Meticulous cementing technique during hemiarthroplasty is essential to prevent cement interposition, which can lead to chronic hip dislocation, instability, and the need for complex revision surgery.
Dr. Vasavi Pushadapu, Department of Orthopaedics, Mamatha Academy of Medical Sciences, Bachupally, Hyderabad, Telangana, India. E-mail: drvasavipushadapu09@gmail.com,
Introduction: Hemiarthroplasty is commonly performed for displaced femoral neck fractures in elderly patients. While generally effective, poor cementing techniques can lead to serious complications, including implant migration and chronic dislocation. Cement interposition in the acetabulum is a rare but preventable cause of persistent instability. This case emphasizes the importance of meticulous cement handling and intraoperative vigilance to avoid avoidable revision surgeries.
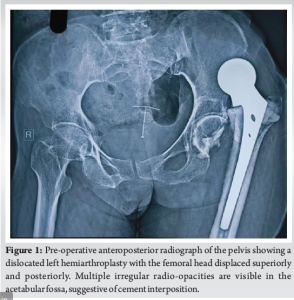
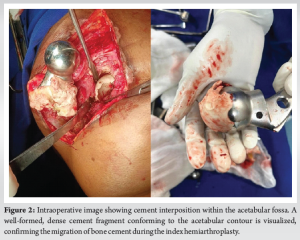
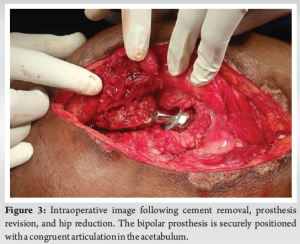
Case Report: A 76-year-old woman presented 8 months after left hemiarthroplasty with persistent hip pain and immobility. She had become bedridden 1-month post-surgery following a sensation of hip slippage. Examination revealed limb shortening, adduction deformity, and restricted mobility. Radiographs showed a dislocated hip and multiple dense opacities in the acetabulum, suggesting cement interposition. A posterior approach revision was planned. Pre-operative skin traction and adductor tenotomy were performed to address soft tissue contractures. Intraoperatively, well-formed cement mass conforming to the acetabulum was removed. The cement was removed en bloc, and a bipolar prosthesis was implanted. Post-operatively, the patient achieved satisfactory recovery with improved hip stability and function.
Discussion: This case illustrates the potential for cement to migrate into the acetabulum during stem insertion if introduced pre-maturely or in excess. Such interposition disrupts joint articulation and can lead to chronic dislocation. Preventive steps – such as waiting for appropriate cement consistency, using a gauze barrier in the acetabulum, and careful intraoperative assessment – are critical to avoid such outcomes. Chronic dislocations further complicate surgical revisions due to soft tissue contractures and biomechanical imbalance. Comprehensive pre-operative planning and soft tissue management, combined with appropriate implant selection, contributed to successful revision in this case. Conclusion: Cement interposition is a rare but preventable cause of chronic dislocation after hemiarthroplasty. This case highlights the need for precise cementing techniques, careful intraoperative assessment, and proactive management strategies. Attention to these details can reduce complications and improve outcomes in elderly patients undergoing hip arthroplasty.
Keywords: Chronic hip dislocation, hip revision surgery, cementing technique.
Hemiarthroplasty is a widely accepted treatment for displaced femoral neck fractures in elderly patients, providing pain relief and facilitating early mobilization. However, complications arising from suboptimal surgical techniques, particularly poor cementing practices, can lead to devastating outcomes. Proper cementation is crucial for implant stability, as inadequate technique increases the risk of aseptic loosening, periprosthetic fractures, and implant migration [1,2]. Failure to achieve an adequate cement mantle predisposes patients to early implant failure, dislocations, and, as in this case, cement interposition leading to chronic dislocation. This case report highlights the consequences of poor cementing techniques in hemiarthroplasty, leading to chronic hip dislocation due to cement interposition. It underscores the importance of meticulous cementing, ensuring the correct cement consistency before application, thorough intraoperative assessment, and timely intervention to prevent catastrophic implant failures. By discussing the surgical challenges encountered and the successful management strategy employed, this report aims to contribute valuable insights for orthopedic surgeons managing similar complications.
