Early MRI is essential for diagnosing bilateral tibial stress fractures in athletes with persistent leg pain and inconclusive X-rays, enabling prompt tibial nailing to support effective recovery and return to sport.
Dr. Zakir Ali Shah, Department of Trauma and Orthopedic, Rashid Hospital, Dubai, United Arab Emirates. E-mail: drzakiralishah@gmail.com
Introduction: Early stress fractures sometimes go undetected or are misdiagnosed due to unusual subtle symptoms; anterior tibial fractures are mostly tiny unilateral fractures involving the diaphyseal portion of the tibia as a result of repetitive microtrauma as deemed in intense athletes. Incomplete anterior tibial stress fractures are very rare, particularly when they occur bilaterally in football players.
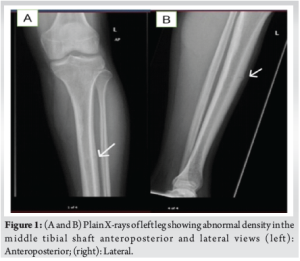
Case Report: Here, we discuss a rare clinical case of a sportsman who presented in our hospital. A 26-year-old professional football player presented to us in July 2024 with bilateral leg pain which worsened on playing football. The plain radiograph showed that the middle part of the left side tibial shaft anteriorly had higher density, while the right side was unremarkable; which was further investigated with computed tomography scan on left side on presentation and magnetic resonance imaging on right side on 3 months follow up.
Conclusion: A thorough review of the patient’s history is essential when evaluating persistent leg pain associated with repetitive activities. Our report emphasis importance of early recognition and surgical intervention in seeking rapid return to play and be active especially in athletes.
Keywords: Magnetic resonance imaging, Athlete, Stress fracture, Tibia, Football players.
Stress fractures are mostly caused by repeated minor injuries that occur during increased or unusual physical activities. There are various body bones, which can be involved, but the most commonly affected bones are especially the tibia and metatarsals. Anterior tibial stress fractures are rare, constituting <5% of tibial stress fractures and bilateral cases are exceptionally uncommon. Tibial stress fractures are seen in all ages, but are more common in adolescent athletes. In 1956, Burrows conducted a study on ballet dancers and reported that they had stress fractures in the anterior cortex of the tibia [1]. There are numerous contributing factors that cause delay or incorrect diagnosis of initial stress fractures in the clinical environment. These fractures generally do not involve any history of trauma and have an unusual presentation. In addition, basic radiographic imaging has proved to have difficulties in making an early diagnosis. However, nuclear imaging and magnetic resonance imaging (MRI) have demonstrated encouraging outcomes in the timely identification of these fractures. Bilateral anterior tibial stress fractures are uncommon and necessitate thorough assessment along with heightened clinical vigilance for accurate diagnosis and treatment. When diagnosing stress fractures, it is important to consider osteochondritis dissecans, osteonecrosis, ligament injuries, periosteal reactions, osteomyelitis, periostitis, and bone tumors. This case report focuses on the delayed identification of anterior tibial shaft stress fractures in a football player, a sport known for inflicting repeated minor impacts on the legs, and the situation will be examined in the context of the present literature.
