Autologous blood injection is a safe and effective alternative to corticosteroids for long-term pain relief and tendon healing in chronic lateral epicondylitis.
Dr. E-mail:
Objective: The objective of the study was to compare the efficacy of autologous blood (AB) injection versus local steroid injection in the treatment of lateral epicondylitis.
Materials and Methods: The current study was carried out at the department of orthopedics, Isra University Hospital, Hyderabad, Pakistan, from May 2024 to December 2024 after taking permission from the ethical board of the institute. A total of 400 patients aged 20–50 years with chronic lateral epicondylitis lasting more than 4 weeks and no prior treatment were enrolled. Using simple randomization, patients were assigned to Group A (methylprednisolone acetate 40 mg with 1 mL 2% lignocaine) or Group B (2 mL autologous venous blood from the opposite arm). Pain was assessed using the visual analogue scale (VAS) at 12 weeks. Data were analyzed with the Statistical Package for the Social Sciences version 24. Means and standard deviations were computed for quantitative variables, while Chi-square tests assessed pain relief.
Results: Two hundred patients were included in each group. Mean age was 37.04 ± 9.27 years in Group A and 38.33 ± 8.33 years in Group B. Baseline VAS scores showed no significant difference between groups. Post-treatment VAS scores were significantly lower in the AB group compared to the steroid group (P < 0.001). Pain relief stratified by age, sex, symptom duration, and baseline VAS score showed significant improvement in both groups, with greater improvement in Group B. No acute or late complications were observed.
Conclusion: AB injection provides superior and more sustained pain relief than steroid injection in patients with lateral epicondylitis.
Keywords: Comparison, efficacy, autologous blood injection, steroid injection, lateral epicondylitis.
Tennis elbow (lateral epicondylitis) is the second most common musculoskeletal condition in primary care that affects the neck and upper extremities. It is frequently diagnosed in orthopedic practice [1]. Its incidence in general practice ranges from 4 to 7 cases/1,000 annually with a mean age of almost 42 years and a peak within the ages of 35 and 54 [2,3,4,5]. According to an epidemiological study, the dominant arm was involved in 87% of cases [6]. Pain and tenderness over the lateral epicondyle are the hallmark clinical symptoms. Overuse from a number of activities has been associated with lateral epicondylitis. Despite being frequently called “tennis elbow,” it is more common in non-athletes than athletes [7,8]. The pathogenesis of acute lateral epicondylitis is controversial, and currently, there is not much research to support any specific course of therapy [9,10]. The majority of recent studies have suggested that lateral epicondylitis is caused by degeneration of the extensor carpi radialis brevis origin, repetitive microtrauma, and insufficient healing response (tendinosis) [11]. The majority of conservative techniques, such as local corticosteroid (CS) injections, focus on suppressing a hypothetical inflammatory process. The bleeding that occurs when fluid is forced into tissue planes at high pressure is thought to be the origin of the steroid injection’s positive effects [12]. Autologous blood (AB) injections have recently been shown to be beneficial for treating lateral epicondylitis in both the short and long term, with a notable reduction in discomfort [13]. The blood contains chemical cellular activity modifiers that are known to be mitomorphogenic. To trigger a healing cascade, AB injection (ABIs) may supply the cellular and humeral mediators required [14]. Orthopedic surgeons are increasingly using and favoring newer injectable treatments, including platelet-rich plasma (PRP) and ABIs. The effectiveness and safety of AB and PRP injections as therapeutic methods have been confirmed by many studies. Nonetheless, CS injections remain one of the most often used therapies. The high recurrence rate of steroid injections is a significant disadvantage. After an injection, individuals usually recover quickly, and this usually lasts for around a month [15]. ABIs as a therapy for lateral epicondylitis have been the subject of very few studies. Therefore, the current study was conducted to find out the efficacy of AB versus steroid in the treatment of lateral epicondylitis.