A 76-year-old female patient underwent a left Non-modular unipolar hemiarthroplasty 8 months ago in view of fracture neck of femur, based on the previous scar the procedure was performed through a posterior approach. The patient was able to walk with the help of a walker for 1 month post-surgery after which the patient experienced a sudden shift or slipping sensation in the hip, followed by pain and difficulty moving. At the time of the slippage, the patient did not seek immediate medical attention. Due to limited mobility and lack of access to local orthopedic care, she remained bedridden at home and received only symptomatic treatment in the form of analgesics prescribed by a local physician. No radiographic evaluation or surgical consultation was done until she presented to our outpatient department 8 months post-surgery with chief complaints of persistent left hip pain and restricted mobility and function of the left hip. She was unable to bear weight on her left limb and was bedridden for 7 months. On clinical examination, the left leg was shortened with a limb length discrepancy of 4 cm and was fixed in adduction and internal rotation. The patient was sent for radiographic examination, and a dislocated left hip was confirmed, additionally, they revealed multiple irregular radio-opacities in the acetabular fossa, raising suspicion of cement interposition, retained bony fragments, or intra-articular ossification. The opacities varied in density, with some areas appearing homogeneous and others more fragmented (Fig. 1). A computed tomography scan was considered to better assess cement penetration, retained bone fragments, and acetabular integrity. However, due to financial constraints, further imaging was not pursued. The surgical plan was formulated based on clinical findings and standard radiographs, with intraoperative evaluation guiding implant selection. Pre-operatively, a percutaneous adductor tenotomy was performed to release contractures caused by the chronic dislocation. In addition, skin traction was applied for 2 weeks to help gradually correct limb alignment, reduce muscle stiffness, and facilitate intraoperative reduction. A posterior approach was selected to facilitate access to both the acetabulum and femoral canal while ensuring adequate visualization. Intraoperatively, a well-formed cement mantle was identified conforming to the acetabular shape, confirming cement migration as the underlying pathology. No bony remnants or free-floating osteochondral fragments were observed, effectively ruling out residual femoral head fragments and intra-articular loose bodies. The acetabular walls were intact, and no signs of osteolysis, sequestrum, or infection were observed. The extracted cement was removed en bloc (Fig. 2). A bipolar prosthesis was chosen over total hip replacement (THR) due to the patient’s advanced age, lower functional demands, and intact acetabular wall with no significant erosion or osteolysis. In contrast to the index surgery, meticulous cementing technique was followed. The acetabulum was protected using moist gauze to prevent cement entry, and the cement was introduced only in its doughy phase. The femoral canal was thoroughly prepared, and cement was introduced retrograde with controlled pressurization to achieve a uniform mantle and secure implant fixation. The hip was successfully reduced, ensuring good stability and range of motion (Fig. 3). Given the patient’s advanced age and osteoporotic bone quality, prophylactic cerclage wiring was applied in the subtrochanteric region to reinforce the femur and minimize the risk of intraoperative or post-operative periprosthetic fracture. Thorough irrigation to minimize the risk of infection, careful soft tissue balancing to optimize hip biomechanics, and repair of the posterior capsule to enhance stability were done. Intraoperative assessment confirmed satisfactory positioning of the prosthesis with no undue impingement or instability. Closure was performed in layers, and the patient was stabilized post-operatively. Standard operating procedures were maintained. The immediate post-operative radiograph demonstrated a well-seated bipolar prosthesis with concentric reduction of the hip joint. The acetabular contours appeared intact with no residual cement fragments or signs of joint incongruity. Limb alignment was restored with no limb length discrepancy, and the implant position was stable without evidence of subsidence or malposition (Fig. 4). The patient had a smooth recovery and was discharged 2 weeks after surgery with instructions for partial weight-bearing using bilateral axillary crutches and focusing on restoring hip mobility and muscle strength.