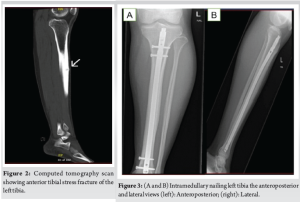
A 26-year-old male professional football player presented to us in the outpatient clinic in July 2024, on wheelchair with the complaint of bilateral shin pain over the past 4 months, localized on the anterior aspect of both legs. The pain was initially mild and worsened during playing football, followed by a constant pain on the left side, which started affecting his sleep and his routine activities. In addition, he complained of mild discomfort on his right leg. He had no history of any recent trauma and other joints or extremity pain in the past, but claimed an increase in intensity of pain while playing football. He had previously used anti-inflammatory medications, calcium, and activated cholecalciferol supplements, and underwent 8 sessions of physiotherapy. During physical examination, inspection revealed normal gait and normal alignment of both lower limbs and there was mild tenderness left mid leg and absent tenderness on the right side on palpation. The range of motion of associated joints and spine was within normal limits. Sensory and motor of each lower limb was normal and comparable. Plain X-ray of left leg (Fig. 1) demonstrated abnormal density in the middle left tibial shaft anteriorly, while right tibia X-rays were inconclusive. Based on X-ray results, the possibility of osteomyelitis in the left tibia was considered, and all inflammatory markers (C-reactive protein, erythrocyte sedimentation rate) were sent, revealing normal levels, which excluded any infections. In addition, endocrine/metabolic workup (Vitamin D, Calcium, parathyroid hormone, thyroid-stimulating hormone, and testosterone) was done and was in normal limits. A computed tomography (CT) scan confirmed left tibia anterior shaft stress fracture (Fig. 2). After reviewing the patient’s history, review of all medications, and thorough examination, including a careful biomechanical assessment and scanning results, a diagnosis of a stress fracture in the left tibia was made. Due to a lack of improvement with trial of conservative management on the left side over the past 4 months, a decision was made to proceed with intramedullary nailing on the left tibia while continuing conservative treatment on the right side, as the X-rays were unremarkable. Post-operative recovery of the patient was unremarkable, and he was allowed weight bearing as tolerated under the supervision of a physiotherapist (Fig. 3). At 3 months, he presented to the outpatient clinic as a follow-up case, with minimal symptoms in his left tibia. However, he expressed ongoing discomfort and mild pain in his right leg, which he claimed partly alleviated with analgesics and avoiding exertional activities. Due to ongoing pain on his right side, right leg X-rays were performed that revealed suspicion of anterior cortex stress fracture (Fig. 4). Consequently, an MRI was performed, which displayed a low signal on T2-weighted imaging with cortical thickening and bone marrow edema, confirming anterior tibial stress fracture (Fig. 5). Keeping in view his previous history, present imaging results and delayed diagnosis, he was decided to undergo intramedullary nailing right tibia. At the 4-month follow-up after the surgical fixation of his right tibial stress fracture, the patient was fully ambulant without any support. Follow-up radiographs of the right leg showed an evidence of fracture healing and nail in situ (Fig. 6). By 6 months, the patient returned to competitive football without restrictions.

Athletes continuously push their physical limits to enhance performance, which increases their risk of developing microfractures, as concluded in a study by Fredericson et al., [2]. Stress fractures can happen in various bones throughout the body, such as the metatarsals, fibula, femur, pelvis, calcaneus, and tibia; however, the tibia and metatarsals are documented as the most frequently affected bones in individuals of all age groups [3,4]. People with stress fracture symptoms often reduce the intensity and frequency of their daily activities. Stress fractures are divided into two categories by most of the authors [5,6]: Those that happen in healthy bones from excessive repetitive activity, and those occurring in weakened bones under normal stress. Strong bones usually break under repeated strain in athletes and others engaging in similar activities. On the other hand, fragile bones can break from everyday forces due to systemic issues, such as bone diseases and certain health conditions, such as exposure to radiation. Athletes who concentrate on racing are prone of experiencing stress fractures because of their high impact running and repetitive strain. When the ongoing pressure on bones from constant mechanical stress surpasses the body’s capacity to heal, it can lead to stress fractures and bone weakening [7-9]. Early diagnosis is important to prevent incomplete fractures from worsening into non-union or full fractures, which necessitate more extensive treatment than in the earlier stages. The initial measures should always be conservative that is rest and stopping the activities that delay fracture healing [10-12]. Astur et al., and other studies believe that a stress fracture happens when the activity of osteoclasts outpaces the ability of osteoblasts to maintain bone density, leading to mechanical breakdown of the bone. They have proposed the prophylactic use of bisphosphonates to suppress osteoclast activity; however, there is currently no scientific foundation for their use in a preventative context [13]. Regarding surgical intervention, existing literature support that intramedullary nailing should be performed in anterior tibial fractures in athletes so that players can return to their game as early as possible. Brukner et al., [10,14] reported and treated bilateral anterior tibial stress fracture in football player with intramedullary nailing and were satisfied with outcome. Our case outcome supports Brukner et al., study. Lastly, we want to mention two potential reasons of the delayed diagnosis of anterior tibial stress fractures [15]. In this particular case, one of the reasons was mild clinical symptoms and unremarkable X-ray, due to which he continued his activities and the diagnosis on the right side was delayed, which was later confirmed on MRI. Another reason for a delayed diagnosis is that rest temporarily alleviates symptoms, which may lead many people to opt out of seeking an orthopedic review. The research conducted by Arendt and Griffiths [16] demonstrates that MRI is more effective than CT scans for diagnosing stress fractures. MRI imaging not only aid in the evaluation of stress fractures but also highlights bone marrow irregularities associated with repetitive trauma.
