Bilateral scaphoid fractures are uncommon and often the result of high-energy trauma. To diagnose these fractures, a high index of suspicion with good clinical examination and radiological correlation is required. Timely and appropriate management is important in minimizing the risk of complications and facilitating recovery. Operative treatment has better outcomes than conservative management
Dr. Bharat Kumar Soni, Department of Orthopaedics, All India Institute of Medical Sciences, Marudhar Industrial Area, 2nd Phase, M.I.A. 1st Phase, Basni, Jodhpur - 342005, Rajasthan, India. E-mail: bsoni9863@gmail.com
Introduction: The most frequent carpal bone fractures are scaphoid fractures, which frequently affect young people, particularly athletes. These fractures can be difficult to identify, and if left untreated, they can cause problems, including non-union. Although they are uncommon, high-energy trauma can result in bilateral scaphoid fractures, and related injuries can make treatment more difficult.
Case Report: A 20-year-old male who had fallen on an outstretched hand from a tractor appeared with pain, edema, and deformity in both wrists and the left elbow. Upon examination, the scaphoid compression test came back positive on both sides, and there was discomfort in the anatomical snuff box. Bilateral scaphoid fractures, a transcaphoid, trans-triquetrum perilunate dislocation on the left, and a Regan-Moorey II coronoid fracture were discovered by X-ray and computed tomography (CT) scans. The perilunate dislocation was repaired during the surgical procedure, and both scaphoid fractures were internally fixed with headless compression (Herbert) screws. At 6-month follow-up, the fractures had successfully united, and the patient regained full wrist functionality. This case underscores the importance of early diagnosis and surgical intervention for scaphoid fractures to prevent complications.
Conclusion: High clinical suspicion and quick radiographic assessment are necessary for scaphoid fractures. In addition to improving results, early surgical fixation lowers the chance of non-union and other issues. For precise diagnosis and surgical planning, CT scans are necessary.
Keywords: Scaphoid, traumatic, headless compression screw, avascular necrosis, union.
The scaphoid is the most common carpal bone to fracture as a result of a fall on an outstretched hand, predominantly seen in males. Bilateral scaphoid fractures are rare and considered challenging because they compromise both wrists, making rehabilitation more complex. The median age of males was significantly younger compared to females. Hebert B2 was the most common type seen [1]. To ensure early diagnosis and effective management of scaphoid fractures, it is crucial to maintain a high index of suspicion and utilize X-rays and computed tomography (CT) scans. This approach helps prevent complications such as non-union, osteoarthritis, chronic pain, and reduced range of motion (ROM) [2]. In this report, we present a rare case of bilateral traumatic scaphoid fracture following a fall on an outstretched hand managed surgically with a headless compression screw. This work was completed in line with Surgical Case Report guidelines [3].
A 20-year-old male presented to an orthopedics emergency at our tertiary care center with pain, swelling, and deformity of the left wrist and left elbow, and pain in the right wrist following an alleged history of a fall on the outstretched hand from the tractor. He had no significant past medical or surgical history and was apparently normal before the injury.
On examination, there was tenderness in the anatomical snuff box on both sides, and the scaphoid compression test was positive bilaterally. There was a significant restriction in the movements of both wrists. He was evaluated with X-rays (Fig. 1) and CT (Fig. 2) of the bilateral wrist and was diagnosed as a case of bilateral closed scaphoid fracture (Herbert type B4 on the left side and type B2 on the right side) with transcaphoid, trans-triquetrum perilunate dislocation on the left side and coronoid fracture (Regan-Moorey II) on the left side (Fig. 3). Closed reduction of perilunate dislocation was done in an emergency under local anesthesia, and a bilateral glass holding slab was applied for scaphoid fracture. While the patient had no prior comorbidities, bone health markers such as serum calcium and Vitamin D levels were evaluated and found to be within the normal range. The patient had no history of smoking or alcohol consumption. These may be important determinants of healing, particularly in older or systemically compromised individuals.
