Showcase varied presentations of giant cell tumor (GCT) at diverse locations, including distal radius and ulna, proximal tibia and tendon sheath with tailored surgical strategies to restore functional outcomes while minimizing recurrence.
Dr. Vinod Dubey, Department of Orthopedic, MRR Children Hospital, 1st, Pokhran road , Shastri Nagar, Vartak nagar , Thane West 400606, India. E-mail: vinoddubey195@gmail.com
Introduction: Giant cell tumor (GCT) in Orthopedics is a clinically challenging problem pertaining aggressive expansion and recurrence. While GCT’s typically occur at epiphyseal ends of long bones, unusual locations, such as tendon sheath, distal ulna, and proximal tibia have been reported, which impose different challenges for management.
Case Series: In this case series, we present surgical methodology tailored for individual characteristics of GCTs, with emphasis on functional recovery. We demonstrate four cases involving different sites GCT – tendon sheath in hand, distal ulna, distal radius, and proximal tibia. Each case was managed using a site-specific surgical approach, ranging from en bloc resection with ulna transposition and arthrodesis to Illizarov assisted bone transport. Emphasis is laid on strategic surgical technique coupled with functional preservation and prevention of recurrence. All patients were successfully treated without recurrences at follow-up ranging 6 months to 2 years. Functional outcomes varied depending on the location and extent of surgical dissection, but improved overall, as evident by patients’ return to routine daily activities with significant relief from pain. This case series underscores importance of a tailored, site-specific approach for managing GCT.
Conclusion: Strategic surgical intervention employed with limb-sparing technique using reconstructive surgery, highlights the potential for restoration of optimal function while minimizing the risk of recurrence. However, the diversity of GCT presentation necessitates vigilant surveillance and an individualized patient management plan.
Keywords: Proximal tibia, distal ulna, tendon sheath, functional outcomes, wrist arthrodesis, surgical management, distal radius, giant cell tumor.
Being a locally aggressive neoplasm, giant cell tumor (GCT) predominantly involves epiphysis [1] with the distal radius holding significance, representing 10% of the total cases [2]. Despite adjunctive therapies, such as phenol or liquid nitrogen, with present standard protocols of extensive curettage and reconstruction, the recurrence rates range from 5% to 17% within the initial 2 years of surgery [3,4]. Complexity of juxta-articular distal radius GCT escalates with damage to subchondral bone and articular cartilage. Reconstruction techniques utilizing structural vascularized/non-vascularized fibula/allografts or centralization of ulna with wrist arthrodesis resulted in lower recurrence rates [5,6]. Seradge’s novel technique of ulnar translocation [7] offers a locally vascularized graft, obviating the necessity for intricate microsurgical techniques with potential drawback of diminished grip strength and restricted wrist mobility. GCT of tendon sheath (GCTTS) and ganglion cyst are the most common benign tumors of hand. They are rare and present as a solitary subcutaneous nodule with incidence being higher among women in fifth decade [8]. Distal femur and proximal tibia followed by distal end of radius are the most common sites involved [1] with distal end of ulna being extremely [9]. Our case series navigates the varied presentations of GCTs at diverse locations, including the distal radius, tendon sheath, distal ulna, and proximal tibia, with focus on surgical strategies aimed at maximizing functional restoration while minimizing recurrence.
Case 1
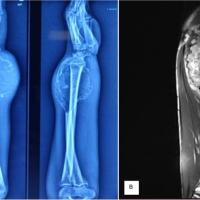
A farmer, 46-year-old male presented with swollen hands and painful wrists with limited movement for 3 months. The start of the ache was slow, dull in nature without high temperature, night sweating’s, loss of weight, and skin rash. The plane radiograph shows a lytic lesion situated eccentrically extending into the diaphysis with well-defined margins (Campanacci grade 3 Aggressive type). Lytic lesion showed trabeculations as well as cortical breakthroughs, indicating an underlying pathological process involving the distal wrist joint (Fig. 1).