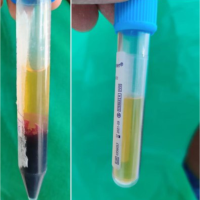
The current study was carried out at the Department of Orthopedics, Isra University Hospital, Hyderabad, Pakistan, from May 2024 to December 2024 after taking permission from the ethical board of the institute. A total of 400 individuals of both genders and different age groups (20–50) diagnosed with chronic cases of lateral epicondylitis with symptoms lasting more than 4 weeks and who had not received treatment were included in this study, while individuals with chronic diseases including diabetes, rheumatoid arthritis, and ankylosing spondylitis were excluded from the study. The study also excluded individuals who had previously had non-operative treatment or who had related elbow injuries. For this study, a 95% confidence level and an 80% power level were used to calculate the minimal sample size needed. With an expected effectiveness rate of 68% for local steroid injection and 79% for ABIs, the minimal sample size was determined to be 400 participants (200 in each group) using the method for comparing two proportions. Individuals who met the criteria were divided into two groups using a simple randomization technique after providing their informed consent. Participants in the single-blinded study were not told which therapy they received, but the researcher who gave the treatment was aware of the group assignments. Group A received methylprednisolone acetate injection of 40 mg locally, along with 1 mL of 2% lignocaine solution. Using a 21-gauge needle, Group B received a single injection of autologous venous blood (2 mL) from the opposite arm’s median cubital vein. To reduce the chance of clotting, the injection was administered immediately to the affected region. For the first 3 weeks after the injection, participants were instructed to avoid repeated wrist and elbow motion activities. They received verbal instructions on how to begin passive stretching exercises for the extensor muscle group as soon as their pain threshold allowed. The visual analogue scale (VAS) for pain evaluation was used to evaluate the final results at the end of 12 weeks. No late or acute side effects were noted after the medication during the research. Statistical Package for the Social Sciences version 24 was used to analyze the data. For quantitative factors like age and VAS score, descriptive statistics like the standard deviation and mean were computed. For qualitative characteristics like gender and pain alleviation, the percentages and frequency were calculated. While the Chi-square test was used to assess pain relief, the independent t-test was used to compare VAS scores between the two groups. To account for potential biases, data stratification was carried out based on variables such as age, gender, illness duration, and baseline VAS score. (Table 1).
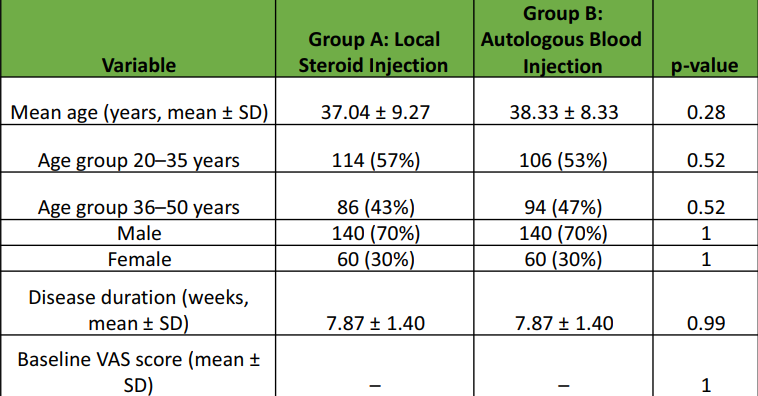
Table 1: Demographics Table
Overall, 400 individuals were included in this study with 200 in each group. The mean age of participants in Group B ABIs was 38.33 ± 8.33 years, whereas the mean age of individuals in Group A (local steroid injection) was 37.04 ± 9.27 years. In Group A, 114 of the participants (57%) were 20–35 years old, whereas Group B included 106 individuals (53%) in the same age range. In both groups, males were most prevalent (70% in each group). On average, the disease lasted 7.87 ± 1.40 weeks. There was no significant difference between the two groups’ baseline VAS scores (P = 1.000). Although arm dominance was not taken into account in this study, previous research indicates that the dominant side is more frequently affected by lateral epicondylitis [16]. AB had a substantially lower mean post-therapy VAS score than the local steroid injection group, with values of 3.48 ± 1.26 and 4.11 ± 1.62, respectively (P = 0.0001). Compared to Group A, Group B showed a greater rate of improvement in terms of pain reduction. In particular, only 120 (60%) of Group A reported pain reduction, compared to 158 (79%) of Group B (P = 0.0001). Significant differences were seen in both groups when the relief of pain results was stratified by age, sex, duration of injury, and baseline VAS score. Participants in Group B who were 36–50 years old reported greater rates of pain reduction than those who were 20–35 years old (86 vs. 71, P = 0.0001). In Group B, male participants also reported more pain alleviation than female participants (112 vs. 45, P = 0.0001). Furthermore, compared to people with shorter disease durations, individuals with disease durations longer than 6 weeks showed noticeably improved relief from pain results in both groups (Group A: 69 vs. 50, P = 0.0001; Group B: 81 vs. 76, P = 0.0001). Furthermore, Group B patients showed larger proportions of pain relief than Group A participants who had a baseline VAS score above 6 (94 vs. 74, P = 0.039). (Table 2).