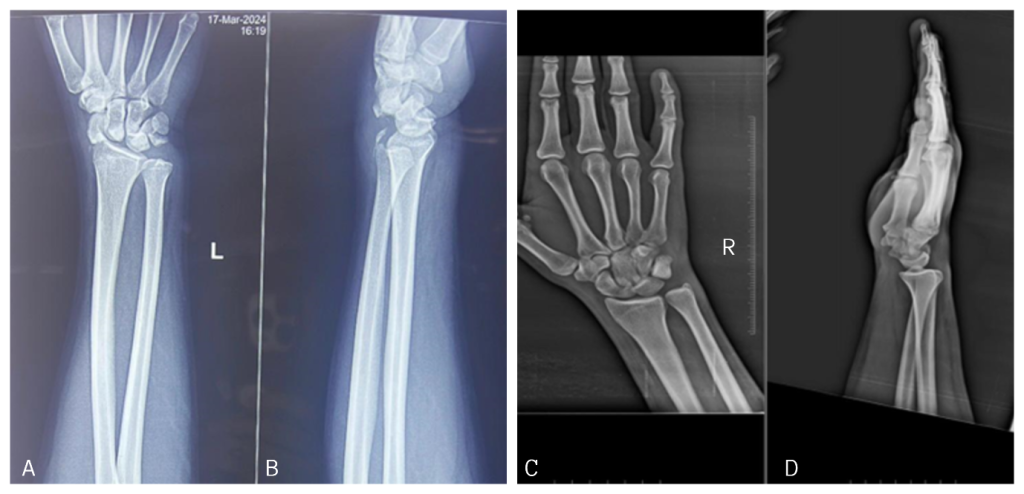
Figure 1: Pre-operative X-rays of the bilateral wrist. Anteroposterior (a) and lateral (b) view of the left wrist. Anteroposterior (c) and lateral (d) view of the right wrist.
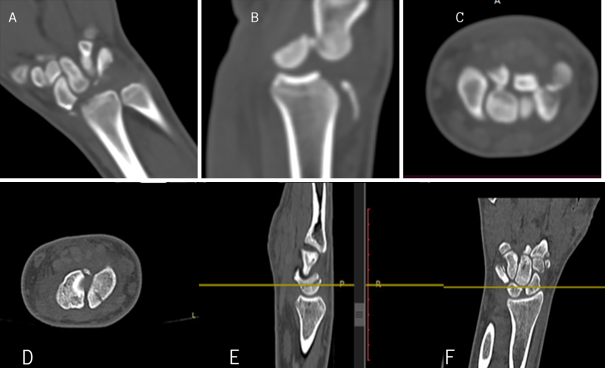
Figure 2: Computed tomography (CT) of left wrist showing scaphoid fracture in coronal (a), sagittal (b), and axial (c) sections. CT of right wrist showing scaphoid fracture in axial (d), sagittal (e), and coronal (f) sections.
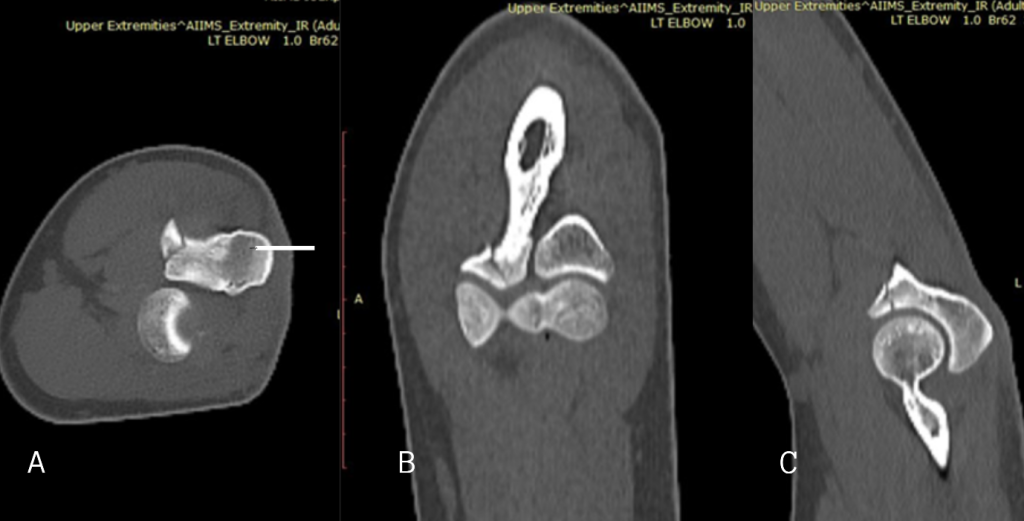
Figure 3: Computed tomography left elbow showing Regan-Moorey II coronoid process fracture in axial (a), coronal (b), and sagittal (c) section.
