margin of subscapularis tendon was identified and tagged using non-absorbable sutures. The LT was osteotomized along with subscapularis tendon in a lateral to medial fashion. The glenohumeral joint was exposed and the soft tissue adhesions between the posterior glenoid and humeral head were released carefully while simultaneous external rotation of the shoulder. A Cobb elevator was used to carefully reduce the joint to prevent any further damage to the humeral head and glenoid while laterally distracting and externally rotating the shoulder. All bony and cartilaginous debris were removed from the joint and the joint was thoroughly irrigated. The size of the humeral head defect was evaluated and freshened using curette to prepare the bed for LT transfer. A tricortical autograft of appropriate size was harvested from the ipsilateral iliac crest to additionally fill the defect and augment the anatomical restoration. The LT fragment with subscapularis was secured using 2.5 mm double-loaded metal suture anchors into the humeral head defect. The graft was then placed between the LT and defect and secured using 2.4 mm cannulated cancellous screws. The fixation was secured and the stability of reduction was checked across all movements of the shoulder under direct vision. The position of the joint and the fixation was further checked using an image intensifier. The operative time was 80 min. Post-operative antibiotic prophylaxis was administered, and the limb was kept in a shoulder abduction brace for 6 weeks, not allowing internal rotation of the shoulder. Gentle passive, active assisted exercises were progressively started, and full active movements were allowed only after 12 weeks of surgery. The patient was followed up clinico-radiologically at monthly intervals and achieved complete restoration of shoulder function after 12 months of surgery (Fig. 3 and 4).


The difficulty and delay in the diagnosis of posterior shoulder dislocations lead to profound damage to the glenohumeral articulation. Chronic lateralized periodic discharges are cases where the delay in diagnosis is more than 6 weeks from the time of injury [7]. The treatment options in these cases vary from conservative management to operative procedures like open reduction and filling the defect using allograft or autograft, subscapularis muscle transposition (McLaughlin procedure), proximal humeral rotational osteotomy, lesion repair, or shoulder arthroplasty [7]. The choice of surgical procedure is governed by the size of RHSL. A CT scan is required to measure the size of the lesion on axial planes. Cases with defects <25% of the humeral head can be treated conservatively whereas those with RHSL involving more than 45% of the humeral head are treated by shoulder replacement surgery. The modified McLaughlin procedure is best suited for defects ranging from 25% to 45% of the humeral head. The procedure can also be augmented using an autograft from the iliac crest to restore the shape of humeral head and achieve stability [8]. Multiple studies have been done on the efficacy of this procedure in CLPD patients. The major complications reported after the surgery included osteonecrosis of the humeral head and osteoarthritis of the glenohumeral joint, but the occurrence of these was very rare. The recurrence of instability or dislocation has hardly ever been reported which shows the benefit of this procedure in chronic cases [1-4]. Various studies have also proved that the use of an allograft or autograft provides an advantage in cases where the LT transfer does not completely restore the shape of humeral head [9]. Xiong et al. conducted a prospective study on five patients of CLPD managed by the modified McLaughlin procedure and found significant improvements in functions of the shoulder at 3-month post-surgery. They reported no complications in any patient and concluded that a partial LT transfer and use of an allograft provide similar results as compared to the complete LT transfer and use of autograft as done in our patient [1]. Haritinian et al. conducted a retrospective analysis on the outcome of this procedure in CLPD patients and found significant improvements in the clinical scores of the patients after surgery [8]. Ippolito et al. conducted a comparative study on patients with acute, irreducible dislocations with an associated RHSL. They evaluated the outcome of an arthroscopic McLaughlin procedure and the open modified McLaughlin procedure in the study group and found no significant difference in the clinical outcomes of the 2 groups of patients [10]. Cohen et al. conducted a study on 10 patients who underwent the procedure for CLPD and reported that the functional recovery was better and profound in patients who presented <6 months from the injury. Cases with delay in diagnosis more than 6 months showed poor functional outcomes and increased chances of degenerative disease of the joint [7].
