Prophylactic carpal tunnel release during volar plating for distal radius fractures significantly lowers the risk of postoperative median nerve compression. It leads to better functional outcomes without adding surgical risk, especially in high-risk fracture cases. This combined approach enhances recovery and reduces long-term complications.
Dr. Abhishek Sharma, Department of Orthopaedics, Krishna Vishwa Vidyapeeth, Karad, Maharashtra, India. E-mail: sharmaabhishek1912@gmail.com
Introduction: Carpal tunnel syndrome (CTS) is a recognized complication following distal end radius fractures, particularly when managed surgically using volar locking plates. The pathophysiology involves post-traumatic edema, hematoma formation, or surgical manipulation leading to median nerve compression. This study compares the incidence of CTS and functional outcomes between patients treated with volar plating alone and those undergoing simultaneous carpal tunnel release (CTR).
Materials and Methods: A prospective observational study was conducted on 34 patients with distal radius fractures, evenly divided into two groups: Group A underwent open reduction and internal fixation (ORIF) with prophylactic CTR, and Group B received ORIF alone. Patients were assessed clinically and electrophysiologically using electromyogram/nerve conduction velocity for CTS symptoms at 3 and 6 months postoperatively. Functional recovery was evaluated using the patient-rated wrist evaluation (PRWE) score. Post-operative complications were also recorded.
Results: At 3 months, CTS symptoms were present in five patients in Group A and seven patients in Group B. At 6 months, only two patients in Group A exhibited symptoms, whereas the number rose to 10 in Group B. Group A showed fewer complications, including nerve irritation (2 vs. 7), tendon irritation (3 vs. 5), infection (2 vs. 4), and plate loosening (1 vs. 2). PRWE scores were consistently better in Group A.
Conclusion: Prophylactic CTR at the time of volar plating for distal radius fractures appears to significantly reduce the incidence of post-operative CTS and improve functional outcomes without increasing complication rates. These findings support the role of early median nerve decompression in select cases.
Keywords: Distal radius fracture, carpal tunnel syndrome, volar plating, carpal tunnel release, electromyogram, patient-rated wrist evaluation.
Distal end radius fractures are among the most common orthopedic injuries, particularly in the elderly population due to osteoporosis and in younger individuals due to high-energy trauma. These fractures often require surgical management, especially in cases with comminution, intra-articular extension, or instability. Volar plating has become the standard approach for internal fixation, offering stable constructs and early mobilization.
Carpal tunnel syndrome (CTS) is a frequent complication following distal radius fractures, with an incidence ranging from 5% to 20% depending on fracture type and treatment modality [1]. Median nerve compression may occur due to fracture displacement, soft-tissue swelling, hematoma formation, or iatrogenic injury during surgery. In certain high-risk patients, this compression may evolve into chronic CTS if not addressed promptly [2].
Prophylactic carpal tunnel release (CTR) during volar plating has been proposed to minimize the risk of median nerve compression and facilitate early recovery. However, routine CTR remains controversial due to concerns about additional operative time and potential complications [3]. This study aims to compare outcomes between patients undergoing volar plating alone and those receiving simultaneous CTR, focusing on the incidence of CTS and functional recovery. Recent biomechanical studies suggest that volar plate positioning and increased intracompartmental pressure may contribute to transient median neuropathy postoperatively [4]. The acute inflammatory response and hematoma near the carpal tunnel exacerbate pressure on the median nerve. Moreover, individuals with narrow carpal tunnels or pre-existing subclinical neuropathy are particularly vulnerable [5]. Therefore, pre-emptive decompression may prevent progression to symptomatic CTS. Some authors advocate routine CTR in high-risk fractures, especially AO Type C patterns and in cases with significant dorsal comminution [6,7].
Aim of study
The aim of the study was to characterize nerve conduction changes resulting from open treatment of fracture of distal end of radius.
This prospective observational study was conducted between March 2023 to September 2024 at the Department of Orthopedics, Krishna Vishwa Vidyapeeth, Karad. Institutional ethical clearance was obtained before study initiation.
IEC NO: 370/2022-2023 (REF NO. KIMSDU/IEC/02/2023).
Inclusion criteria
- Age >18 years
- All types of distal end radius fractures (AO A3, B3, C2–C3)
- Radiographic/computed tomography scan confirmation of distal end radius fracture
- Treated definitively with volar plating fixation.