He was planned for and underwent closed reduction and internal fixation with one headless compression (Herbert) screw (Titanium, 2.7 mm) for left scaphoid fracture and closed reduction and internal fixation with one Herbert screw (Titanium, 3.5 mm) for right scaphoid fracture (Fig. 4). A volar approach was used bilaterally. Under fluoroscopic guidance, Herbert screws (2.7 mm on the left and 3.5 mm on the right) were inserted following pre-drilling and countersinking. Screw trajectory was central, ensuring optimal compression across the fracture plane. Screw positioning was confirmed intraoperatively. Bone quality was good, and there was no need for bone grafting. No intraoperative complications occurred. The bilateral nature of the scaphoid fractures also increased operative time and required special attention to patient positioning, draping, and access, as both upper limbs were involved. In addition, significant soft-tissue edema from the high-energy trauma made dissection and exposure more difficult and increased the risk of soft-tissue complications.

Figure 4: Post-operative X-rays of bilateral wrist with bilateral scaphoid fixation with Herbert screw. Anteroposterior (a) and lateral (b) view of left wrist and anteroposterior (c) and lateral (d) view of right wrist.
Patient was allowed with wrist mobilization after 4 weeks, and follow-up X-rays were done on subsequent visits to the outpatient department. Six-month follow-up X-rays show union in the bilateral scaphoid (Fig. 5). Clinically, the patient was able to carry out daily activities without pain. Grip strength was assessed using a dynamometer, and at 12-month follow-up, was found to be 90% of normal bilaterally. Functional assessment was performed using QuickDASH, Mayo Wrist score, and wrist ROM measured via goniometer. (Table 1) Our follow-up period was limited to 12 months. While this showed satisfactory union and functional outcomes, scaphoid-related complications such as avascular necrosis (AVN) and post-traumatic arthritis often manifest over longer durations. Continued monitoring is advised.
 Figure 5: A 6-month follow-up X-ray of the bilateral wrist. Anteroposterior (a) view, lateral (b) and scaphoid (c) view.
Figure 5: A 6-month follow-up X-ray of the bilateral wrist. Anteroposterior (a) view, lateral (b) and scaphoid (c) view.
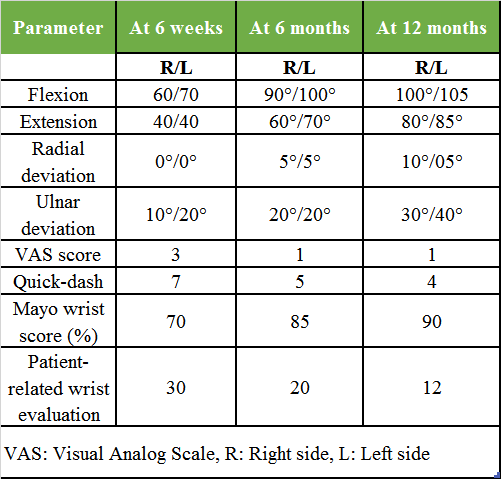 Table 1: Clinical parameters and functional score at 12 months follow-up
Table 1: Clinical parameters and functional score at 12 months follow-up
A 12-month follow-up, radiological evaluation using X-rays (Fig. 6), and CT confirmed complete union of the scaphoid fractures. Objective assessment revealed 100% trabecular bridging across the fracture sites in coronal, sagittal, and axial planes (Fig. 7), which is considered the gold standard indicator of union following internal fixation of scaphoid fractures [4]. According to the CT-based grading system, this finding corresponds to Grade 4, indicating complete osseous healing [5]. Furthermore, based on the scaphoid fracture healing score, the patient achieved the maximum score of 10, reflecting optimal bone consolidation and structural integrity [6]. These objective measures provided strong evidence of successful healing, allowing for full return to functional activities.
 Figure 6: A 12-month follow-up X-ray of the bilateral wrist. Anteroposterior (a) view, and scaphoid (b) of the bilateral wrist.