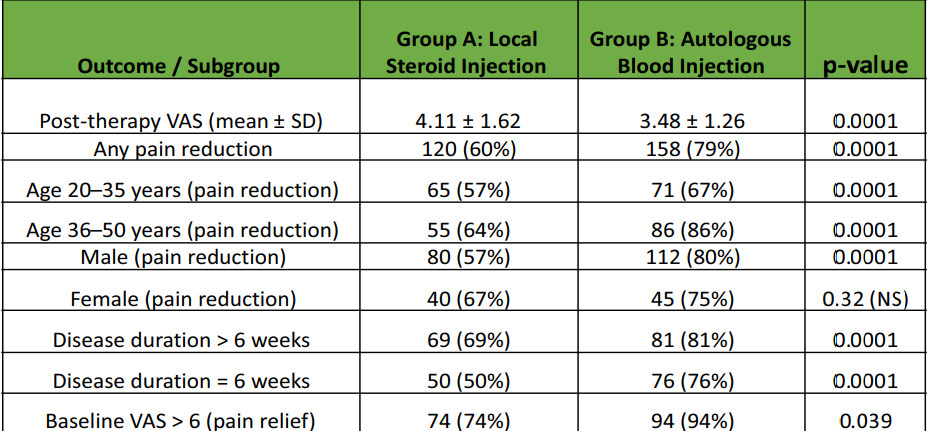
Table 2: Results Table
One of the most common muscular disorders, lateral epicondylitis (tennis elbow), affects the forearm’s common extensor origin. It usually arises from excessive strain on the wrist and finger extensors during repetitive manual labor, which severely limits a person’s capacity to do everyday tasks. The tenderness at the lateral epicondyle, both direct and indirect, is a clinical hallmark of the disease [17]. The most effective type of treatment for lateral epicondylitis is up for debate, despite the fact that the diagnosis is straightforward [18]. It has been shown that localized steroid injections consistently reduce pain in the short term. However, new therapies such as PRP injections, prolotherapy, ABIs, and extracorporeal shockwave therapy are being studied for their possible advantages [19]. The purpose of this study was to compare the efficacy of local steroid injections and ABIs in treating tennis elbow. Our findings revealed that there was no significant difference between the two groups’ baseline VAS scores (P = 1.000). However, the ABIs had a substantially lower mean post-therapy VAS score than the local steroid injection group (P = 0.0001). Compared to Group A, Group B showed a greater rate of improvement in terms of pain reduction (60% vs. 79%, P = 0.0001). These results are consistent with previous studies, including a study by Kazemi et al. that revealed ABIs to be more beneficial than CS treatment [19]. Injections of AB boost the inflammatory cascade by supplying humoral and cellular mediators, which aid in tendon recovery. Reductions in abnormal vascularity, anechoic foci, and interstitial cleft closure are examples of ultrasound evidence of tendon healing [13]. After receiving an ABIs, reports show recovery rates of 79% after a short period, 94.2% after 6 months, and 58% after 8 months [20]. The self-limiting character of the disease is highlighted by studies such as that conducted by Wolf et al., which reveals no significant difference among AB, CS, and placebo injections [16]. In a local investigation, local steroid injections and ABIs produced pain alleviation rates of 64% and 82%, respectively (P = 0.0005) [21]. By age and gender stratification, ABIs considerably decreased pain in all categories when compared to steroid injections [22]. Similarly, research by Mobarakeh et al. and Edwards and Calandruccio showed that ABIs resulted in excellent recovery rates, with success rates of 85% and 79%, respectively [10]. Connell et al. found that ABIs administered under ultrasound supervision had a 94.2% success rate in reducing pain [18]. On the other hand, certain studies, including the 6-week follow-up study by Singh et al., revealed no obvious distinction between the two approaches, indicating the need for more research [23]. Systematic experiments by de Vos et al. also showed that AB had no effect on tendinopathies [24]. Furthermore, Lee et al. revealed that in cases with plantar fasciitis, steroids provide comparable relief from pain [25]. It is crucial to remember that, despite the fact that arm dominance was not taken into account in this study, previous research indicates that lateral epicondylitis usually affects the dominant side [16]. This may have an effect on treatment results, thus information on the dominant arm’s involvement should be included in future research to give a more thorough picture of how it affects the efficacy of various treatment approaches [26].