Exclusion criteria
- Other tunnel syndromes: Guyon’s canal, cubital tunnel, radial tunnel syndrome
- Pre-existing CTS symptoms
- Previous median nerve symptoms or prior CTR
- Hematological disorders: Hemophilia, thalassemia
- Corticosteroid use
- Age <18 years
- Non-adherence to follow-up protocol (6 months)
- Thyroid disorders
- Old fractures (>3 weeks)
- Open fractures
- Systemic diseases affecting nerve function or healing (e.g., diabetes mellitus, rheumatoid arthritis)
- Treatment strategies excluding volar plating.
Patients were divided into two groups of 17 each:
- Group A: Volar plating + prophylactic CTR
- Group B: Volar plating alone.
Surgical procedure
All patients were operated under regional or general anesthesia in the supine position with the affected limb placed on a radiolucent hand table. A pneumatic tourniquet was applied to the upper arm to maintain a bloodless field.
We used the standard volar approach through the flexor carpi radialis (FCR) interval. A longitudinal incision was made along the FCR tendon. After identifying and retracting the FCR and radial artery laterally and the flexor pollicis longus medially, we exposed the pronator quadratus muscle. The pronator was incised in an L-shaped manner and elevated subperiosteally to expose the distal radius.
Fracture reduction was achieved under direct vision with manual manipulation and aided by K-wires or small reduction forceps as required. Intraoperative fluoroscopy was used to confirm restoration of the volar tilt, radial height, and radial inclination.
An anatomically contoured volar locking/non-locking compression plate was then applied proximal to the watershed line. The distal screws were inserted first to achieve subchondral fixation, followed by proximal cortical screws. Final reduction and implant placement were confirmed under fluoroscopy in both anteroposterior and lateral views.