Figure 6: A 12-month follow-up X-ray of the bilateral wrist. Anteroposterior (a) view, and scaphoid (b) of the bilateral wrist.
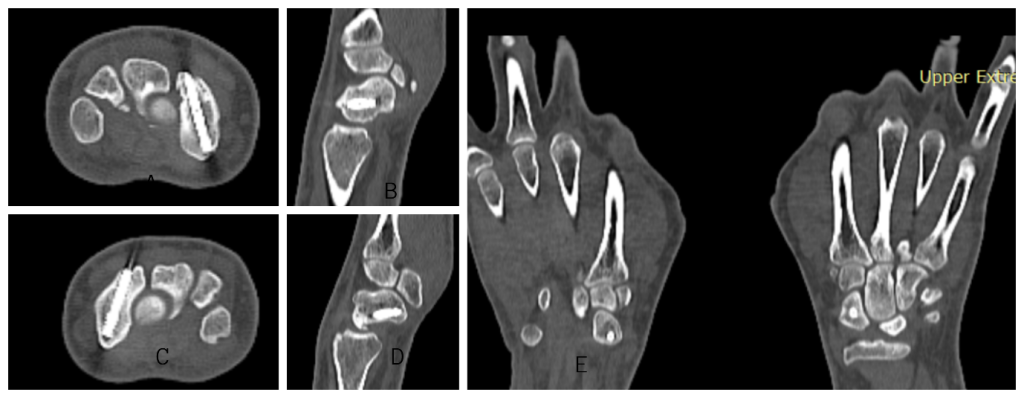 Figure 7: A 12-month follow-up computed tomography showing complete bony union of left side axial and sagittal view (a and b), right side axial and sagittal view (c and d), and Coronal view (e).
Figure 7: A 12-month follow-up computed tomography showing complete bony union of left side axial and sagittal view (a and b), right side axial and sagittal view (c and d), and Coronal view (e).
The wrist ROM was measured using a goniometer at 6 weeks, 6 months, and 12 months follow-up (Fig. 8).
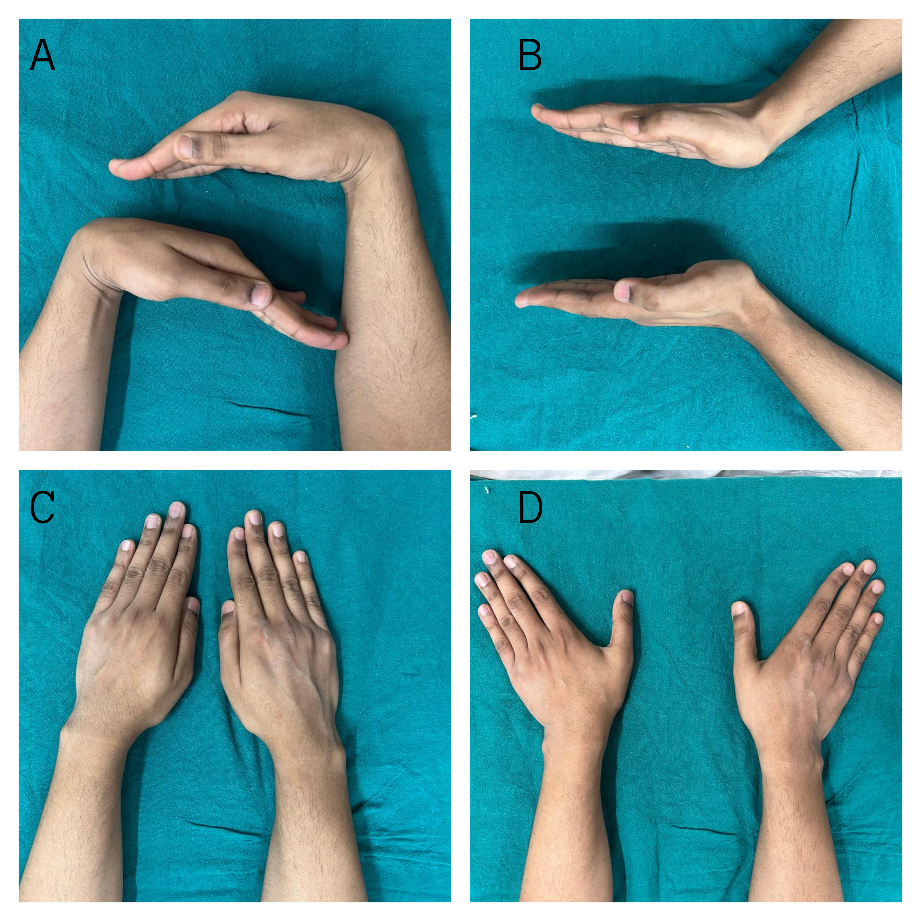
Figure 8: 12-month follow-up clinical pictures.