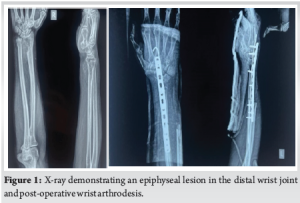
The tumor as seen on magnetic resonance imaging (MRI) is a large, fairly defined, oval shaped, sub-articular, expansile, osteolytic lesion having narrow zone of transition and involving the articular margin of right distal radio-ulnar joint (DRUJ) measuring approximately 3.37 cm × 3.40 cm × 3.15 cm. The computed tomography scan shows aggressive osteolytic lesion that presents with an exophytic component. The biopsy confirmed GCT which shows multiple soft, ash-colored pieces of tissue and blood clots. There were high number of mononuclear cells which were oval to dull, spindle-like nuclei and have a reasonable amount of eosinophilic cytoplasm. With dorsal-volar approach an incision approximately 15–20 cm was carefully crafted over the dorsal aspect of the wrist, extending from the 2nd metacarpal to the volar aspect, ensuring optimal exposure and preserving superficial radial nerve (Fig. 2a). The superficial radial nerve was found early in the procedure and carefully isolated. The dissection procedure was carefully executed, removing tumor adhesions from adjacent tissues (Fig. 2b). An important arterial structure, the radial artery, was carefully safeguarded. The tumor along with pronator quadratus muscle was removed leaving a wide safety margin of 3 cm to lower the possibility of recurrence and tumor spillage (Fig. 2c and d). An approximately 7 cm gap was created following tumor excision for ulna bone transposition without sacrificing structural integrity (Fig. 2e). To reconstruct the bone defect, a 7 cm ulna was trans-positioned with soft tissue attachment, providing the necessary structural support and vascularity (Fig. 2f).
Arthrodesis of the wrist achieved after centralizing the ulna over wrist and denuding the over lying cartilage till raw bone exposed and fixed with 2 mm Kirschner wires and a 3.5 mm 12-hole compression plate (LC-LCP) (Fig. 1), to optimize biomechanical provide patient with the best possible outcome and enhanced quality of life.
To reduce the risk of post-operative infection, dual injectable antibiotics, amikacin and cefuroxime, were used. Pain was managed with injectable analgesics. The drainage system was watched carefully to spot any signs of possible problems. The dressings were replaced on days three and six following surgery. The observation showed clean, dry wound sites, indicating a successful healing process. Once wound healed well and edema reduced gentle finger, thumb and elbow movement started after 3–4 weeks’ time. Once union visible on X-ray, gradual strengthening was started which continued till the next 3–4 months. A significant improvement in functional outcomes was noted in the patient with reduction in pain and edema at 6-month and 1 year follow-up suggesting a good recovery and rehabilitation. X-ray revealed bone fusion, proving the arthrodesis was successful. The patient also reported a satisfactory return to functional independence, improving job-related daily responsibilities and chores without any major difficulty.
Case 2
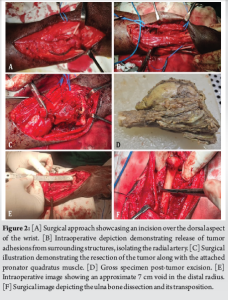
A 62-year-old woman, right-hand dominant, presented with progressive swelling over the middle phalanx of the middle finger of the right hand for the past 6 months. She also reported dull, aching pain in this area for the past 2–3 months. There was no history of trauma, swelling elsewhere, fever or weight loss. Further examination by MRI revealed soft tissue swelling originating from the flexor tendon sheath of the FDP middle finger and extending dorsally over the radial aspect. It is noteworthy that neither the digital nerve nor the artery was affected (Fig. 3).
The tumor was surgically removed and FDP tendon was preserved. Entire tumor was removed together with the tendon sheath, sparing the radial digital nerve and vessel (Fig. 4). The excised tumor sent for histopathological examination, which confirmed GCTTS. After 2 weeks, sutures were removed and supervised finger flexion and extension initiated after 1 month. The wound healed well and patient achieved a good range of motion (ROM) and strength in the affected finger at the 6-month follow-up. No recurrence of the tumor was noted at past 6-month follow-up and the patient continues to be monitored regularly. She regained the ability to perform all her activities without restrictions.
Case 3
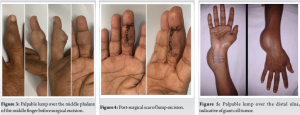
A 30-year-old housewife with a medical history complained of swelling and pain in the right wrist and distal forearm for the past 6–8 months. The swelling had gradually increased over the past 3–4 months, accompanied by pain and difficulty in performing activities of daily living (Fig. 5).

