Suprapectineal anatomical plate for both-column acetabular fractures may optimize anterior approaches and could set a new standard in treatment.
Dr. Sharandeep Singh Saluja, 10561, 4th floor, Lane no. 4, Pratap Nagar, New Delhi - 110007, India. E-mail: sharandoc72@gmail.com
Introduction: Acetabular fractures have increasingly become a prevalent occurrence in the field of orthopedic trauma, and their surgical management continues to present significant challenges for surgeons. The complexity and variability of these fractures often require careful consideration and expertise, making effective treatment a demanding task. Various Complex Fracture patterns, such as anterior column and posterior hemitransverse affect both the anterior and posterior columns of the acetabulum and have been traditionally treated with a combined approach of column plates and lag screw fixation techniques. The aim of this study is to assess the outcomes following fixation of both columns of complex acetabular fractures with predominant anterior displacement, using a suprapectineal plate through Anterior approach (anterior intrapelvic ± Modified Iliofemoral) in a single sitting.
Materials and Methods: A hospital-based prospective study was done on 31 patients of acetabular fracture with associated quadrilateral plate component were included in our tertiary care center during 1-year period. Patients were followed up clinically and radiologically at 4 weeks, 3 months, 6 months, and 1 year. Functional assessment was done using the Visual Analog Scale score, Harris Hip Score modified, and Merle d’Aubigné score.
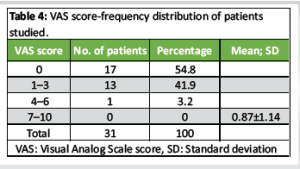
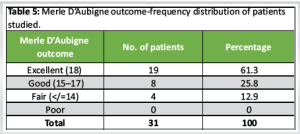
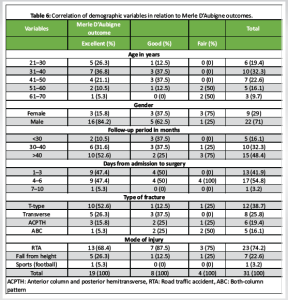
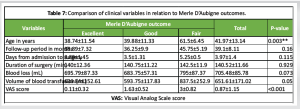
Results: 31 patients were included in the study with a mean age of 41.96 ± 13.14. Average follow-up was 39.09 ± 8.11 months. Excellent reduction with a congruent hip was achieved in all of our cases. The average intra-operative blood loss and transfusion were 705.48 ± 85.78 mL and 651.61 ± 171.01 mL, respectively. At 1-year follow-up, all fractures showed a satisfactory union with maintained reduction. Clinical outcomes at 1-year follow-up using Merle D’Aubigne and Postel grading were excellent in 61.3% cases, good in 25.8% cases, and fair in 12.9% cases. Radiologically, 2 patients had loosening of the plate from the anterior side; however, fracture had united and the patients could perform all the activities of daily living satisfactorily.
Conclusion: Complex acetabular fractures requiring both column fixations with this revolutionary anatomical plate can further push the boundaries of anterior approaches and might be a new “gold standard” for managing complex acetabular fractures in the future with further long-term results.
Keywords: Complex acetabular fracture, anterior intrapelvic, modified stoppa, suprapectineal plate, Harris Hip Score, Visual Analog Scale score, Merle d’Aubigné score.