The scaphoid is the most frequently fractured carpal bone, representing 60% of all carpal fractures [7] and 2.4% of all wrist fractures [8]. It is the largest bone in the proximal carpal row, which facilitates the transfer of load from the hand to the forearm and plays a crucial role in maintaining wrist stability. Scaphoid fractures are more common in young athletes and are less common in the pediatric age group [9]. Fractures of the scaphoid can be categorized into two primary mechanisms: traumatic and stress-induced. The typical cause is a fall onto an outstretched hand, resulting in forceful hyperextension of the wrist [10].
Clinically, they are suspected if there is tenderness in the anatomical snuff box. The scaphoid compression test, as described by Chen [11], has higher sensitivity and specificity for scaphoid fracture. These fractures are commonly missed on X-rays. The “scaphoid view” with wrist pronated in ulnar deviation and X-ray beam 25° off vertical, direct cephalad can be used to visualize the scaphoid more clearly. A CT scan is used for diagnosis, and some studies have described the accuracy of new modalities such as 3D printing in diagnosing and surgical planning [12]. Scaphoid fractures are classified according to Herbert [13] into four types.
Bilateral simultaneous scaphoid fractures are rare [14] and have been infrequently reported in the literature. (Table 2) The occurrence of bilateral scaphoid fractures can significantly diminish patients’ quality of life, impair functionality, and impose limitations on basic activities of daily living, such as dressing, grooming, and household tasks, but also sports activities and hobbies, thereby highlighting the importance of prompt diagnosis and comprehensive treatment to optimize recovery and minimize disability. They are most commonly (68.75%) associated with other wrist injuries, such as bilateral distal end radius fractures and bilateral non-scaphoid carpal bone fractures [15].
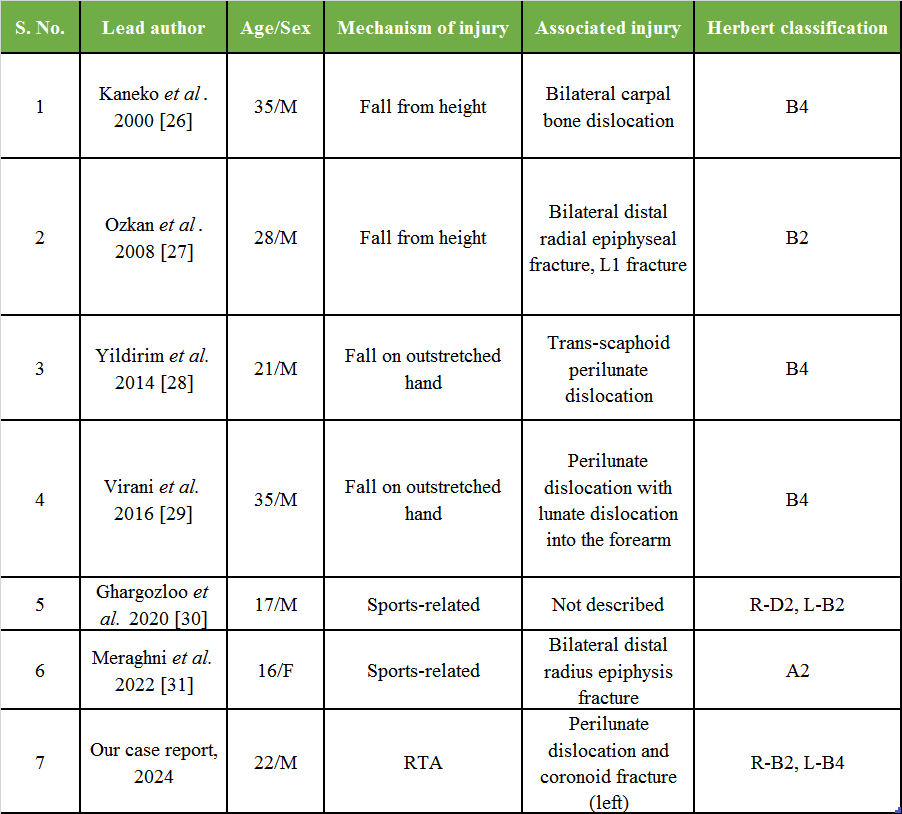
Table 2: Review of previous cases with bilateral traumatic scaphoid fracture managed surgically with headless compression screw
Our analysis revealed a variety of traumatic mechanisms leading to bilateral scaphoid fractures, with falls from height being the most common cause (37.50%). Only 12.50% were due to acute injuries during sports activities. This contrasts with the pattern seen in unilateral scaphoid fractures, where sports-related injuries are more typical [1]. Even when considering stress fractures associated with sports, falls from height remain the predominant cause of bilateral injuries. In literature, bilateral scaphoid fractures typically occur from significant axial loading, often due to falling on both outstretched hands, force transmission through wrists while holding a bike handle [16], steering wheel [14], or during high-impact trauma.
Fractures involving the proximal pole of the scaphoid have the highest chance of non-union (30–40%), followed by the scaphoid waist (10–20%) due to its retrograde blood supply [17]. Early diagnosis and treatment are necessary since delayed treatment by 4 weeks can increase the risk of non-union as high as 40% compared to 3% when treated within 4 weeks [18]. Scaphoid non-union, advanced collapse arthritis is a complication of neglected scaphoid fractures. Immediate emergency management includes immobilization with a glass holding slab. Non-displaced and stable