A bony tumor overlying the wrist joint and classified as Campanacci Grade III with soft tissue involvement was discovered during evaluation (Fig. 6). An en bloc excision of the distal ulna GCT with soft tissue involvement was done and confirmed by biopsy. Reconstruction was performed with an ipsilateral anterolateral thigh flap and wrist stabilized with external fixation. Intraoperatively, the tumor was found to involve multiple structures, including the FCU, ECU and EIP, which were partially removed. The tumor mass also involved the pronator quadratus, the dorsal cutaneous branch of the ulnar nerve, and the pisiform and triquetrum bones. In addition, tenodesis was performed on the proximal portion of the FCU by passing it through the distal end of the ulna and suturing it to itself. Surgery involved an en bloc excision, external fixation to stabilize the wrist, and soft tissue reconstruction using an ipsilateral anterolateral thigh flap (Fig. 5).
Once wound healed and flap was accepted, gradual finger movement was started. Once union visible on X-ray after 1.5 months, external fixation was removed and gradual wrist ROM and strengthening was started. The patient showed remarkable improvement at the 6-month follow-up, indicating a complete recovery and rehabilitation. Patient had a sufficient strength and ROM at the wrist. The degree of discomfort and edema dramatically decreased compared to pre-operative state, and ability to do daily duties also improved. There were no signs of a tumor recurrence or surgical site complications (Fig. 7).
Case 4
A 40-year-old male presented with a recurrent swelling in the left knee, which had been progressively increasing over the past year and was accompanied by pain (Fig. 8).

The patient had already undergone curettage of left proximal tibia and cementation of a GCT in another hospital a year ago which recurred and the patient was recommended an en bloc excision and reconstruction. Due to financial constraints, the patient opted for tumor excision and Illizarov-assisted bone transport. Once the appropriate length was achieved, an arthrodesis with an iliac crest bone graft was performed. Throughout the treatment, the patient remained mobile with the help of the Illizarov frame (Fig. 9).
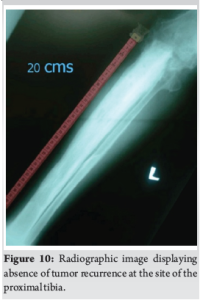
Arthrodesis was successfully achieved, and external fixator was subsequently removed. At 2 years follow-up, there were no signs of tumor recurrence. (Fig. 10).
In this case, despite the limitations, successful outcome was achieved with combination of tumor excision, Illizarov-assisted bone transport and arthrodesis with an iliac crest bone graft.
The case series emphasizes challenges in the management of GCTs subject to anatomical location with a case specific strategy aimed at optimizing functional results and reducing recurrence rate. En bloc resection of distal ulna GCT, soft tissue reconstruction in proximal tibia GCT with Illizarov-assisted bone transport for limb salvage and dorsal-volar approach for distal radius GCT were adopted. Favorable outcomes at 6-month to 2 years follow-up emphasize the potential for successful recovery, return to daily activities and the importance of continuous post-surgical monitoring in comprehensive treatment of GCTs. Despite the differences in surgical techniques for distal radius GCT opted by Agrawal’s et al. wide local excision [10], Sheth’s et al. en bloc resection [11] and our dorsal-volar approach resection with 3 cm safety margin, ulnar transposition and wrist arthrodesis, the results were comparative in all cases with excellent functional outcomes and no local recurrence at follow-up. GCTTS on the middle finger extended from flexor tendon to the dorsal side with no recurrence in contrast of Briët’s et al. volar predominance [8] and Ozben’s and Coskun theory of high recurrence [12]. Different surgical procedures pertaining distal radius GCT include Verma’s DRUJ and triangular fibrocartilage complex reconstruction after tumor excision and proximal fibula graft compression plating to proximal ulna stump for stabilization [13]; Sauve-Kapandji method [14] and en bloc excision of tumor with the affected soft tissue and stabilization using external fixation device. Recurrent GCT of proximal tibia in the series falls in contrast to Kandarkar’s et al. report [15] involving an elderly patient managed by en bloc resection, plate osteosynthesis and extensive rehabilitation, whereas our management focused on Illizarov-assisted bone transfer and arthrodesis with iliac crest bone graft, achieving optimal outcome; highlighting adaptability in orthopedic oncology subject to availability of means. Surgical success of these cases highlights the need for careful surgical planning, regular post-operative follow-up for continued monitoring and rehabilitation to ensure functional recovery. Although our case series offer valuable insights into the management of GCTs occurring at diverse anatomical location, the relatively small number may restrict the generalizability of findings, emphasizing the need of larger study populations are to support and validate procedures.