Acetabular fractures have become more frequent, and orthopedic trauma surgeons have traditionally found it challenging to treat them surgically [1]. Early anatomical reduction and appropriate internal fixation are the cornerstones of the gold standard treatment, which permits early mobility and a speedy recovery [2,3]. Acetabular fractures consist of two main categories: Elementary and complex, each has five subcategories, giving the overall number of 10 distinctive types [4]. People older than 60 years represent the most rapidly growing population subset to encounter acetabular fractures [5], simply due to falls on the greater trochanter [6]. Many techniques widely employed in the fixation of acetabular fractures are not biomechanically validated and their reliability and mechanical stability in fixing those kinds of fractures remain unknown. About 20% of all acetabular fractures in the elderly are of the anterior column and posterior hemi-transverse (ACPHT) type [7]. Column plates and lag screw fixation procedures have historically been used in conjunction to treat this type of fracture, which affects the acetabulum’s anterior and posterior columns [8]. Nonetheless, there is ongoing debate on the best internal fixing method for ACPHT fractures [9,10]. Yildirim et al., [11] assessed a total of five different fixation methods under two loading conditions, specifically standing and sitting, through the use of a finite element model. The study’s conclusions suggested that the two-column plate fixation technique was not needed for the transverse acetabular fractures. To date, comparable research has not been conducted regarding the treatment modalities for ACPHT fractures. In the meantime, various anterior intra-pelvic surgical techniques, including modified Stoppa [12], pararectus [13], and supra-ilioinguinal [14] approaches, have resulted in the establishment of two distinct techniques for anterior column plate fixation: Suprapectineal and infrapectineal fixation [15,16]. However, it remains elusive as to which of these two techniques is better at treating ACPHT fractures. Utilizing the anterior intrapelvic (AIP)/Modified Stoppa approach allows for access to the medial wall of the acetabulum and the quadrilateral surface up to the sacroiliac joint. This technique supports the management of both columns and facilitates direct reinforcement of quadrilateral plate fractures. The treatment of complex acetabular fractures, including T-shaped, both columns, transverse, anterior, and hemi-transverse posterior fractures, as well as transitional forms, is recognized as one of the most formidable challenges faced by orthopedic surgeons. Wide experiences and clinical results of anatomically pre-contoured suprapectineal plates are still lacking in the literature. The aim of this study is to assess the outcomes following fixation of both columns of complex acetabular fractures with predominant anterior displacement, using a suprapectineal plate by anterior approach (AIP ± Modified Iliofemoral) in a Single Sitting.
A hospital-based prospective study was done on 31 patients sustaining complex acetabulum fracture with associated quadrilateral plate component in our tertiary care center from January 2019 to September 2023, and followed up till 1-year post-operatively. The study was started after obtaining ethical clearance from the Institutional Ethics Board. (IEC: F.4(63)/2019/BSAH/DNB/PF/2133).
Inclusion criteria
- All patients with acetabulum fractures with both-column pattern (ABC), the ACPHT pattern, and the T-type pattern
- Presenting within 3 weeks of injury.
Exclusion criteria
- Isolated/combined posterior column fractures
- Any surgical procedures of the hip before trauma
- Individuals with a head injury, chest trauma, polytrauma that has led to prolonged immobilization or those with a previous ipsilateral hip injury
- Patients who lost to follow-up
- Patients with co-morbidities and not fit for anesthesia
- Patients with sacral fractures/unstable pelvic ring injuries.
Operative technique
A uniform surgical plan was utilized in all the patients. Both pre-operative and post-operative assessments included routine X-rays, Judet views, computed tomography scans, three-dimensional (3D) reconstructions, and Doppler ultrasounds of the pelvic region and lower limbs. In each case, a senior surgeon carried out the surgical approach utilizing the AIP/modified Stoppa [17] approach with or without a modified ileofemoral approach. Patients were kept in the supine position with the hip flexed up to 30° and a Schanz screw was placed in the femoral neck for lateral traction. Notably, we augmented the pelvic view associated with the iliofemoral approach by utilizing a typical 10-cm horizontal Pfannenstiel incision, which is kept two finger breadths above the pubic symphysis. Thereafter, we ensure the protection of the spermatic cord or round ligament, remove the rectus insertion from the pubis, and incise the transversalis fascia superior to the pubic symphysis to access the retropubic space of Retzius [18]. The identification and ligation of the corona mortis, as well as the protection of the obturator nerve and femoral vascular bundle, were successfully achieved. The ileopectineal fascia was incised, followed by lifting up of the iliacus from the pelvic brim, and the fracture site was exposed after dissection along the quadrilateral plate. The steps of the surgical approach are depicted in Fig. 1 and 2. Following adequate exposure up to the sacro-iliac joint, the fracture reduction was performed under direct visualization using a pelvic clamp, with the option of employing K-wires or lag screws as required. The application of an anatomical pre-contoured suprapectineal plate along the pelvic brim was implemented to deliver essential mechanical support for the stabilization of acetabular fractures. Additional fixation with screws or recon plates was done wherever needed. The reduction was checked under C-arm. Closure was done in layers with meticulous handling of the rectus.