fractures can be managed by immobilization alone. A fracture gap of 1 mm or less on an anteroposterior view, lunate-capitate angle <15°, and scapholunate angle <60° on a lateral view is described as displacement by Cooney et al. [19]. A meta-analysis by Al-Ajmi et al. showed that surgical fixation can decrease the rate of non-union [20]. Thus, while our results support surgical treatment, we acknowledge that stable fractures may still be managed conservatively, and randomized comparative trials are warranted in bilateral cases.
Surgical management includes fixation with Herbert screws, or Kirschner wires can also be used. Both dorsal and volar approaches can be used for percutaneous fixation for undisplaced or minimally displaced fractures. Alternative fixation methods, such as Kirschner wires or volar locking plates, have been described, especially in pediatric or osteoporotic bone. However, these methods may require longer immobilization and pose higher risks of displacement. In our case, Herbert screw fixation allowed early mobilization with excellent union. D’Itri et al. did a systematic review in 2024 and concluded a lower complication rate in surgically treated patients as compared to the conservative group, especially because most surgically treated fractures commonly exhibit a pattern of greater instability and/or associated injuries. As per current literature, even for acute displaced scaphoid fractures, percutaneous fixation is preferred due to decreased violation of volar ligaments, preventing carpal instability, preserving blood supply from surgical trauma in open fixation, and minimizing the risk of delayed union or non-union [20-23]. Although surgical intervention yielded excellent outcomes in this case, conservative treatment remains the standard for stable, non-displaced scaphoid fractures. The absence of a comparative conservative cohort limits our ability to conclusively advocate operative treatment in all bilateral cases. Future comparative studies would be beneficial. After several years of follow-up, magnetic imaging resonance (MRI) can also be used to assess the vascular status of the scaphoid, particularly the proximal pole, which is most susceptible to AVN. The MRI-based Schmitt grading system is used for scaphoid AVN [24]. Most fracture types can be approached dorsally, although humpback deformity requires a volar approach. Complications of these approaches include scaphotrapezial arthritis following the volar approach and increased risk of extensor pollicis longus tendon injury via the dorsal approach [25]. As this is a single-patient case report, findings should be interpreted with caution. While valuable insights are offered, generalizability is inherently limited. Larger prospective or comparative studies are necessary to validate the effectiveness of the surgical approach across diverse populations. Immobilization of both wrists posed significant functional limitations for the patient, impacting activities of daily living and requiring considerable caregiver support. This dependence can lead to frustration, reduced compliance, and even psychological stress, highlighting the importance of incorporating psychosocial support and counselling into the rehabilitation plan. Pain management was also more complex due to bilateral upper limb involvement. Therefore, rehabilitation must be more gradual and cautiously advanced to prevent overuse or strain on healing structures.