GCTs may occur at various locations, including distal radius, distal ulna, tendon sheath, and proximal tibia, highlighting the importance of specific surgical approaches tailored for each case. Favorable results mandate adequate tumor removal with sufficient margin and innovative reconstructive methods with focused rehabilitation. Thus, a multidisciplinary approach ensures restoration of function, eventually enhancing quality of life. Further research in customized surgical plans for successful management of variegated presentations of GCT.
1.Unusual GCT Location (distal ulna , tendon sheath) demand bespoke technique over generic curettage.
2.Arthrodesis reliably restores daily function despite sacrificing joint mobility
3.Ilizarov/ External Fixator offers viable limb salvage where graft/ prosthetics are inaccessible
4.Adherence to Oncological margins and soft tissue clearance is non compromisable
References
- 1. Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg Am 1987;69:106-14. [Google Scholar] [PubMed]
- 2. Salunke AA, Shah J, Warikoo V, Chakraborty A, Pokharkar H, Chen Y, et al. Giant cell tumor of distal radius treated with ulnar translocation and wrist arthrodesis: What are the functional outcomes? J Orthop Surg 2017;25:2309499016684972. [Google Scholar] [PubMed]
- 3. O’Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am 1994;76:1827-33. [Google Scholar] [PubMed]
- 4. Siddiqui MA, Seng C, Tan MH. Risk factors for recurrence of giant cell tumours of bone. J Orthop Surg (Hong Kong) 2014;22:108-10. [Google Scholar] [PubMed]
- 5. Saikia KC, Borgohain M, Bhuyan SK, Goswami S, Bora A, Ahmed F. Resection-reconstruction arthroplasty for giant cell tumor of distal radius. Indian J Orthop 2010;44:327-32. [Google Scholar] [PubMed]
- 6. Humail SM, Ghulam MK, Zaidi IH. Reconstruction of the distal radius with non-vascularised fibular graft after resection of giant cell tumour of bone. J Orthop Surg (Hong Kong) 2014;22:356-9. [Google Scholar] [PubMed]
- 7. Seradge H. Distal ulnar translocation in the treatment of giant-cell tumors of the distal end of the radius. J Bone Joint Surg Am 1982;64:67-73. [Google Scholar] [PubMed]
- 8. Briët JP, Becker SJ, Oosterhoff TC, Ring D. Giant cell tumor of tendon sheath. Arch Bone Jt Surg 2015;3:19-21. [Google Scholar] [PubMed]
- 9. Goldenberg RR, Campbell CJ, Bonfiglio M. Giant-cell tumor of bone. An analysis of two hundred and eighteen cases. J Bone Joint Surg Am 1970;52:619-64. [Google Scholar] [PubMed]
- 10. Agrawal AC, Garg AK, Choudhary R, Verma S, Dash RN. Giant cell tumor of the distal radius: Wide resection, ulna translocation with wrist arthrodesis. Cureus 2021;15:15034-10. [Google Scholar] [PubMed]
- 11. Sheth DS, Healey JH, Sobel M, Lane JM, Marcove RC. Giant cell tumor of the distal radius. J Hand Surg 1995;20:432-40. [Google Scholar] [PubMed]
- 12. Ozben H, Coskun T. Giant cell tumor of tendon sheath in the hand: Analysis of risk factors for recurrence in 50 cases. BMC Musculoskelet Disord 2019;20:457. [Google Scholar] [PubMed]
- 13. Verma A, Goyal D, Patel Y. Giant cell tumor of distal ulna – a rare case report. J Orthop Case Rep 2022;12:72-4. [Google Scholar] [PubMed]
- 14. Minami A, Iwasaki N, Nishida K, Motomiya M, Yamada K, Momma D. Giant-cell tumor of the distal ulna treated by wide resection and ulnar support reconstruction: A case report. Case Rep Med 2010;2010:871278. [Google Scholar] [PubMed]
- 15. Kandarkar MM, Jadhav S, Kandarkar SM, Vaidya S. The rare occurrence of giant cell tumor of the proximal tibia with pathological fracture in an elderly male: A case report. Cureus 2023;15:e43102. [Google Scholar] [PubMed]