Early diagnosis and prompt surgical management are critical in acute unstable SCFE to prevent catastrophic complications like avascular necrosis.
Dr. B Mohan Choudhary, Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: kartheekasthird@gmail.com
Introduction: Slipped capital femoral epiphysis (SCFE) is a common hip disorder in adolescents, characterized by the displacement of the femoral head from the femoral neck along the physeal plate. Diagnosis relies on clinical evaluation and radiographic imaging, with classification based on duration, stability, and severity. The standard treatment is in situ pinning using a single cannulated screw to stabilize the epiphysis. However, the modified Dunn procedure (MDP) has emerged as an alternative, particularly for unstable slips, aiming to reduce osteonecrosis risk. SCFE is associated with significant complications, including osteonecrosis, chondrolysis, slip progression, and femoro-acetabular impingement. Long-term management focuses on preserving hip function and delaying the need for hip arthroplasty.
Case Report: A 15-year-old boy with normal body mass index (BMI) of 18.6 kg/m2 had trivial fall while playing and had difficulty in walking. Five days post injury, he was not able to weight bear with increasing progression of pain. Based on radiographs, SCFE was suspected and computed tomography scan was done to confirm the slip. He underwent MDP and started on post-operative rehabilitation protocol.
Conclusion: This review shows the effectively managed acute presentation of SCFE in normal BMI children. Sudden trauma does not rule out SCFE and a differential diagnosis to be always considered along with fractures.
Keywords: Acute slipped capital femoral epiphysis, Ganz surgical dislocation of hip, modified Dunn’s procedure, femoro-acetabular impingement, avascular necrosis.
Slipped capital femoral epiphysis (SCFE) is the most common hip disorder in adolescents, occurring due to the displacement of the capital femoral epiphysis relative to the femoral neck along the growth plate [1]. The exact etiology remains unclear but is associated with obesity, hormonal imbalances, and mechanical factors affecting the growth plate [2]. SCFE is classified into three main categories: (1) Duration-based classification includes acute where symptoms were lasting <3 weeks, chronic where symptoms were persisting >3 weeks, acute-on-chronic where chronic slip is present with a recent worsening of symptoms [3]. (2) Stability-based classification. Stable means the patient can bear weight with or without crutches. Unstable means the patient is unable to bear weight, even with crutches [4]. (3) Severity-based classification (Southwick slip angle classification) mild is <30°, moderate is 30°–50°, severe is >50° [5]. Treatment approaches [6] are in situ pinning (ISP) where a single cannulated screw is inserted into the femoral epiphysis to prevent further slippage. Most widely used treatment for stable, mild-to-moderate SCFE. Advantages are minimally invasive, effective in stabilizing the epiphysis, lower complication rates compared to open procedures. Limitations include persistence of residual deformity which may contribute to FAI.. Another treatment approach includes modified Dunn’s procedure (MDP) which is an open surgical technique that aims to restore normal hip anatomy and preserve blood supply to the femoral head. It is done especially for unstable and severe slips. It involves surgical dislocation of the hip, osteotomy of the greater trochanter, realignment, and fixation of the femoral head [7,8]. Advantages are potentially reducing the risk of osteonecrosis in unstable SCFE, restore normal hip anatomy, and may lower the risk of FAI. Limitations include technically demanding, requiring high surgical expertise, higher risk of osteonecrosis in some studies [9]. Complications of SCFE are osteonecrosis, most serious complication, particularly in unstable SCFE, occurring in 24–47% of cases. Chondrolysis is the progressive destruction of articular cartilage, leading to persistent hip pain and stiffness. Slip progression occurs due to implant failure and continued femoral neck growth, causing the epiphysis to outgrow the screw. FAI is a common long-term consequence of SCFE, affecting 32–90% of patients. It occurs when the deformed femoral neck impinges against the acetabulum, leading to pain and stiffness during hip flexion and internal rotation [10]. ISP carries fewer immediate risks but may leave residual deformity requiring later arthroscopic/open reshaping. MDP offers true anatomic correction but demands meticulous technique to avoid avascular necrosis (AVN) and other open surgery complications. The ISP versus MDP debate continues, with ongoing research focusing on identifying which patients benefit most from MDP, reducing the risk of osteonecrosis in unstable SCFE, improving long-term hip function while minimizing complications [6]. Newer techniques include use of intraoperative Doppler or laser flowmetry to assess epiphyseal perfusion during MDP that is gaining traction to reduce AVN risk. 3D navigation and planning, arthroscopic-assisted reductions are being explored to improve outcomes and reduce complications [1].