In patients allocated to the prophylactic CTR group, a separate longitudinal incision was made over the carpal tunnel. The transverse carpal ligament was carefully incised to decompress the median nerve.
After confirming hemostasis, the pronator quadratus was re-approximated wherever feasible. The wound was closed in layers, and a sterile dressing was applied. A below-elbow slab was given in a functional position for pain control, and patients were encouraged to begin finger movements on the same day.
Clinical examination for CTS symptoms (numbness, tingling, night pain) was performed at 3 and 6 months. Electromyogram/nerve conduction velocity (EMG/NCV) studies were used to confirm clinical diagnosis. Functional assessment was done using the PRWE score as mentioned in Fig. 1.
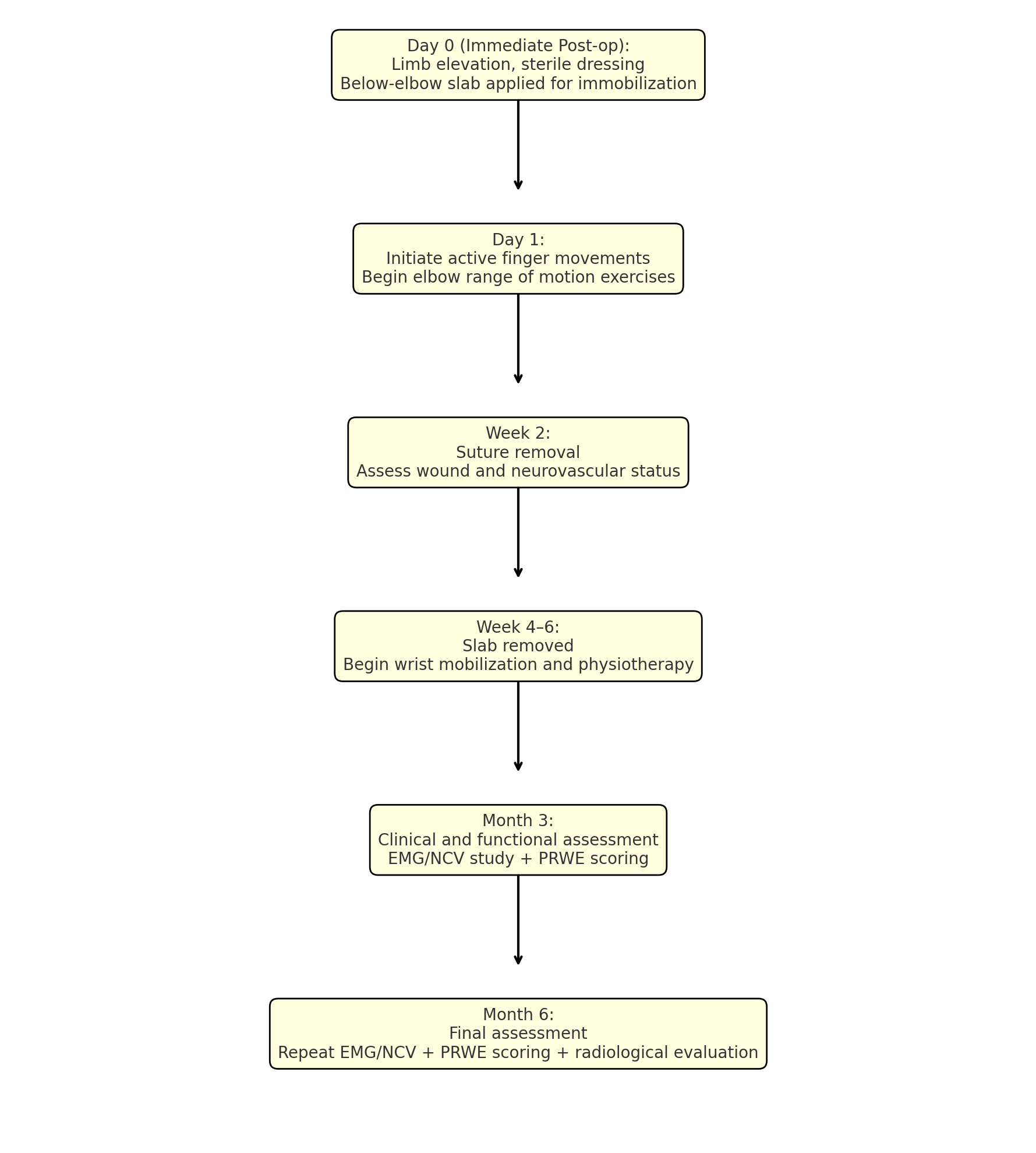
Figure 1: Post-operative protocol.
At the 3-month follow-up, 5 patients (29.4%) in Group A exhibited clinical and electrophysiological features of CTS, compared to 7 patients (41.1%) in Group B. By the 6-month mark, symptoms had resolved in most patients in Group A, with only 2 cases (11.7%) persisting, whereas Group B showed a significant increase to 10 symptomatic patients (58.8%). This progression highlights the protective benefit of prophylactic CTR as shown in Table 1.
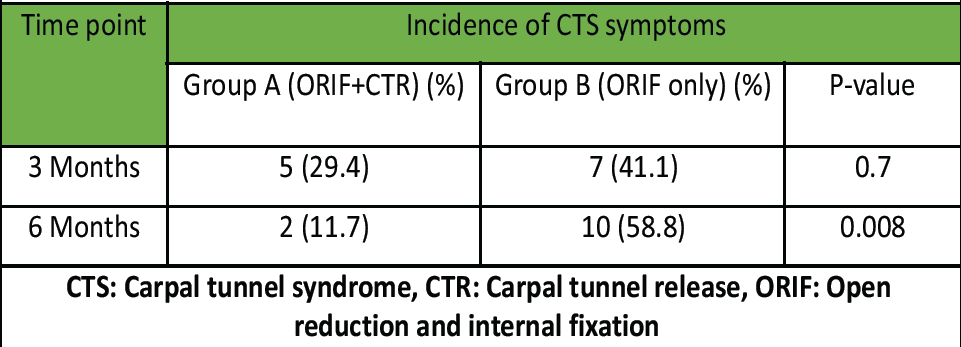
Table 1: Incidence of CTS symptoms at 3 and 6 months
In terms of complications, Group A had a lower incidence of nerve irritation 2 (11.7%) versus 9 (52.9%), tendon irritation 3 (17.6%) versus 7 (41.2%), superficial wound infections 2 (11.7%) versus 5 (29.4%), and plate loosening 1 (5.9%) versus 2 (11.7%) compared to Group B. These findings indicate that concurrent CTR did not result in additional surgical complications and may have reduced soft-tissue-related sequelae as shown in Table 2.