Follow-up
All cases conformed to the same post-operative rehabilitation protocol and were allowed to bear full weight 6 weeks after the surgery. Clinical and radiographic assessments were conducted at 4 weeks, 3 months, 6 months, and 1 year. Following at least 24 months of follow-up, patients revisited the clinic for a comprehensive re-evaluation, which involved a physical examination, the completion of quality-of-life surveys, and a radiographic evaluation. The assessment of functional status involved the application of the Visual Analog Scale score (VAS), the modified Harris hip score (HHS), and the Merle d’Aubigné score. The Matta radiographic criteria offer a practical, rapid, and efficient method for evaluating and categorizing the radiological results of surgical interventions for acetabular fractures [19].
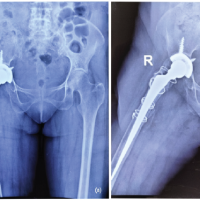
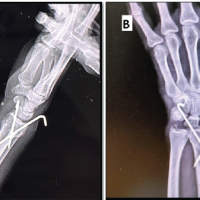
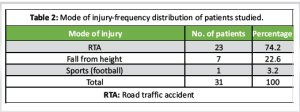
31 patients were included in the study with a mean age of 41.96 ± 13.14. Mean follow-up was 41.96 ± 13.14 months. The data regarding demographic and clinical profile of patients along with mode of injury are shown in Tables 1 and 2. The quadrilateral plate was involved in all cases. Eight transverse, 5 ABC, 12 T-type, and 6 anterior column and posterior hemitransverse fractures were operated using an anterior approach in a single sitting through suprapectineal plate and reconstruction plates for fixation of both columns. Of these, 8 were operated using a single AIP (Fig. 3) and the rest of the 23 fractures required an additional modified ileofemoral approach with anterior superior iliac spine osteotomy (Fig. 4). All cases adhered to the same post-operative rehabilitation protocol, permitting weight-bearing activities to commence with toe-touch at 2 weeks, progressing to gradual and full weight-bearing by 12 weeks post-surgery.
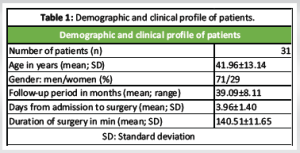
HHS modified (Table 3), VAS (Table 4), and Merle d’Aubigné (Table 5) score were used to assess the functional status. Follow-up assessments for patients were conducted at 4 weeks, 3 months, 6 months, and 1 year. Excellent reduction with a congruent hip was achieved in all of our cases. The mean blood loss during the operation was recorded at 705.48 ± 85.78 mL, while the average volume of transfusion was 651.61 ± 171.01 mL. After 1 year of follow-up, all fractures exhibited successful union while maintaining their reduction. Clinical outcomes at 1-year follow-up using Merle D’Aubigne and Postel grading were excellent in 61.3% cases, good in 25.8% cases, and fair in 12.9% cases. Tables 6 and 7 depict the correlation of demographic variables and comparison of clinical variables in relation to Merle D’Aubigne outcomes in the study patients.
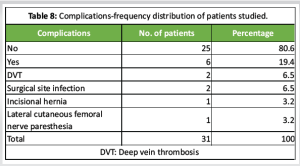
Complications were encountered in 6 patients clinically (Table 8). 2 cases had deep vein thrombosis which settled with medications. 2 patients had surgical site infections of which 1 patient had a superficial infection that settled with antibiotics and serial wound dressings, while the other patient needed surgical debridement, following which the wound healed satisfactorily. 1 patient had an incisional hernia at the AIP incision site, which healed through granulation tissue and secondary intention after application of a negative pressure wound therapy device followed by closure. Paresthesia along the lateral femoral cutaneous nerve of the thigh was noted in 1 patient, which required an additional modified ileofemoral approach. Radiologically, 2 patients had loosening of the plate from the anterior side; however, fracture had united and the patients could perform all the activities of daily living satisfactorily.
We planned for implant removal in 3 of our cases because 2 patients had implant loosening and 1 patient complained of discharge from the wound site.
