Locking compression plate fixation of tibial plateau fractures facilitates early mobilization and yields favorable radiological and functional outcomes when precise reduction and stable fixation are achieved, particularly in high-energy fracture patterns.
Dr. Udit Agrawal, Department of Paediatric Orthopaedics, King George Medical University, Lucknow, Uttar Pradesh, India. E-mail: uditagrawal28@gmail.com
Introduction: Tibial plateau fractures are complex intra-articular injuries of the proximal tibia that can lead to significant functional impairment if not adequately managed. Locking compression plates (LCP) have emerged as a preferred modality for surgical fixation due to their biomechanical advantages, particularly in comminuted and osteoporotic fractures.
Materials and Methods: This prospective study included 35 adult patients with tibial plateau fractures treated with internal fixation using LCPs. Fractures were classified using the Schatzker classification, and patients were followed clinically and radiologically for a minimum of 6 months. Functional outcomes were assessed using the modified Rasmussen criteria (MRC), and radiological healing was evaluated using the Rasmussen radiological criteria (RRC).
Results: Most fractures occurred in middle-aged males, with road traffic accidents being the predominant mechanism of injury. Schatzker type II fractures were the most common pattern observed. At final follow-up, 51.43% of patients achieved excellent functional outcomes, and 45.71% demonstrated excellent radiological outcomes. The mean time to union was 14.38 weeks. The most frequent complications were knee stiffness and infection, primarily associated with high-energy fracture patterns.
Conclusion: LCP fixation of tibial plateau fractures provides reliable radiological union and satisfactory functional outcomes in most cases. Early mobilization and careful management of high-energy injuries are essential to optimize results.
Keywords: Tibial plateau fracture, locking compression plate, functional outcome, radiological outcome, Schatzker classification.
Tibial plateau fractures are intra-articular injuries involving the proximal tibia, an anatomical region critical for load transmission through the knee joint [1]. Disruption of this weight-bearing surface can lead to significant impairment of knee stability and long-term function if not appropriately addressed [2]. These fractures are frequently encountered in orthopedic practice and present considerable challenges in diagnosis, classification, and management. The fracture patterns of the tibial plateau are diverse, ranging from isolated lateral condylar depressions to complex bicondylar split and depression configurations [3]. Each pattern carries distinct biomechanical implications and requires a tailored therapeutic approach [4]. High-energy mechanisms of injury, such as road traffic accidents or falls from height, often result in extensive soft tissue damage and may be associated with ligamentous disruptions and meniscal injuries [1]. Accurate preoperative assessment, incorporating radiographs and advanced imaging like computed tomography (CT) or magnetic resonance imaging (MRI), is essential for defining fracture morphology and planning surgical intervention [5]. Management options for tibial plateau fractures include non-operative treatment in select low-energy, minimally displaced cases, as well as surgical fixation in displaced or unstable fractures [4]. Among surgical techniques, open reduction and internal fixation using locking compression plates (LCP) has become the preferred method due to its ability to achieve stable fixation, maintain reduction, and facilitate early mobilization [6]. Locking plates provide angular stability, particularly beneficial in osteoporotic bone and comminuted fractures [7]. Despite advancements in implant design and surgical technique, outcomes can be variable, and complications such as malunion, infection, stiffness, and post-traumatic osteoarthritis remain concerns [8]. Therefore, evaluating both the functional and radiological outcomes following fixation with LCP is critical to improve patient care and inform clinical decision-making. This report presents our experience assessing the functional recovery and radiological healing of tibial plateau fractures treated surgically with LCP, highlighting practical considerations and challenges encountered in management.