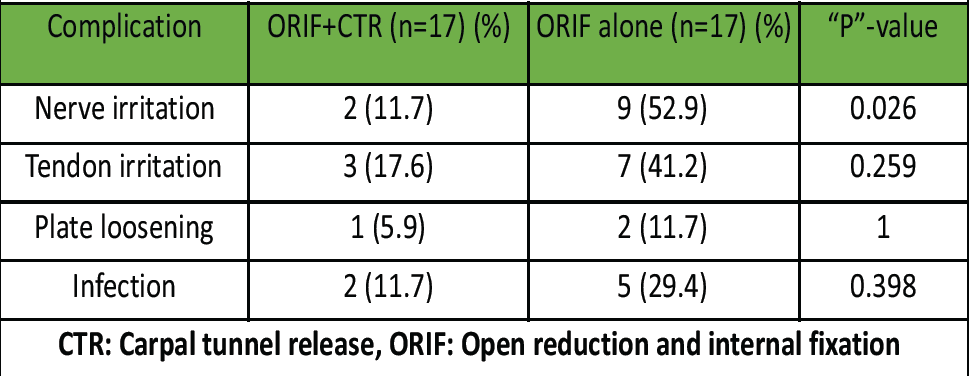
Table 2: Post-operative complications by treatment group
Functional outcomes, as measured by patient-rated wrist evaluation (PRWE) scores, showed a consistent advantage in Group A (38.2 ± 5.1 vs. 42.1 ± 6.3 at 3 months and 21.3 ± 4.7 vs. 26.8 ± 5.9 at 6 month), with improved pain relief and restoration of wrist function at both 3 and 6 months. The exact values are detailed in Table 3.
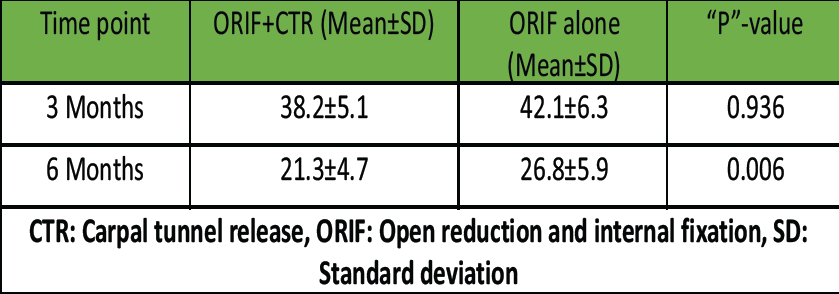
Table 3: Patient-rated wrist evaluation scores by treatment group
At 6 months postoperatively, the ORIF + CTR group demonstrated significantly fewer EMG/NCV abnormalities (23.5%) compared to the ORIF-alone group (64.7%), with the difference reaching statistical significance (P = 0.036), indicating a clear neuroprotective advantage of prophylactic CTR as shown in Table 4.
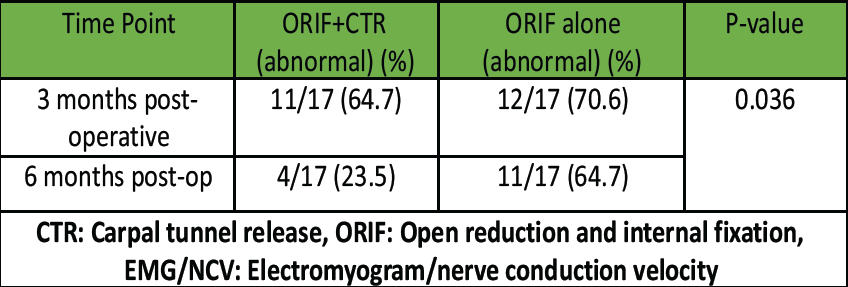
Table 4: Post-operative nerve conduction (EMG/NCV) abnormalities by treatment group
This study demonstrates a clear benefit of prophylactic CTR in reducing post-operative CTS incidence. Group A had significantly fewer cases of CTS at both follow-up points. This aligns with prior research by Meena et al., who reported improved nerve outcomes with early decompression in high-risk fractures [4]. Similarly, a study by Zhao et al., highlighted better PRWE scores in patients undergoing simultaneous CTR [5]. The pathophysiology of CTS in distal radius fractures involves median nerve ischemia from elevated compartment pressures or prolonged edema. Volar plating can exacerbate this due to surgical manipulation. Therefore, CTR may provide a protective effect, particularly in patients with high-energy trauma or severe comminution [6,8]. Other studies have shown that delayed recognition and treatment of post-traumatic CTS can lead to irreversible nerve damage and persistent functional impairment [9]. Our results, demonstrating a significantly lower rate of persistent CTS in the CTR group, reinforce the value of early intervention. Furthermore, post-operative complications were not increased in the CTR group, suggesting safety and feasibility. From a clinical standpoint, performing CTR concurrently with ORIF adds minimal operative time but may significantly reduce patient morbidity, especially in high-risk populations [10,11]. The findings also emphasize the importance of EMG/NCV testing for early detection, particularly in borderline symptomatic patients. Limitations include small sample size, single-center data, and lack of randomization. Future multicenter randomized trials are needed to validate our findings.