Due to the high rate of unsatisfactory outcomes after conservative treatment, complex and displaced acetabular fractures typically require open reduction and internal fixation [19]. Managing fractures of this nature presents a considerable challenge for trauma surgeons due to the deep anatomical positions where these injuries occur, coupled with the intricate and complex anatomy of the surrounding structures with direct proximity, such as major blood vessels and uro-genital organs. This makes the surgical intervention not only more complicated but also heightens the risk of complications during the healing process. In the course of our comprehensive study, we made use of an anatomical plate that was specifically designed to incorporate both suprapectineal and infrapectineal holes. This innovative plate was further enhanced by the addition of a 90° bent triangular component, which was strategically placed on the inner side of the primary plate to provide additional support and stability. This triangular element on a quadrilateral surface serves to link the anterior and posterior sections, integrating the benefits of suprapectineal and infrapectineal plating to enhance both reduction and stability. Furthermore, as demonstrated by Culemann et al., [20] we frequently positioned an infra-acetabular long screw between both columns to accomplish the objectives of perfect reduction, compression, and stiff fixation. According to the present study’s clinical findings, only a small percentage of patients required walking assistance, and 96.7% of patients expressed satisfaction with their condition during day-to-day activities. Furthermore, employing the Merle D’Aubignè scoring system alongside the HHS, 87.1% of patients were classified as having good or excellent outcomes. Our findings are consistent with those reported in prior researches [21-23]. Hirvensalo et al., [21] found that 80% of 164 patients had HHS of 75 or higher on clinical examination. Sagi et al., [12] conducted a study in which they utilized the Merle D’Aubigné scoring system to evaluate the outcomes of various patients. Their findings revealed that a significant 88% of the patients were ultimately classified as either good or excellent in terms of their results. According to Laflamme et al., [23] 92.9% and 70.6% of their patients achieved ratings of good or excellent, as assessed by the Merle D’Aubignè score and the HHS, respectively. In a study conducted by Yao et al., [24] it was reported that an impressive 87.5% of the patients in their analysis were rated as either having achieved a good outcome or an excellent one. Several authors, such as Sagi et al., [12] Andersen et al., [8] and Hirvensalo et al., [21] have reported the results of a large series of patients operated on using the modified Stoppa approach and demonstrated satisfactory reduction in 92%, 82%, and 84% of patients, respectively. Achieving proper anatomical alignment, particularly in the upper weight-bearing area of the acetabulum, can lead to good or excellent functional results in 83–89% of patients. Our complication rate and the time required for surgery are comparable to those reported in the literature by other studies and medical professionals. It is important to highlight that the process of removing hardware is a significant challenge and demands considerable effort. Given these factors, we strongly recommend that hardware removal should only be considered when it is absolutely necessary and only where benefits outweigh the risks. The present study has a few limitations. The study’s small sample size limits statistical power, potentially affecting the reliability of its conclusions. A larger sample would improve the robustness and validity of the findings by better capturing population variability. Future multi-center studies should compare Stoppa’s suprapectineal plate approach with conventional reconstruction plates.
Complex acetabular fractures with predominant anterior displacement requiring fixation of both columns using the anterior approach in a single sitting through suprapectineal plate gives excellent to good outcomes in the majority of cases with less morbidity without any additional learning. Both column fixation with this revolutionary anatomical plate can further push the boundaries of anterior approaches and might be a new “gold standard” for managing complex acetabular fractures in the future with further long-term results.
Anterior approach using a suprapectineal anatomical plate allows effective single-stage fixation of both columns in complex acetabular fractures with anterior displacement, providing excellent to good outcomes and reduced morbidity. This technique shows promise as a future gold standard, pending validation by long-term results.