Limitations of the study
This study has several limitations. The follow-up period was short (12 weeks), preventing assessment of long-term efficacy, recurrence, or sustained tendon healing. Being a single-center study limits generalizability to other populations and healthcare settings. The single-blinded design could introduce bias, as the treating physician was aware of group allocation. Functional outcomes such as grip strength, validated scoring systems, and return to activity were not evaluated. Finally, potential confounding factors, including arm dominance, occupational demands, and lifestyle factors, were not considered, which may have influenced results.
The present study concluded that, as compared to steroid injections, AB considerably relieves pain in individuals with lateral epicondylitis. AB could provide a more long-lasting and efficient therapy, thereby lowering the need for follow-up procedures and enhancing overall patient outcomes.
ABIs are a safe, simple, and effective treatment for lateral epicondylitis, providing greater and longer-lasting pain relief than CS injection. It can be considered a preferred option, especially for patients seeking sustained improvement and reduced recurrence.
References
- 1. Haahr JP, Andersen JH. Physical and psychosocial risk factors for lateral epicondylitis: a population based case-referent study. Occup Environ Med. 2003 May;60(5):322-329. doi:10.1136/oem.60.5.322. [Google Scholar] [PubMed] [CrossRef]
- 2. Hamilton PG. The prevalence of humeral epicondylitis: A survey in general practice. J R Coll Gen Pract 1986;36:464-5. [Google Scholar] [PubMed]
- 3. Verhaar JA. Tennis Elbow [Thesis]. Maastricht: Maastricht University Press; 2019. [Google Scholar] [PubMed]
- 4. Gruchow HW, Pelletier D. An epidemiologic study of tennis elbow. Incidence, recurrence, and effectiveness of prevention strategies. Am J Sports Med 1979;7:234-8. [Google Scholar] [PubMed]
- 5. Nirschl RP. Tennis elbow. Prim Care 1997;4:367-82. [Google Scholar] [PubMed]
- 6. Bernhang AM. The many causes of tennis elbow. NY State J Med 197979:1363-6. [Google Scholar] [PubMed]
- 7. Teitz CC, Garrett WE Jr, Miniaci A, Lee MH, Mann RA. Tendon problems in athletic individuals. Instr Course Lect. 1997;46:569-582. [Google Scholar] [PubMed]
- 8. Terry CS, Beaty JH. Shoulder and elbow injuries. In: Terry CS, editor. Campbell’s Operative Orthopaedics. 11th ed. Vol. 3. Mosby: Elsevier; 2018. p. 2634-8. [Google Scholar] [PubMed]
- 9. Bowen RE, Dorey FJ, Shapiro MS. Efficacy of nonoperative treatment for lateral epicondylitis. Am J Orthop (Belle Mead NJ). 2001 Aug;30(8):642-646. [Google Scholar] [PubMed]
- 10. Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surg Am. 2003 Mar;28(2):272-278. doi:10.1053/jhsu.2003.50045. [Google Scholar] [PubMed] [CrossRef]
- 11. Leadbetter WB. Cell-matrix response in tendon injury. Clin Sports Med. 1992 Jul;11(3):533-578. [Google Scholar] [PubMed]
- 12. Balasubramaniam P, Prathap K. The effect of injection of hydrocortisone into rabbit calcaneal tendons. J Bone Joint Surg Br 1972;54:729-34. [Google Scholar] [PubMed]