Cost-benefit impact of prophylactic CTS release:
- Cost side
Additional costs of prophylactic CTR
- Operative time: +10–15 min (increases OT costs slightly)
- Surgical fee/anesthesia: Marginally higher
- Consumables: Minimal (blade, retractors, sutures already in use)
- Hospital stay: Usually unchanged (done in same sitting as plating).
In most setups, prophylactic CTR adds ~5–10% to the surgery cost.
- Benefit side
Clinical benefits
- Prevents acute CTS from postoperative swelling or hematoma
- Avoids delayed CTS due to altered carpal tunnel dynamics after fracture fixation
- Immediate decompression → prevents median nerve ischemia and irreversible damage.
Economic benefits
- Avoids cost of secondary surgery (late CTR)
- OT charges
- Additional anesthesia
- Separate hospital stay
- Recovery downtime/work absence
- Prevents loss of productivity from prolonged neuropathy
- Reduces medico-legal risk if CTS develops post-fixation.
Prophylactic CTR at the time of volar plating in distal radius fractures significantly reduces the incidence of post-operative CTS and leads to superior functional outcomes. Our findings suggest that early decompression of the median nerve provides both preventive and therapeutic advantages, particularly in high-risk patients such as those with comminuted fractures or substantial soft-tissue swelling. The procedure does not increase operative risk and may even reduce the occurrence of nerve and tendon irritation. Incorporating CTR into the primary surgical plan may optimize patient satisfaction and decrease the likelihood of secondary interventions for CTS. Further large-scale randomized studies are needed to establish definitive guidelines for its routine use.
- Simultaneous carpal tunnel release at the time of fracture fixation offers a safe and effective strategy to prevent delayed-onset CTS
- It improves patient satisfaction, reduces post-operative nerve symptoms, and should be considered in distal radius fractures with high-risk features
References
- 1. Gelberman RH, Rydevik BL, Pess GM, Szabo RM, Lundborg G. The carpal tunnel syndrome: A scientific basis for clinical care. Orthop Clin North Am 1996;27:239-47. [Google Scholar]
- 2. Karl JW, Olson PR, Rosenwasser MP. Complications of distal radius fractures. J Am Acad Orthop Surg 2015;23:369-79. [Google Scholar]
- 3. Kim JK, Koh YD, Do NH. Median nerve injury during volar plating. J Hand Surg Am 2010;35:379-81. [Google Scholar]
- 4. Meena S, Sharma P, Sambharia AK, Dawar A. Prophylactic carpal tunnel release in distal radius fracture fixation: A prospective study. Indian J Orthop 2018;52:305-10. [Google Scholar]
- 5. Zhao H, Zhang F, Wang B, Ma J, Yang Y. Carpal tunnel release combined with volar plate fixation: A comparative study. J Orthop Surg Res 2020;15:211. [Google Scholar]
- 6. Oyen J, Brudvik C, Gjertsen JE. Carpal tunnel syndrome after distal radius fracture: A prospective study. J Orthop Trauma 2021;35:e135-40. [Google Scholar]
- 7. Gabl M, Reinhart C, Lutz M, Bodner G, Rudisch A, Hussl H. Acute carpal tunnel syndrome after distal radius fracture. J Trauma 2002;52:371-5. [Google Scholar]
- 8. Soni A, Gul A, Singh D, Gaba S, Singh P. High-risk distal radius fractures and carpal tunnel decompression. Acta Orthop Belg 2013;79:416-21. [Google Scholar]
- 9. Lutz K, Meuli-Simmen C, Jüni P, Jupiter JB. Long-term outcomes after surgical treatment of post-traumatic CTS. J Hand Surg Eur Vol 2012;37:783-9. [Google Scholar]
- 10. Takemoto R, Chung KC, Shauver MJ. Risk factors for carpal tunnel syndrome following distal radius fracture. J Hand Surg Am 2015;40:904-8. [Google Scholar]
- 11. Prommersberger KJ, van Schoonhoven J, Lanz UB. Simultaneous CTR and plate fixation. Arch Orthop Trauma Surg 2014;134:353-8. [Google Scholar]