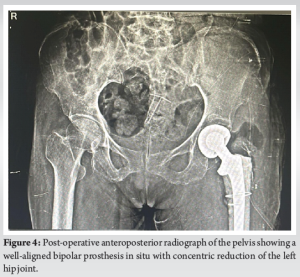
The present follow-up duration is 9 months post-revision surgery. The patient has shown good functional recovery, with no recurrence of dislocation or implant-related complications. She is ambulatory with the help of a stick and reports improved pain and mobility.
Proper cementation in hemiarthroplasty is essential for ensuring stable fixation of the prosthesis to the bone, which is crucial for the implant’s longevity and functionality. Inadequate cementing can compromise the cement mantle, leading to micromovements of the implant, accelerated wear, and eventual mechanical failure. These failures can manifest as aseptic loosening, periprosthetic fractures, and dislocations, making the integrity of the cement mantle a critical factor in the success of the arthroplasty [1]. Achieving the correct cement consistency is a critical step in hemiarthroplasty. Bone cement should reach a doughy, non-sticky phase before placement to allow optimal pressurization, and uniform mantle formation, and to prevent extrusion into unintended areas [3]. If introduced too early, while still in a liquid or sticky state, the cement may migrate into the acetabulum during stem insertion, particularly if excessive cement is used or if the femoral canal is inadequately sealed [4]. Cement dripping into the acetabulum can result in intra-articular interposition, disrupting joint biomechanics and leading to persistent instability and dislocation, as seen in this case [5]. One crucial yet often overlooked step in cementing techniques during hemiarthroplasty is the placement of a moist sponge or gauze in the acetabulum before introducing bone cement. This simple measure serves as a mechanical barrier, preventing inadvertent cement migration into the acetabular fossa. Cement interposition within the joint space can lead to serious complications, including chronic instability, restricted range of motion, and persistent pain. Using a well-moistened gauze or sponge ensures that the cement remains confined to the femoral canal, allowing for an optimal cement mantle without the risk of intra-articular spillage. In addition, careful removal of the sponge after cementation must be ensured to avoid retained foreign bodies, which can themselves become sources of mechanical obstruction or infection. This preventive step significantly reduces the likelihood of cement-related complications, reinforcing the need for meticulous intraoperative technique [6]. Cement interposition is a rare but serious cause of chronic dislocation, compromising joint function by obstructing femoral head articulation and causing persistent instability and pain [7]. While intra-articular cement fragments may result from technical errors during implantation, they can remain asymptomatic or, as in this case, lead to severe morbidity. Identifying and addressing such complications is crucial to improving patient outcomes and avoiding complex revision surgeries [8]. In addition, Chronic dislocations present significant challenges, leading to functional impairment, pain, and periarticular fibrosis, which complicate revision surgeries [9]. Managing such complications requires a comprehensive approach. Pre-operative strategies, such as percutaneous adductor tenotomy and skin traction, can aid in correcting limb alignment and reducing muscle stiffness, facilitating intraoperative reduction. Intraoperatively, selecting an appropriate surgical approach is crucial. The posterior approach, in this case, allowed adequate visualization for cement removal. The decision to opt for a bipolar prosthesis over THR was influenced by the patient’s age, functional demands, and the integrity of the acetabular wall. Post-operative management focusing on partial weight-bearing and rehabilitation is vital for optimal recovery [10]. This case underscores the imperative of meticulous surgical technique in hemiarthroplasty, particularly concerning cementing practices. Thorough intraoperative assessment and prompt intervention are crucial in preventing catastrophic implant failures. Orthopedic surgeons must remain vigilant about potential complications arising from cement interposition and adopt strategies to mitigate such risks, thereby improving patient outcomes and reducing the necessity for complex revision surgeries [11].