- 13. Connell DA, Ali KE, Ahmad M, Lambert S, Corbett S, Curtis M. Ultrasound-guided autologous blood injection for tennis elbow. Skeletal Radiol. 2006 Jun;35(6):371-377. doi:10.1007/s00256-006-0081-9. [Google Scholar] [PubMed] [CrossRef]
- 14. Zouzias IC, Byram IR, Shillingford JN, Levine WN. A primer for physical examination of the elbow. Phys Sportsmed 2012;40:51-61. [Google Scholar] [PubMed]
- 15. Kıvrak A, Ulusoy I. Comparison of the clinical results of platelet-rich plasma, steroid and autologous blood injections in the treatment of chronic lateral epicondylitis. Healthcare (Basel) 2023;11:767. [Google Scholar] [PubMed]
- 16. Wolf JM, Ozer K, Scott F, Gordon MJ, Williams AE. Comparison of autologous blood, corticosteroid, and saline injection in the treatment of lateral epicondylitis: A prospective, randomized, controlled multicenter study. J Hand Surg Am 2011;36:1269-72. [Google Scholar] [PubMed]
- 17. Gopal Sagar DC. Effectiveness of autologous blood and steroid injection in tennis elbow based on visual analog score pain score and Nirschl stage. J Nepalgunj Med Coll 2020;18:15-7. [Google Scholar] [PubMed]
- 18. Mobarakeh MK, Nemati A, Fazli A, Fallahi A, Safari S. Autologous blood injection for treatment of tennis elbow. Trauma Mon 2013;17:393-5. [Google Scholar] [PubMed]
- 19. Kazemi M, Azma K, Tavana B, Moghaddam FR, Panahi A. Autologous blood versus corticosteroid local injection in the short-term treatment of lateral elbow tendinopathy: A randomized clinical trial of efficacy. Am J Phys Med Rehabil 2010;89:660-7. [Google Scholar] [PubMed]
- 20. ul Gani N, Butt MF, Dhar SA, Farooq M, Mir MR, Kangu KA, et al. Autologous blood injection in the treatment of refractory tennis elbow. The Internet Journal of Orthopedic Surgery. 2006/2007;5(1):1. [Google Scholar] [PubMed]
- 21. Ahmad Z, Iqbal MZ, Rauf A, Shafi MT, Ahmad Z. Comparison of autologous blood injections versus steroid injections in tennis elbow. JSZMC 2019;10:4. [Google Scholar] [PubMed]
- 22. Arik HO, Kose O, Guler F, Deniz G, Egerci OF, Ucar M. Injection of autologous blood versus corticosteroid for lateral epicondylitis: a randomised controlled study. J Orthop Surg (Hong Kong) 2018;22:333-7. [Google Scholar] [PubMed]
- 23. Singh P, Gawri V, Singh M, Choudhary N, Khichy H. Comparative study of local steroid injection versus autologous blood injection therapy for the management of lateral epicondylitis. J Evol Med Dent Sci 2015;4:3449-57. [Google Scholar] [PubMed]
- 24. De Vos RJ, Van Veldhoven PL, Moen MH, Weir A, Tol JL, Maffulli N. Autologous growth factor injections in chronic tendinopathy: A systematic review. Br Med Bull 2010;95:63-77. [Google Scholar] [PubMed]
- 25. Lee TG, Ahmad TS. Intralesional autologous blood injection compared to corticosteroid injection for treatment of chronic plantar fasciitis. A prospective, randomized, controlled trial. Foot Ankle Int 2007;28:984-90. [Google Scholar] [PubMed]
- 26. Prabhu JA, Soni M, Chouhan D. Comparison of autologous blood injection and local steroid injection in the treatment of lateral epicondylitis: A prospective randomized trial. J Clin Orthop Trauma 2019;10:1179-84. [Google Scholar] [PubMed]