This prospective study was conducted in the Department of Orthopaedics at K V G Medical College and Hospital in Sullia from August 2022 to January 2024, following ethical approval from the institutional ethics committee. A total of 35 patients who met the established inclusion and exclusion criteria were enrolled in this research. The participants were adults aged 18 years and older who sustained tibial plateau fractures and were managed with internal fixation employing an LCP. Enrolment was restricted to individuals who were medically fit for surgical intervention and who provided informed consent to participate in the study. The exclusion criteria included patients younger than 18 years, those with open fractures, fractures associated with vascular injury, pathological fractures, and individuals managed conservatively. Furthermore, patients who were medically unfit for surgical procedures or who declined operative treatment were excluded from participation. All fractures were classified according to the Schatzker classification system. Each patient underwent fracture fixation using an LCP after obtaining informed consent and completing a thorough pre-operative evaluation. This evaluation included radiographs and CT scans with 3D reconstructions of the injured knee to assess the size, location, and extension of the articular fragment. Temporary stabilization of the fracture was achieved with an above-knee splint, and the limb was elevated. Surgeries were performed after securing informed consent under spinal anesthesia on a standard radiolucent table. The operative limb was prepared and draped according to established protocols, and a tourniquet was inflated as necessary. The surgical approach was adapted based on the fracture pattern, with the objective of achieving anatomical reduction of the articular fragment. The typical sequence of fixation involved indirect reduction and temporary fixation of the articular fracture, followed by the alignment of the articular fragment to the diaphysis and fixation with the plate.
During the post-operative period, radiographs were obtained, and a removable knee brace accompanied by limb elevation was provided for the operated limb. Intravenous antibiotics were administered for 2 days, followed by oral antibiotics for 5 days. The first wound inspection was conducted on post-operative day (POD) 2, followed by a subsequent inspection on POD 5. Static quadriceps and ankle pump exercises were initiated from the first POD, and patients were permitted to begin intermittent knee mobilization once pain had subsided. Sutures were removed on POD 14. Partial weight-bearing was allowed from 6 to 8 weeks, depending on the fracture configuration as assessed through radiographic evaluation. Full weight-bearing was deferred until there was radiographic evidence of union, typically observed between 8 and 12-week post-surgery. Patients were followed up at intervals of 2 weeks, 6 weeks, 12 weeks, and 24 weeks. Fracture union was evaluated both radiologically and clinically, where union was defined by the presence of complete bone regeneration at the fracture site and the absence of pain during full weight-bearing on the injured limb. Delayed union was characterized by inadequate consolidation 6-month post-operation. All complications, including malunion, delayed union, non-union, knee stiffness, and nerve injury, were meticulously documented. Functional evaluation was conducted utilizing the Modified Rasmussen criteria (MRC) [9], and radiological outcomes were assessed according to the Rasmussen radiological criteria (RRC) [9]. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software, version 25.0 (SPSS Inc., Chicago, IL, USA). Categorical data were reported as frequencies and proportions, while continuous data were expressed as means and standard deviations. The paired t-test was employed to determine statistical significance, with a P < 0.05 considered to be statistically significant.
This study encompasses a total of 35 consecutive cases of proximal tibia fractures, wherein 82.85% (29 cases) were male and 17.15% (6 cases) were female. The findings indicate a significant predominance of male patients, resulting in a male-to-female ratio of 4.8:1. Patients were represented across all age groups; however, the majority (54.28%, or 19 cases) fell within the age range of 30–50 years. The mean age of the study cohort was 44.8 years, with a standard deviation of 13.5 years, suggesting a higher incidence of these fractures in the middle-aged population (Table 1).
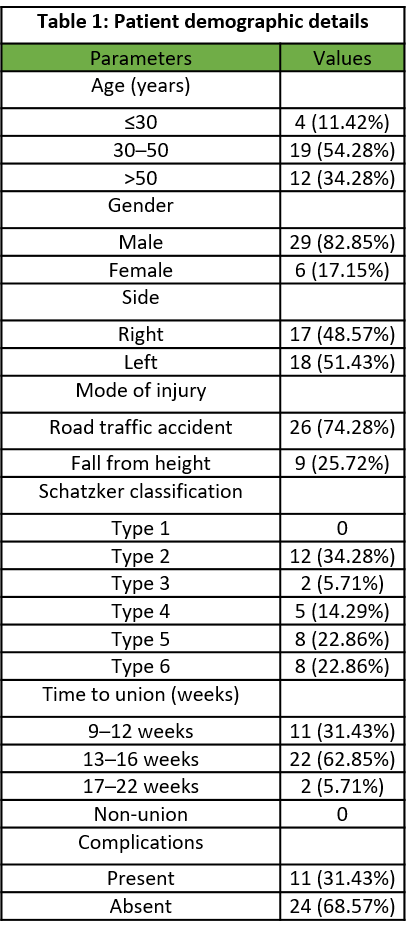
Table 1: Patient demographic details
In this study, 48.57% (17 cases) of patients sustained injuries to their right limb, while 51.43% (18 cases) experienced injuries to their left limb, indicating a minimal difference in site of injury. Furthermore, the majority of injuries (74.28%, or 26 cases) were attributed to road traffic accidents, suggesting that these injuries are more prevalent among males engaged in outdoor activities. Conversely, 25.72% (9 cases) of injuries resulted from simple domestic falls (Table 1).