Bilateral scaphoid fractures are uncommon in the literature and have been documented in only a limited case reports that have been published. This type of injury is often the result of high-energy trauma. A high index of suspicion with good clinical examination and radiological correlation is required to diagnose scaphoid fractures. Timely and appropriate management strategies are paramount in minimizing the risk of complications and facilitating optimal recovery in these cases. Although literature on this topic is still limited, operative treatment has better outcomes than conservative management. Our case report aims to highlight the possibility that these fractures may happen more frequently due to the increasingly common occurrence of high-energy trauma.
Bilateral scaphoid fractures are uncommon and often the result of high-energy trauma. A high index of suspicion with good clinical examination and radiological correlation is required to diagnose scaphoid fractures. Timely and appropriate management strategies are paramount in minimizing the risk of complications and facilitating optimal recovery. Although literature on this topic is still limited, operative treatment has better outcomes than conservative management.
References
- 1. Jørgsholm P, Ossowski D, Thomsen N, Björkman A. Epidemiology of scaphoid fractures and non-unions: A systematic review. Handchir•Mikrochir Plast Chir 2020;52:374-81. [Google Scholar] [PubMed]
- 2. Patrick CN. Diagnosis and treatment of scaphoid fractures. Radiol Technol 2010;82:161-76. [Google Scholar] [PubMed]
- 3. Sohrabi C, Mathew G, Maria N, Kerwan A, Franchi T, Agha RA. The SCARE 2023 guideline: Updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 2023;109:1136-40. [Google Scholar] [PubMed]
- 4. Buijze GA, Juttmann JW, Haak MH, Ring D, Marsman M, Dijkman BG. Diagnostic performance of computed tomography compared with radiography for suspected scaphoid fractures: A meta-analysis. J Bone Joint Surg Am 2010;92:1230-7. [Google Scholar] [PubMed]
- 5. Singh HP, Forward DP, Davis TR, Dawson JS, Oni JA, Foster MA. The conservative management of acute scaphoid fractures: A 5-year review. J Bone Joint Surg Br 2006;88:1533-7. [Google Scholar] [PubMed]
- 6. Mallee WH, Doornberg JN, Ring D, van Dijk CN, Maas M, Goslings JC, et al. Computed tomography for the diagnosis of suspected scaphoid fractures: A cost-effectiveness analysis. J Bone Joint Surg Am 2011;93:20-28. [Google Scholar] [PubMed]
- 7. Testa G, Lucenti L, D’Amato S, Sorrentino M, Cosentino P, Vescio A, et al. Comparison between vascular and non-vascular bone grafting in scaphoid nonunion: A systematic review. J Clin Med 2022;11:3402. [Google Scholar] [PubMed]
- 8. Van Tassel DC, Owens BD, Wolf JM. Incidence estimates and demographics of scaphoid fracture in the US population. J Hand Surg 2010;35:1242-5. [Google Scholar] [PubMed]
- 9. Winston MJ, Weiland AJ. Scaphoid fractures in the athlete. Curr Rev Musculoskelet Med 2017;10:38-44. [Google Scholar] [PubMed]
- 10. Hayat Z, Varacallo M. Scaphoid wrist fracture. StatPearls. Treasure Island, FL, USA: StatPearls Publishing; 2023. [Google Scholar] [PubMed]
- 11. Chen SC. The scaphoid compression test. J Hand Surg Br 1989;14:323-5. [Google Scholar] [PubMed]
- 12. Lebowitz C, Massaglia J, Hoffman C, Lucenti L, Dheer S, Rivlin M, et al. The accuracy of 3D printed carpal bones generated from cadaveric specimens. Arch Bone Joint Surg 2021;9:432-8. [Google Scholar] [PubMed]