Posterior dislocations present as a diagnostic trap since they are often missed in routine practice. The management of CLPD is a challenge and depends upon factors such as the injury time, size of RHSL, functional expectations of the patient, and anatomical status of the joint. In cases with humeral head defects ranging from 25% to 45%, the modified McLaughlin procedure has proven to be a successful procedure. The technique addresses the important objectives of restoration of anatomy and reimposition of the stability with complications owing only to the chronicity of the condition. The patient in our report had a delay of 6 months from injury but a vigilant and innovative approach to the case resulted in excellent results after surgery.
- The duration of locked posterior dislocation and the humeral head defect size affects the treatment strategy to achieve the best functional outcome
- Modified McLaughlin procedure is best suited to restore the functioning of the glenohumeral articulation in cases with humeral head defect size <45%
- The use of a bone graft helps in stable fixation and near-normal restoration of humeral head anatomy in addition to the LT transfer.
References
- 1.Xiong F, Yin Q, Wang J, Wei C, Gu S, Liu Y. A novel modified McLaughlin surgery for treating locked chronic posterior shoulder dislocation. BMC Musculoskelet Disord 2023;24:114. [Google Scholar | PubMed]
- 2.Burkett CM, Roberts CS, Franklin GA. Successful treatment of chronic, locked posterior shoulder dislocations in young trauma patients with the modified McLaughlin procedure. Eur J Trauma 2006;32:179-84. [Google Scholar | PubMed]
- 3.Konrads C, Konrads MI, Döbele S, Histing T, Ziegler P. Posterior shoulder dislocation with associated reverse Hill-Sachs lesion: Clinical outcome 10 years after joint-preserving surgery. Arch Orthop Trauma Surg 2022;143:2503-7. [Google Scholar | PubMed]
- 4.Demirel M, Erşen A, Karademir G, Atalar AC, Demirhan M. Transfer of the lesser tuberosity for reverse Hill-Sachs lesions after neglected posterior dislocations of the shoulder: A retrospective clinical study of 13 cases. Acta Orthop Traumatol Turc 2017;51:362-6. [Google Scholar | PubMed]
- 5.Gerber C, Catanzaro S, Jundt-Ecker M, Farshad M. Long-term outcome of segmental reconstruction of the humeral head for the treatment of locked posterior dislocation of the shoulder. J Shoulder Elbow Surg 2014;23:1682-90. [Google Scholar | PubMed]
- 6.Moroder P, Tauber M, Hoffelner T, Auffarth A, Korn G, Bogner R, et al. Reliability of a new standardized measurement technique for reverse Hill-Sachs lesions in posterior shoulder dislocations. Arthroscopy 2013;29:478-84. [Google Scholar | PubMed]
- 7.Cohen M, Fonseca R, Amaral MV, Monteiro MT, Motta Filho GR. Treatment of chronic locked posterior dislocation of the shoulder with the modified McLaughlin procedure. J Shoulder Elbow Surg 2022;31:100-6. [Google Scholar | PubMed]
- 8.Haritinian EG, Stoica IC, Popescu R, Gheorghievici GL, Nové-Josserand L. Treatment and outcomes of chronic locked posterior shoulder dislocations: A retrospective case series. BMC Musculoskelet Disord 2023;24:82. [Google Scholar | PubMed]
- 9.9. Kokkalis ZT, Mavrogenis AF, Ballas EG, Papanastasiou J, Papagelopoulos PJ. Modified McLaughlin technique for neglected locked posterior dislocation of the shoulder. Orthopedics 2013;36:e912-6. [Google Scholar | PubMed]
- 10.Ippolito G, Zitiello M, De Marinis G, D’angelo F, Surace MF, Ronga M, et al. Posterior shoulder dislocation with engaging reverse hill-Sachs lesion: A retrospective study of ten patients treated with arthroscopy or open reduction and stabilization. J Clin Med 2021;10:1410. [Google Scholar | PubMed]