Among the various fracture patterns, 34.28% (12 cases) presented with Schatzker type II fractures, which constituted the highest incidence. This was followed by types V and VI, each representing 22.86% (8 cases). Type III accounted for 5.71% (2 cases), and type IV comprised 14.29% (5 cases). Notably, no cases of type I fractures were observed (Table 1).
The mean range of motion at the final follow-up was recorded at 125° with a standard deviation of 9.90°. A significant improvement in range of motion was noted between the first and second follow-ups, followed by a gradual enhancement in subsequent assessments. All patients achieved a range of motion exceeding 90° during the final evaluation. Fractures categorized as Schatzker types II and III were treated with a single LCP (Fig. 1), while dual plating was required for nearly all cases of types V and VI (Fig. 2). In addition, three cases of type IV fractures were fixed with dual plating, and one type V fracture was stabilized utilizing triple plating.

Figure 1: (a and b) Pre-operative and 6-month follow-up radiograph of Schatzker type II proximal tibia fracture.

Figure 2: (a and b) Pre-operative and 6-month follow-up radiograph of Schatzker type VI proximal tibia fracture.
According to the MRC, 74.28% (26 cases) of patients initially demonstrated poor outcomes at the first follow-up. This statistic improved significantly, with 51.43% (18 cases) achieving excellent outcomes, 37.14% (13 cases) attaining good outcomes, and 8.57% (3 cases) categorized as fair outcomes, leaving only one case classified as poor. The improvement in outcomes was notably pronounced between the first and second follow-ups, characterized by a sharp increase, followed by steady enhancement up to the final visit, which was statistically significant (P < 0.001) (Tables 2 and 3).
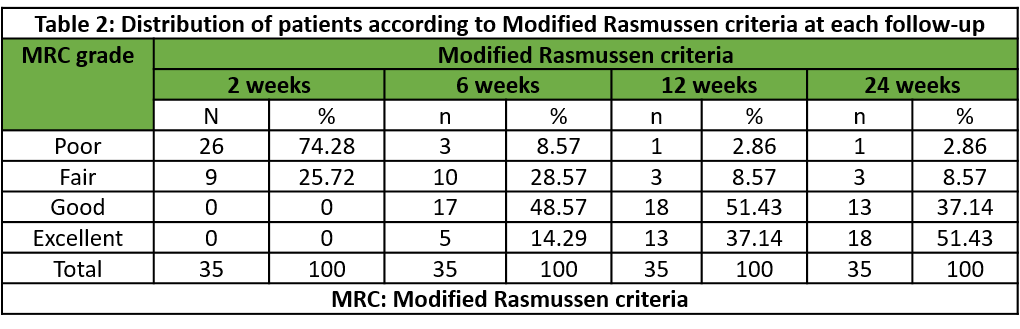
Table 2: Distribution of patients according to Modified Rasmussen criteria at each follow-up
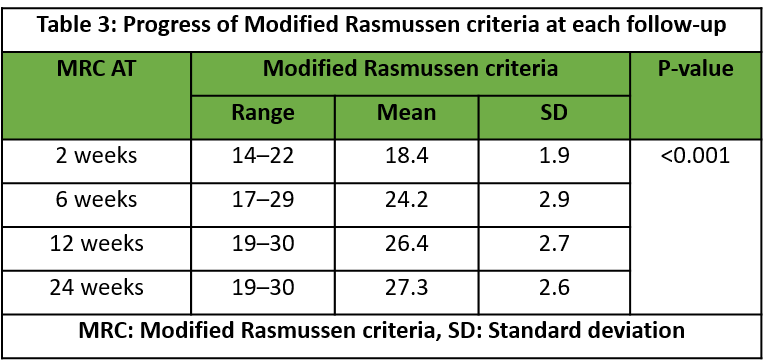
Table 3: Progress of Modified Rasmussen criteria at each follow-up
Radiological assessments were conducted utilizing the RRC. A progressive improvement in radiological outcomes was observed over time, with 45.71% (16 cases) achieving excellent results, 51.43% (18 cases) attaining good results, and 2.86% (1 case) classified as fair outcomes. These findings were statistically significant (P < 0.001) (Tables 4 and 5).