- 13. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br 1984;66:114-23. [Google Scholar] [PubMed]
- 14. Kattan AE, Almarghoub MA, Alnujaim NH, Barasain O, AlLababidi NH. Bilateral scaphoid fractures: Case report and literature review. Int J Surg Case Rep 2020;66:412-5. [Google Scholar] [PubMed]
- 15. D’Itri L, Gattuso MS, Cobisi CD, Ferruzza M, Lucenti L, Camarda L. Bilateral scaphoid fractures: A systematic literature review. J Pers Med 2024;14:424. [Google Scholar] [PubMed]
- 16. Umashree T, Sarin P. Traumatic bilateral scaphoid fracture-a case report. J Clin Exp Orthop 2018;4:51. [Google Scholar] [PubMed]
- 17. Adam JR, Woodruff MJ. Acute scaphoid fractures and non-unions. Orthop Trauma 2017;31:257-65. [Google Scholar] [PubMed]
- 18. Langhoff O, Andersen JL. Consequences of late immobilization of scaphoid fracture. J Hand Surg Br 1988;13:77-9. [Google Scholar] [PubMed]
- 19. Cooney WP, Dobyns JH, Linscheid RL. Fractures of the scaphoid: A rational approach to management. Clin Orthop Relat Res 1980;149:90-7. [Google Scholar] [PubMed]
- 20. Al-Ajmi TA, Al-Faryan KH, Al-Kanaan NF, Al-Khodair AA, Al-Faryan TH, Al-Oraini MI, et al. A systematic review and meta-analysis of randomized controlled trials comparing surgical versus conservative treatments for acute undisplaced or minimally-displaced scaphoid fractures. Clin Orthop Surg 2018;10:64-73. [Google Scholar] [PubMed]
- 21. Filan SL, Herbert TJ. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Br 1996;78:519-29. [Google Scholar] [PubMed]
- 22. Garcia-Elias M, Vall A, Salo JM, Lluch AL. Carpal alignment after different surgical approaches to the scaphoid: A comparative study. J Hand Surg 1988;13:604-12. [Google Scholar] [PubMed]
- 23. Botte MJ, Mortensen WW, Gelberman RH, Rhoades CE, Gellman H. Internal vascularity of the scaphoid in cadavers after insertion of the Herbert screw. J Hand Surg 1988;13:216-20. [Google Scholar] [PubMed]
- 24. Schmitt R, Christopoulos G, Meier R, Heller M, Lanz U. MRI for detection and classification of avascular necrosis in scaphoid nonunion. AJR Am J Roentgenol 2005;185:732-7. [Google Scholar] [PubMed]
- 25. Geurts G, van Riet R, Meermans G, Verstreken F. Incidence of scaphotrapezial arthritis following volar percutaneous fixation of nondisplaced scaphoid waist fractures using a transtrapezial approach. J Hand Surg 2011;36:1753-8. [Google Scholar] [PubMed]
- 26. Kaneko K, Miyazaki H, Yamaguchi T, Yanagihara Y, Kurosawa H. Bilateral transcapholunate dislocation. Chir Main 2000;19:263-8. [Google Scholar] [PubMed]
- 27. Ozkan K, Ugutmen E, Unay K, Poyanli O, Guven M, Eren A. Fractures of the bilateral distal radius and scaphoid: A case report. J Med Case Rep 2008;2:93. [Google Scholar] [PubMed]
- 28. Yildirim C, Unuvar F, Keklikci K, Demirtas M. Bilateral dorsal trans-scaphoid perilunate fracture-dislocation: A case report. Int J Surg Case Rep 2014;5:226-30. [Google Scholar] [PubMed]
- 29. Virani SR, Wajekar S, Mohan H, Dahapute AA. A unique case of bilateral trans-scaphoid perilunate dislocation with dislocation of lunate into the forearm. J Clin Orthop Trauma 2016;7:110-4. [Google Scholar] [PubMed]
- 30. Ghargozloo D, Tomarchio A, Ballerini M, Chitoni G. Traumatic bilateral scaphoid fractures. Med Glas 2021;18:222-5. [Google Scholar] [PubMed]
- 31. Meraghni N, Lahlali MA, Mohand-Oussaid A, Derradji M, Kara Z. Bilateral combined fractures of the scaphoid and distal radius: A case report. J Orthop Case Rep 2022;12:1-4. [Google Scholar] [PubMed]