This case highlights the critical role of proper cementing techniques in hemiarthroplasty and the devastating consequences of cement interposition leading to chronic dislocation. Cement migration into the acetabulum can severely disrupt joint biomechanics, causing persistent instability, pain, and functional impairment. Prevention strategies, including meticulous cement handling, maintaining optimal cement consistency, and using a mechanical barrier to prevent interposition, are essential to avoid such complications. For patients presenting with chronic hip dislocation due to cement interposition, a structured approach involving thorough pre-operative planning, appropriate surgical technique, and tailored post-operative rehabilitation is crucial. In this case, a combination of pre-operative soft tissue management, intraoperative cement removal, and proper implant selection allowed for successful revision surgery with restored hip stability and function. This case reinforces the need for vigilance in cementation practices and serves as a reminder that attention to detail during primary surgery can prevent complex and avoidable revision procedures. By adhering to best practices in cementing and intraoperative assessment, orthopedic surgeons can significantly improve patient outcomes and enhance the longevity of hemiarthroplasty implants.
Meticulous cementing technique is crucial in hemiarthroplasty to prevent complications, such as cement interposition, which can lead to chronic instability and dislocation. Ensuring the correct cement consistency, using preventive measures like a mechanical barrier, and conducting thorough intraoperative assessment can help avoid avoidable revision surgeries. Attention to detail during the primary procedure significantly improves implant longevity and patient outcomes.
References
- 1. Berry DJ, Maloney WJ. The well-cemented total hip arthroplasty. In: Theory and Practice. Berlin: Springer; 2005. Available from: https://link.springer.com/book/10.1007/3-540-28924-0 [Google Scholar] [PubMed] [CrossRef]
- 2. Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impaction bone grafting of the femur: A decade of experience. J Bone Joint Surg Br 1993;75:14-21. [Google Scholar] [PubMed]
- 3. Lee AJ, Ling RS. Simple guidelines for optimal cementing technique in hip arthroplasty. J Bone Joint Surg Br 1998;80:757-9. [Google Scholar] [PubMed]
- 4. Oh I, Harris WH. The femoral cement wedge: Its effect on cement fixation and strength. J Bone Joint Surg Am 1978;60:889-94. [Google Scholar] [PubMed]
- 5. Howard JL, Kremers HM, Loechler YA, et al. Comparative survival of uncemented and cemented hemiarthroplasty for femoral neck fracture. J Bone Joint Surg Am 2015;97:1855-62. [Google Scholar] [PubMed]
- 6. Scott S, McCaskie AW, Calder SJ, Wildin C, Gregg PJ. Current cementing techniques in hip hemi-arthroplasty. Injury 2001;32:461-4. [Google Scholar] [PubMed]
- 7. Stucinskas J, Tarasevicius S, Robertsson O, Wingstrand H. Dislocation after total hip arthroplasty: Implant positioning and other risk factors. Acta Orthop 2008;79:323-6. [Google Scholar] [PubMed]
- 8. Della Valle AG, Padgett DE, Salvati EA. Preoperative planning for primary total hip arthroplasty. J Am Acad Orthop Surg 2005;13:455-62. [Google Scholar] [PubMed]
- 9. Berry DJ. Unstable total hip arthroplasty: Detailed overview. Instr Course Lect 2001;50:265-74. [Google Scholar] [PubMed]
- 10. Sariali E, Lazennec JY, Khiami F, Catonné Y. Anatomical variation of the femoral offset: Implications for total hip arthroplasty. Eur J Orthop Surg Traumatol 2009;19:643-7. [Google Scholar] [PubMed]
- 11. Malchau H, Herberts P, Söderman P, Odén A. Update on long-term survival of hip replacement. Clin Orthop Relat Res 2002;403:22-8. [Google Scholar] [PubMed]









