For cases of hallux hyperdorsiflexion and stiffness resistant to conservative treatment, surgical intervention may also be worth considering.
Dr. Nobuyuki Fujita, Department of Orthopaedic Surgery, Fujita Health University, Aichi, Japan. E-mail: nfujita2007@gmail.com
Introduction: Hallux hyperdorsiflexion and stiffness are typically associated with hallux rigidus. Although the underlying cause remains unclear, this case appears to have arisen in a patient undergoing treatment for schizophrenia, highlighting the importance of individualized and carefully tailored treatment approaches to achieve optimal patient outcomes and maintain high-quality care.
Case Report: A 71-year-old Asian woman undergoing treatment for schizophrenia presented with severe hyperdorsiflexion and stiffness of the right hallux, causing intense pain, which was particularly noticeable during gait and daily activities. Initially, the patient underwent rehabilitation to restore normal active motion of the right extensor hallucis longus (EHL). However, despite continuous rehabilitation, the stiffness persisted. Consequently, the patient underwent surgery involving dissection, lengthening of the distal EHL, and partial transposition of the proximal EHL. Postoperatively, the patient regained active hallux movement and showed significantly improved gait.
Conclusion: Surgical treatment should be considered as an alternative option if symptoms persist for long in patients with hallux hyperdorsiflexion and stiffness. However, this approach is technically demanding and requires careful consideration of the strategy for successful recovery and optimal patient outcomes.
Keywords: Hallux hyperdorsiflexion and stiffness, extensor hallucis longus, metatarsophalangeal joint.
A persistently stiff toe, which often results from tendon adhesion due to joint inflammation [1], requires a customized treatment approach decided by each physician. Stretching the stiff toe joint to achieve proper alignment and flexibility is a widely accepted approach in the initial stages [2]. However, if conservative treatment is ineffective, a specialized surgical approach may be warranted. Although hallux hyperdorsiflexion and stiffness typically result from hallux rigidus [3], we present an unusual case of an Asian female patient without any known risk factors except for a history of schizophrenia. In this case, the surgical option was constrained due to localization in a peripheral area. We thus explored a rare surgical solution for the treatment of hallux hyperdorsiflexion and stiffness in this case. The patient underwent a surgical approach combining the lengthening of the distal portion of the extensor hallucis longus (EHL) and partial transposition of the proximal EHL. The patient’s hallux movement recovered and gait improved, and the patient expressed high satisfaction. Surgical treatment could be considered as an alternative option if the patient’s symptoms persist for a long period.
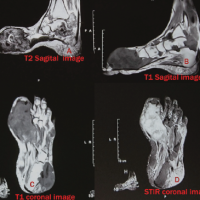
A 71-year-old Asian woman with a history of schizophrenia was admitted to our hospital for specialized care. During treatment, the patient developed severe hyperdorsiflexion and stiffness of the right hallux, causing intense pain, which was particularly noticeable during gait. As the condition persisted, the patient was referred to the orthopedic department for consultation. Physical examination and plain radiography revealed a hyperdorsiflexed contracture of the right hallux at 20° (Fig. 1).

Figure 1: Manifestation of hallux hyperdorsiflexion and stiffness on the dorsal aspect of the right toe, along with corresponding findings on plain radiography.
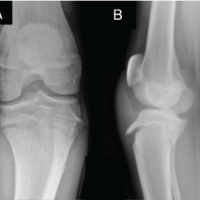
The condition was distinct from the so-called claw toe or hammer toe. Mild resistance to passive motion was observed; however, firm downward pressure temporarily achieved a plantar flexed position. There were no neurological abnormalities observed that are typically associated with schizophrenia or spinal cord disorders. The patient’s Japanese Society for Surgery of the Foot (JSSF) hallux metatarsophalangeal (MTP)-interphalangeal scale was 23. While radiographic findings were consistent with gross observations, the arrows of magnetic resonance imaging (MRI) (T1WI, T2WI) of the right MTP joint indicated areas of high signal intensity (Fig. 2).
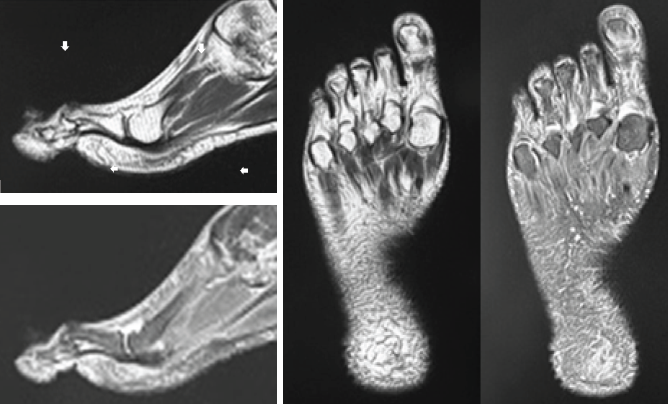
Figure 2: Magnetic resonance image of heightened signal intensity at the right metatarsophalangeal joint, indicative of localized tendinitis on the dorsal aspect of the right extensor hallucis longus. The MRI findings revealed that the area of signal intensity alteration was thin and localized along the tendon course at the level of the MTP joint, which ruled out the possibility of tumorous changes. Adhesion of the EHL tendon sheath to the surrounding tissues was considered the most likely cause of the stiffness, suggesting local tendinopathy. No other relevant observations were made. Based on the findings, the patient was clinically diagnosed with the right EHL tendinopathy, which associated with hyperdorsiflexion of the right hallux.