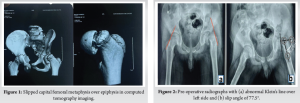
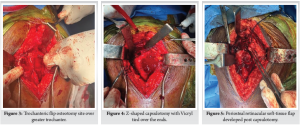
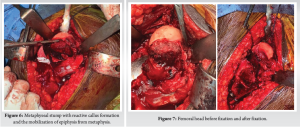
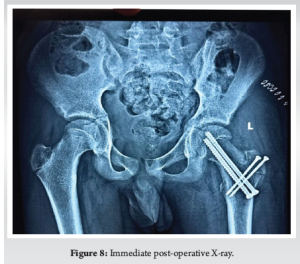
A 15-year-old boy with body mass index (BMI)-18.6 kg/m2 presented to the emergency department with acute left hip pain and inability to bear weight. The pain began after a minor stumble while playing at his school, though he denied any significant trauma. He was initially able to weight bear but gradually pain progressed leading to difficulty in walking and unable to weight bear over the past 24 h. His medical history was unremarkable. His family history was negative for hip disorders, early-onset osteoarthritis, or metabolic conditions. Examination revealed lower limb in flexion, shortened and externally rotated with diffuse tenderness over hip region. Radiography showing widening and irregularity of the left physeal plate, posterior displacement of the femoral epiphysis relative to the femoral neck (Fig. 1] and Klein’s line failed to intersect the epiphysis (positive Trethowan’s sign) (Fig. 2a). Based on clinical presentation and imaging, the patient was diagnosed with: Unstable, severe SCFE (Fig. 2b) (Southwick angle >50°), high risk for osteonecrosis due to inability to bear weight. Given the severity of displacement and instability, MDP was selected over traditional ISP to restore hip anatomy and preserve femoral head vascularity. Patient underwent the MDP through a Ganz surgical hip dislocation approach, performed under general anesthesia. A straight digastric osteotomy of the greater trochanter was performed leaving the most posterior fibers of gluteus medius tendon intact (Fig. 3). This did not potentially endanger the deep branch of the medial femoral circumflex artery. Mobilization of the trochanteric fragment together with the vastus, gluteus minimus, and medius muscles was done ventrally to expose the capsule. A Z-shaped capsulotomy was performed providing access to the displaced epiphysis (Fig. 4). Femoral epiphysis was temporarily pinned with 2 mm Kirschner wires. The viability of femoral epiphysis was ensured by drilling of the femoral head. Dislocation of femoral head was done by flexion and external rotation and placement in a sterile bag by the side of operating table. Full inspection of acetabulum was done to see any corresponding chondral damage. After relocating the head, retinacular soft-tissue flap containing deep branch of medial femoral circumflex artery, the periosteum, the piriformis muscle, part of the posterior capsule, and the short external rotators was developed (Fig. 5). Distally, the flap was mobilized till the level of the lesser trochanter which reduced the tension from the retinacular vessels. Complete epiphyseal mobilization (Fig. 6) and carefully separating the femoral epiphysis from the posteriorly displaced metaphysis was facilitated by external rotation. The excess callus formation of the metaphysis which was seen was resected until a spherical surface of neck became reapparent. The epiphysis was then reduced manually on the metaphyseal stump (Fig. 6). A 3.0 mm Kirschner wire was placed anterograde for temporary reduction and checked under fluoroscopy for capital realignment. Internal fixation was done using one fully (75 mm) and one partially (80 mm) threaded 6.5 mm cannulated cancellous screws for stable fixation (Fig. 7). Retinacular soft-tissue flap was reattached back with tension free sutures. Similarly, capsule was closed without tension. Osteotomy site was fixed at the end with two 3.5 mm cortical screws. In immediate post-operative period (Fig. 8), the patient was kept non-weight-bearing for 6 weeks with strict activity modification, physical therapy initiated with passive range-of-motion (ROM) exercises at post-operative day 2 to prevent stiffness, pain was well controlled with non-steroidal anti-inflammatory drugs, and no early post-operative complications were noted. 6 weeks post-operative, radiographs showed stable fixation with no further slip progression, early signs of physeal healing were observed. Patient regained near full near-full ROM with no significant pain (Fig. 9). Three months post-operative (Fig. 10), the patient transitioned to full weight-bearing. At present, the patient is 4 months post-operative and able to do regular activities without restriction. Radiographs showed complete healing of the osteotomy site No clinical or radiographic evidence of FAI or chondrolysis were found.