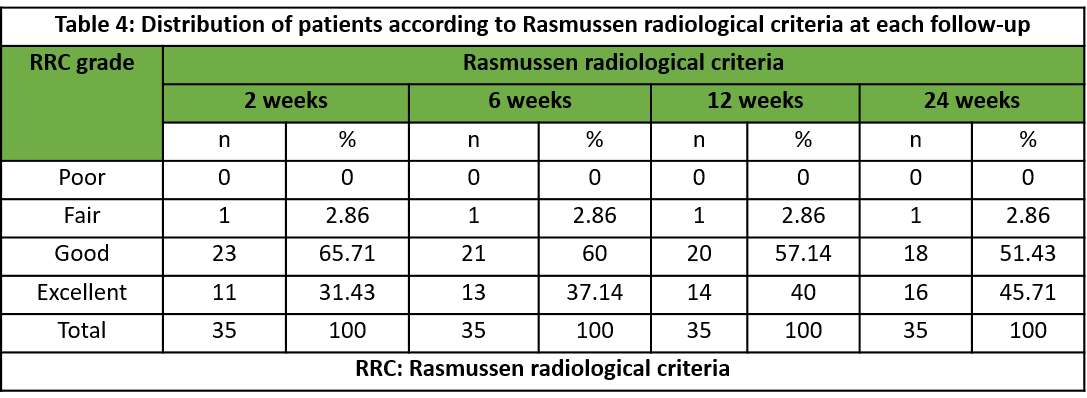
Table 4: Distribution of patients according to Rasmussen radiological criteria at each follow-up
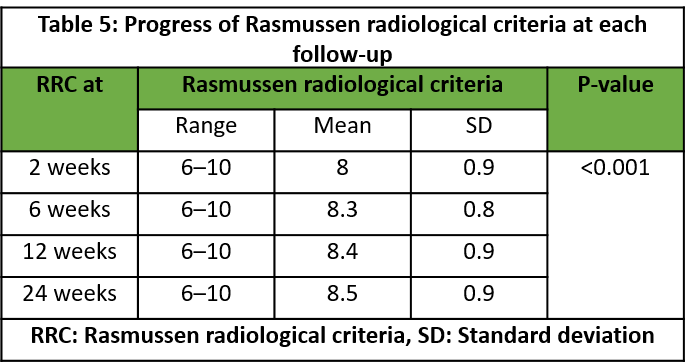
Table 5: Progress of Rasmussen radiological criteria at each follow-up
Tibial plateau fractures are common intra-articular injuries often caused by road traffic collisions, falls, or violence [1]. The management of these fractures raises debates about the need for surgery and the best treatment methods. Poor management can lead to complications like joint instability and restricted motion [2]. The introduction of locking plates has improved surgical techniques by reducing contact between the plate and bone while enhancing stability [1]. These plates feature modified screw holes that allow screws to lock, creating a fixed-angle system that minimizes vascular damage and is effective for osteoporotic bones [6]. This prospective study was conducted at a tertiary care hospital and involved 35 patients diagnosed with proximal tibial fractures, all of whom underwent internal fixation utilizing LCP. The cohort included individuals from various age demographics, with a majority, specifically 54.28% (19 patients), being between the ages of 30 and 50 years. The mean age was recorded at 44.8 years, with a standard deviation of 13.5 years, indicating a higher incidence of these fractures within the middle-aged population. This finding corroborates previous research by Bormann et al. [10] and Cole et al. [11]. In this patient cohort, 48.57% (17 patients) presented with injuries to the right limb, while 51.43% (18 patients) were affected on the left side, indicating no significant difference in limb distribution. A notable male predominance was observed, with 77.5% of the patients being male and 22.5% female. This observation is consistent with earlier studies by Tang et al., [12] and Sharma et al. [5], wherein 74.28% (26 patients) sustained their injuries as a result of road traffic accidents. This trend suggests that such injuries are more frequent among males engaged in outdoor activities. In addition, 25.72% (9 patients) experienced fractures due to simple domestic falls, reinforcing the notion that tibial plateau fractures are more likely to stem from high-velocity incidents, particularly in the middle-aged male demographic, as reported by Biggi et al. [13] and Sharma et al. [5]. In this study, the Schatzker classification was employed as the primary method for categorizing fracture types. A majority of 34.28% (12 patients) presented with a Schatzker type II fracture pattern, which exhibited the highest incidence, followed by type V and type VI fractures, each accounting for 22.86% (8 patients) of cases. This distribution aligns with the findings reported by Sharma et al. [5] and Gardner et al. [14]. All patients adhered to a non-weight-bearing regimen for 6 weeks postoperatively, after which they were gradually permitted to resume weight-bearing activities. The mean duration for achieving full weight-bearing status following surgery was 11.7 weeks, with a standard deviation of 1.9 weeks. Notably, nearly 60% of patients achieved full weight-bearing capability within the 9–12-week post-operative range, aligning with findings reported by Kalmet et al. [15].