Due to rarity and subtle presentations, bilateral anterior tibial stress fractures in football players have always diagnostic and therapeutic challenges. It is highly recommended to perform MRI for early diagnosis whenever routine X-rays are inconclusive. Intramedullary nailing offers a reliable solution for athletes, enabling return to sport. This case emphasizes the importance of heightened clinical suspicion, comprehensive imaging, and biomechanical evaluation to prevent delays in diagnosis and optimize outcomes. Our future studies should focus on preventive measures and improved imaging protocols to facilitate early detection in high-risk groups.
Simultaneous bilateral anterior tibial pain is extremely rare in athletes. Maintain high clinical suspicion for stress fractures, even with normal X-rays, and promptly obtain MRI for early diagnosis. Early surgical intervention, such as intramedullary nailing, is critical to ensure timely recovery and safe return to sports.
References
- 1. Burrows HJ. Fatigue infraction of the middle of the tibia in ballet dancers. J Bone and Joint Surg Br 1956;38:83-94. [Google Scholar] [PubMed]
- 2. Fredericson M, Jennings F, Beaulieu C, Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging 2006;17:309-25. [Google Scholar] [PubMed]
- 3. Dhillon S, Ekstrand J, Mann G, Sharma S. Stress fractures in football. JISAKOS 2016;1:229-38. [Google Scholar] [PubMed]
- 4. Beck B, Drysdale L. Risk factors, diagnosis and management of bone stress injuries in adolescent athletes: A narrative review. Sports (Basel) 2021;9:52. [Google Scholar] [PubMed]
- 5. Choi HJ, Cho HM. Multiple stress fractures of the lower extremity in healthy young men. J Orthop Traumatol 2011;13:105-10. [Google Scholar] [PubMed]
- 6. Altuwairqi A. Bilateral stress fractures of the tibia in a long-distance runner. Cureus 2024;16:e70599. [Google Scholar] [PubMed]
- 7. Shindle MK, Endo Y, Warren RF, Lane JM, Helfet DL. Stress fractures about the tibia, foot, and ankle. J Am Acad Orthop Surg 2012;20:167-76. [Google Scholar] [PubMed]
- 8. Da Rocha Lemos Costa TM, Borba VZ, Correa RG, Moreira CA. Stress fractures. Arch Endocrinol Metab 2022;66:765-73. [Google Scholar] [PubMed]
- 9. Hadjispyrou S, Hadjimichael AC, Kaspiris A, Leptos P, Georgoulis JD. Treatment and rehabilitation approaches for stress fractures in long-distance runners: A literature review. Cureus 2023;15:e49397. [Google Scholar] [PubMed]
- 10. Orava S, Karpakka J, Hulkko A, Vaananen K, Takala T. Diagnosis and treatment of stress fractures located at the mid-tibial shaft in athletes. Int J Sports Med 1991;12:419-22. [Google Scholar] [PubMed]
- 11. Saunier J, Chapurlat R. Stress fracture in athletes. Joint Bone Spine 2018;85:307-10. [Google Scholar] [PubMed]
- 12. Matcuk GR, Mahanty SR, Skalski MR, Patel DB, White EA, Gottsegen CJ. Stress fractures: Pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2016;23:365-75. [Google Scholar] [PubMed]
- 13. Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini AC, Ejnisman B. Stress fractures: Definition, diagnosis and treatment. Rev Bras Ortop 2015;51:3-10. [Google Scholar] [PubMed]
- 14. Brukner P, Fanton G, Bergman AG, Beaulieu C, Matheson GO. Bilateral stress fractures of the anterior part of the tibial cortex. A case report. J Bone Joint Surg Am 2000;82:213-8. [Google Scholar] [PubMed]
- 15. Knapik JJ, Reynolds KL, Hoedebecke KL. Stress fractures: Etiology, epidemiology, diagnosis, treatment, and prevention. J Spec Oper Med 2017;17:120-30. [Google Scholar] [PubMed]
- 16. Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med 1997;16:291-306. [Google Scholar] [PubMed]