References
- 1. Guo J, Dong W, Zhou Y, Hu J, Ye P, Chen W, et al. Differences in fixation to young and elderly quadrilateral surfaces with anatomic quadrilateral surface plate (AQSP) based on cortical thickness morphological results. J Orthop Surg Res 2022;17:143. [Google Scholar] [PubMed]
- 2. Märdian S, Schaser KD, Hinz P, Wittenberg S, Haas NP, Schwabe P. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: A direct comparison. Bone Joint J 2015;97-B:1271-8. [Google Scholar] [PubMed]
- 3. Chen K, Yang F, Yao S, Xiong Z, Sun T, Zhu F, et al. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res 2019;105:877-84. [Google Scholar] [PubMed]
- 4. Letournel E, Judet R. Fractures of the Acetabulum. New York: Springer; 1981. [Google Scholar] [PubMed]
- 5. Lonner JH, Koval KJ. Polytrauma in the elderly. Clin Orthop Relat Res 1995;318:136-43. [Google Scholar] [PubMed]
- 6. Helfet DL, Borrelli J Jr., DiPasquale T, Sanders R. Stabilization of acetabular fractures in elderly patients. J Bone Joint Surg Am 1992;74:753-65. [Google Scholar] [PubMed]
- 7. Butterwick D, Papp S, Gofton W, Liew A, Beaulé PE. Acetabular fractures in the elderly: Evaluation and management. J Bone Joint Surg Am 2015;97:758-68. [Google Scholar] [PubMed]
- 8. Andersen RC, O’Toole RV, Nascone JW, Sciadini MF, Frisch HM, Turen CW. Modified stoppa approach for acetabular fractures with anterior and posterior column displacement: Quantification of radiographic reduction and analysis of interobserver variability. J Orthop Trauma 2010;24:271-8. [Google Scholar] [PubMed]
- 9. May C, Egloff M, Butscher A, Keel MJ, Aebi T, Siebenrock KA, et al. Comparison of fixation techniques for acetabular fractures involving the anterior column with disruption of the quadrilateral plate: A biomechanical study. J Bone Joint Surg Am 2018;100:1047-54. [Google Scholar] [PubMed]
- 10. Chen K, Yang F, Yao S, Xiong Z, Sun T, Guo X. Biomechanical comparison of different fixation techniques for typical acetabular fractures in the elderly: The role of special quadrilateral surface buttress plates. J Bone Joint Surg Am 2020;102:e81. [Google Scholar] [PubMed]
- 11. Yildirim AO, Alemdaroglu KB, Yuksel HY, Öken ÖF, Ucaner A. Finite element analysis of the stability of transverse acetabular fractures in standing and sitting positions by different fixation options. Injury 2015;46:S29-35. [Google Scholar] [PubMed]
- 12. Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma 2010;24:263-70. [Google Scholar] [PubMed]
- 13. Keel MJ, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Büchler L, et al. The pararectus approach for anterior intrapelvic management of acetabular fractures: An anatomical study and clinical evaluation. J Bone Joint Surg Br 2012;94:405-11. [Google Scholar] [PubMed]
- 14. Chen K, Ji Y, Huang Z, Navinduth R, Yang F, Sun T, et al. Single modified ilioinguinal approach for the treatment of acetabular fractures involving both columns. J Orthop Trauma 2018;32:e428-34. [Google Scholar] [PubMed]
- 15. Yücens M, Alemdaroğlu KB, Özmeriç A, İltar S, Yıldırım AÖ, Aydoğan NH. A comparative biomechanical analysis of suprapectineal and infrapectineal fixation on acetabular anterior column fracture by finite element modeling. Turk J Med Sci 2019;49:442-8. [Google Scholar] [PubMed]
- 16. Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: A technical adjunct to internal fixation. J Orthop Trauma 2004;18:175-8. [Google Scholar] [PubMed]
- 17. Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res 1994;305:112-23. [Google Scholar] [PubMed]
- 18. Tannast M, Keel MJ, Siebenrock KA, Bastian JD. Open reduction and internal fixation of acetabular fractures using the modified stoppa approach. JBJS Essent Surg Tech 2019;9:e3. [Google Scholar] [PubMed]
- 19. Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res 1988;230:83-97. [Google Scholar] [PubMed]
- 20. Culemann U, Marintschev I, Gras F, Pohlemann T. Infra-acetabular corridor–technical tip for an additional screw placement to increase the fixation strength of acetabular fractures. J Trauma 2011;70:244-6. [Google Scholar] [PubMed]
- 21. Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res 1993;297:28-32. [Google Scholar] [PubMed]
- 22. Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury 2011;42:1130-4. [Google Scholar] [PubMed]
- 23. Yao S, Chen K, Ji Y, Zhu F, Zeng L, Xiong Z, et al. Supra-ilioinguinal versus modified stoppa approach in the treatment of acetabular fractures: Reduction quality and early clinical results of a retrospective study. J Orthop Surg Res 2019;14:364. [Google Scholar] [PubMed]
- 24. Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br 2005;87:2-9. [Google Scholar] [PubMed]