Radiological and clinical union was observed within a timeframe of 9–22 weeks, with an average of 14.38 weeks. These results are consistent with findings from Prasad et al. [8], Manidakis et al. [16], and Sharma et al. [5]. All patients initiated passive range of motion exercises on the 1st POD. At the final follow-up, the mean range of motion was recorded at 125°, with a standard deviation of 9.90. By the 1-year follow-up, all patients demonstrated knee flexion exceeding 90°, consistent with observations made by Prasad et al. [8] and Sharma et al. [5]. In this study, 31.43% (11 patients) experienced some form of complications. The most frequently reported complication was knee stiffness, affecting 14.29% (5 patients). Infection occurred in 11.43% (4 patients), with one case classified as superficial and three as deep infections; these were addressed promptly with local wound care and antibiotics. In addition, knee instability was noted in 5.71% (2 cases). The majority of complications were associated with type V and VI fracture patterns, impacting 25.72% (9 patients), while other fracture types exhibited a relatively low incidence of complications. These findings are in accordance with studies conducted by Cole et al., Phisitkul et al. [17], Vasanad et al. [18], and Sharma et al. [5]. Notably, no patients in this series presented with complications such as compartment syndrome or deep venous thrombosis postoperatively. The MRC was the primary functional assessment metric in this study. Initially, 74.28% (26 patients) reported poor results, and 25.72% (9 patients) had fair results. At the 24-week follow-up, 51.43% (18 patients) achieved excellent results, 37.14% (13 patients) had good results, and only one patient experienced a poor outcome. The most significant improvements occurred between the first and second follow-ups, with a mean MRC score of 27.3 and a standard deviation of 2.6 at the final follow-up, consistent with findings from Jain et al. [19] and Sharma et al. [5]. Radiological assessments using the RRC showed that 45.71% (16 patients) achieved excellent results, 51.43% (18 patients) had good results, and 2.86% (1 patient) was recorded as fair, aligning with studies by Ebraheim et al. [20]. The main strengths of this study include its prospective design, standardized follow-up intervals, and the use of validated functional and radiological scoring systems to assess outcomes comprehensively across a representative spectrum of tibial plateau fracture types. However, the study is limited by its small sample size, single-center design, and short follow-up, which may affect generalizability and long-term outcome assessment. The lack of a control group, unblinded evaluations, and absence of patient-reported outcomes further limit the strength of the conclusions. Comorbidities and soft tissue injuries were not fully analyzed, and variability in surgical techniques was not accounted for.
LCP is an effective and dependable option for the surgical management of tibial plateau fractures, providing stable fixation that promotes early range of motion and satisfactory functional recovery. High-energy fractures and complex patterns require meticulous surgical technique and attentive post-operative care to minimize complications and optimize outcomes.
Anatomical reduction and stable fixation using locking compression plates in tibial plateau fractures enable predictable union and good functional recovery. Careful patient selection, early mobilization, and structured rehabilitation are a key to achieving optimal results, especially in high-energy fracture configurations.