For unstable SCFE, ISP is associated with high rates of osteonecrosis (24–47%) due to vascular compromise. The MDP was chosen in this case because it allows direct realignment of the epiphysis, correcting the deformity, it preserves blood supply by careful dissection and protection of the posterior retinacular vessels, it potentially reduces long-term complications such as FAI [6,7]. Unstable SCFE requires urgent intervention due to the high risk of osteonecrosis. Magnetic resonance imaging can be valuable preoperatively to assess vascular status and guide surgical decisions. The MDP can be successful in select patients, but requires significant surgical expertise [11]. Early post-operative monitoring for osteonecrosis is crucial. This case highlights the successful management of an unstable, severe SCFE using the MDP.
Unstable SCFE with acute presentation requires urgent and precise management to prevent long-term morbidity. In this case, the MDP provided effective realignment of the epiphysis with preservation of femoral head vascularity in a 15-year-old child with normal BMI. This technique, when performed using safe surgical hip dislocation and strict attention to vascular preservation, offers favorable outcomes in unstable slips. Early diagnosis, appropriate surgical planning, and meticulous execution are essential to minimize complications such as AVN and to optimize functional recovery.
The MDP remains a reliable surgical option for acute unstable SCFE, emphasizing the importance of early diagnosis, safe dislocation techniques, and vascular preservation to ensure optimal patient outcomes.
References
- 1. Zuo B, Zhu JF, Wang XY, Wang CL, Ma F, Chen XD. Outcome of the modified Dunn procedure in severe slipped capital femoral epiphysis. J Orthop Surg Res 2020;15:506. [Google Scholar] [PubMed]
- 2. Loder RT, Wittenberg B, DeSilva G. Slipped capital femoral epiphysis associated with endocrine disorders. J Pediatr Orthop 1995;15:349-56. [Google Scholar] [PubMed]
- 3. Peck DM, Voss LM, Voss TT. Slipped capital femoral epiphysis: Diagnosis and Management. Am Fam Physician 2017;95:779-84. [Google Scholar] [PubMed]
- 4. Aronsson DD, Loder RT, Breur GJ, Weinstein SL. Slipped capital femoral epiphysis: Current concepts. J Am Acad Orthop Surg 2006;14:666-79. [Google Scholar] [PubMed]
- 5. Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am 1967;49:807-35. [Google Scholar] [PubMed]
- 6. Abu Amara S, Leroux J, Lechevallier J. Surgery for slipped capital femoral epiphysis in adolescents. Orthop Traumatol Surg Res 2014;100(Suppl 1):S157-67. [Google Scholar] [PubMed]
- 7. Tannast M, Jost LM, Lerch TD, Schmaranzer F, Ziebarth K, Siebenrock KA. The modified Dunn procedure for slipped capital femoral epiphysis: The Bernese experience. J Child Orthop 2017;11:138-46. [Google Scholar] [PubMed]
- 8. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;83:1119-24. [Google Scholar] [PubMed]
- 9. Madan SS, Cooper AP, Davies AG, Fernandes JA. The treatment of severe slipped capital femoral epiphysis via the Ganz surgical dislocation and anatomical reduction: A prospective study. Bone Joint J 2013;95-B:424-9. [Google Scholar] [PubMed]
- 10. Vukasinović Z, Slavković N, Slavković S. Complications of slipped capital femoral epiphysis. Srp Arh Celok Lek 2007;135:105-10. [Google Scholar] [PubMed]
- 11. Slongo T, Kakaty D, Krause F, Ziebarth K. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am 2010;92:2898-908. [Google Scholar] [PubMed]