References
- 1. Dunbar RP, Egol KA, Jones CB, Ostrum RF, Humphrey CA, Ricci WM, et al. Locked plating versus nailing for proximal tibia fractures: A multicenter RCT. J Orthop Trauma 2023;37:155-60. [Google Scholar] [PubMed]
- 2. García Vélez DA, Headford M, Suresh KV, Liberatos PM, Bledsoe G, Revak T. Biomechanical analysis of dual versus lateral locked plating in elderly bicondylar tibial plateau fractures: Does medial comminution matter? Injury 2022;53:3109-14. [Google Scholar] [PubMed]
- 3. Sharma S, Gupta P, Kothiyal P, Vij K. A prospective study on clinical, functional and radiological outcome of proximal tibia fractures treated with internal fixation by plating. Int J Orthop Sci 2023;9:319-23. [Google Scholar] [PubMed]
- 4. Mthethwa J, Chikate A. A review of the management of tibial plateau fractures. Musculoskelet Surg 2018;102:119-27. [Google Scholar] [PubMed]
- 5. Sharma SK, Yadav SS, Waghmare C, Jain P. Study of functional and radiological outcome of proximal tibial fractures managed with locking compression plating technique. Int J Pharm Clin Res 2023;15:661-70. [Google Scholar] [PubMed]
- 6. Amin TK, Patel I, Jangad AH, Shah H, Vyas RP, Patel NV, et al. Evaluation of radiological and functional outcome of intra-articular proximal tibia plateau fracture treated with plating. Malays Orthop J 2023;17:90-7. [Google Scholar] [PubMed]
- 7. Rohra N, Suri HS, Gangrade K. Functional and radiological outcome of schatzker type V and VI tibial plateau fracture treatment with dual plates with minimum 3 years follow-up: A prospective study. J Clin Diagn Res 2016;10:RC05-10. [Google Scholar] [PubMed]
- 8. Prasad GT, Kumar TS, Kumar RK, Murthy GK, Sundaram N. Functional outcome of Schatzker type V and VI tibial plateau fractures treated with dual plates. Indian J Orthop 2013;47:188-94. [Google Scholar] [PubMed]
- 9. Rasmussen S. Knee function-Rasmussen. J Orthop Trauma 2006;20:S88. [Google Scholar] [PubMed]
- 10. Bormann M, Neidlein C, Gassner C, Keppler AM, Bogner-Flatz V, Ehrnthaller C, et al. Changing patterns in the epidemiology of tibial plateau fractures: A 10-year review at a level-I trauma center. Eur J Trauma Emerg Surg 2023;49:401-9. [Google Scholar] [PubMed]
- 11. Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: Surgical experience and early clinical results in 77 fractures. J Orthop Trauma 2004;18:528-35. [Google Scholar] [PubMed]
- 12. Tang X, Liu L, Tu CQ, Yang TF, Wang GL, Fang Y, et al. Timing of internal fixation and effect on Schatzker IV-VI tibial plateau fractures. Chin J Traumatol 2012;15:81-5. [Google Scholar] [PubMed]
- 13. Biggi F, Di Fabio S, D’Antimo C, Trevisani S. Tibial plateau fractures: Internal fixation with locking plates and the MIPO technique. Injury 2010;41:1178-82. [Google Scholar] [PubMed]
- 14. Gardner MJ, Yacoubian S, Geller D, Suk M, Mintz D, Potter H, et al. The incidence of soft tissue injury in operative tibial plateau fractures: A magnetic resonance imaging analysis of 103 patients. J Orthop Trauma 2005;19:79-84. [Google Scholar] [PubMed]
- 15. Kalmet PH, Van Horn YY, Sanduleanu S, Seelen HA, Brink PR, Poeze M. Patient-reported quality of life and pain after permissive weight bearing in surgically treated trauma patients with tibial plateau fractures: A retrospective cohort study. Arch Orthop Trauma Surg 2019;139:483-8. [Google Scholar] [PubMed]
- 16. Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P. Tibial plateau fractures: Functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop 2010;34:565-70. [Google Scholar] [PubMed]
- 17. Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma 2007;21:83-91. [Google Scholar] [PubMed]
- 18. Vasanad GH, Antin SM, Akkimaradi RC, Policepatil P, Naikawadi G. Surgical management of tibial plateau fractures – a clinical study. J Clin Diagn Res 2013;7:3128-30. [Google Scholar] [PubMed]
- 19. Jain RK, Shukla R, Baxi M, Agrawal U, Yadav S. Evaluation of functional outcome of tibial plateau fractures managed by different surgical modalities. Int J Res Orthop 2016;2:5-12. [Google Scholar] [PubMed]
- 20. Ebraheim NA, Sabry FF, Haman SP. Open reduction and internal fixation of 117 tibial plateau fractures. Orthopedics 2004;27:1281-7. [Google Scholar] [PubMed]