Initially, the patient was prescribed a 1month rehabilitation regimen to restore the normal active motion of the right EHL. However, despite continuous rehabilitation efforts, the stiffness persisted. The patient expressed a desire for the restoration of normal active motion of the right EHL and the amelioration of pain. Consequently, a surgical intervention was suggested, and the patient consented to the procedure. The procedure was performed under local infiltration anesthesia. After confirming that tumorous lesions were indeed unlikely, extensive release of the adhesive area surrounding the right MTP joint (Fig. 3a) and lengthening of the right EHL were planned (Fig. 3b).
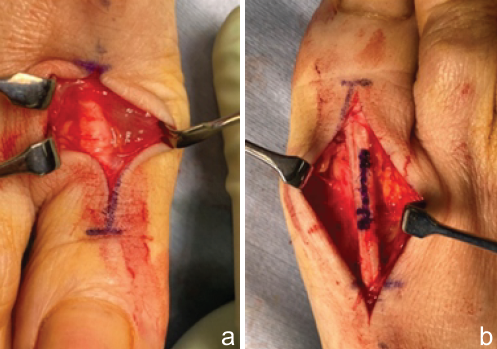
Figure 3: (a) Severe adhesive tendinitis is evident on the dorsal aspect of the right extensor hallucis longus, impeding active flexion of the hallux. (b) Initial plan for 10-mm lengthening of the right extensor hallucis longus, following the White slide technique.
The lengthening of the EHL was modeled after the White slide technique, which was originally devised for the lengthening of the Achilles tendon [4]. A lengthening of <20 mm of the EHL was anticipated to be sufficient; however, a neutral position could not be achieved without an edge-to-edge suture of the proximal and distal EHL (Fig. 4a), due to an unexpectedly high restoring force. At this stage, it became challenging to employ the White method which involves partially overlapping proximal and distal EHL.
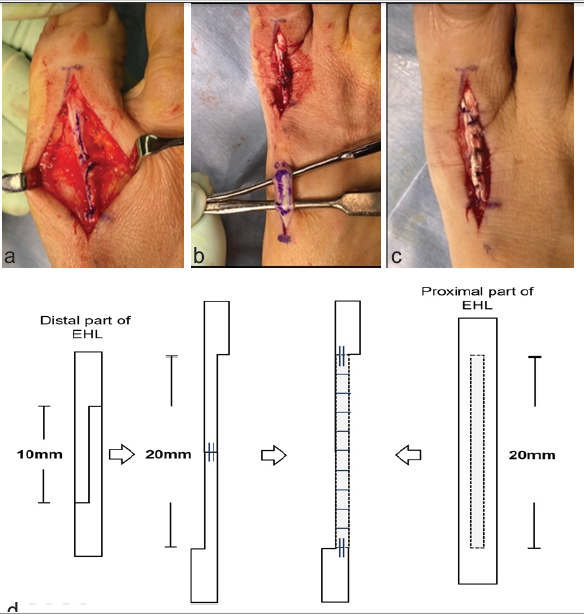
Figure 4: (a) The proximal and distal segments of the right extensor hallucis longus are subsequently connected using a precise edge-to-edge suture technique. (b) One-third thickness of the proximal portion of the right extensor hallucis longus is harvested to fortify the connective segment. (c) The transplanted graft reinforces the connected site. (d) The schematic diagram of the process.
Despite the edge-to-edge reinforcement using horizontal mattress sutures and simple interrupted sutures with monofilament suturing material, there were concerns regarding potential rupture due to the fragility of the delicate tissue. Consequently, a segment 1/3 in thickness and 20 mm in length was harvested from the proximal part of the right EHL (Fig. 4b) and grafted onto the connected part for reinforcement (Fig. 4c). The schematic diagram of the process is shown (Fig. 4d). The safety of early passive motion was ascertained through intraoperative assessment of gentle passive motion. Neutral alignment has been achieved through tendon lengthening and is expected to be maintained with external fixation. Furthermore, taking into account the preservation of tendon gliding function, the prevention of contracture risk, and the potential impact of pin site infection on the graft, it was deemed preferable not to perform bony stabilization using K-wires or similar methods. Postoperatively, a short splint was applied for 3 weeks. Following this period, the patient was instructed to commence range of motion (ROM) training and was advised to use the offloading shoe, OrthoWedge (DARCO, Huntington, WV) for an additional 3 weeks to avoid loading stress on the right toe. After 6 post-operative weeks, the patient was allowed to resume normal ambulation without OrthoWedge. The patient’s activities of daily living showed steady improvement. At the 1-year post-operative follow-up, the patient’s severe right hallux pain decreased from a visual analog scale score of 10–2, with temporary alleviation to 0. Moreover, the patient achieved a smooth right hallux ROM, progressing from a hyperdorsiflexed stiff hallux condition at 20° to a smooth hyperdorsiflexion of 25° and a smooth active plantar flexion of 5°, without recurrence of the previous condition. No recurrence of hyperdorsiflexion has been observed on follow-up plain radiograph (Fig. 5).
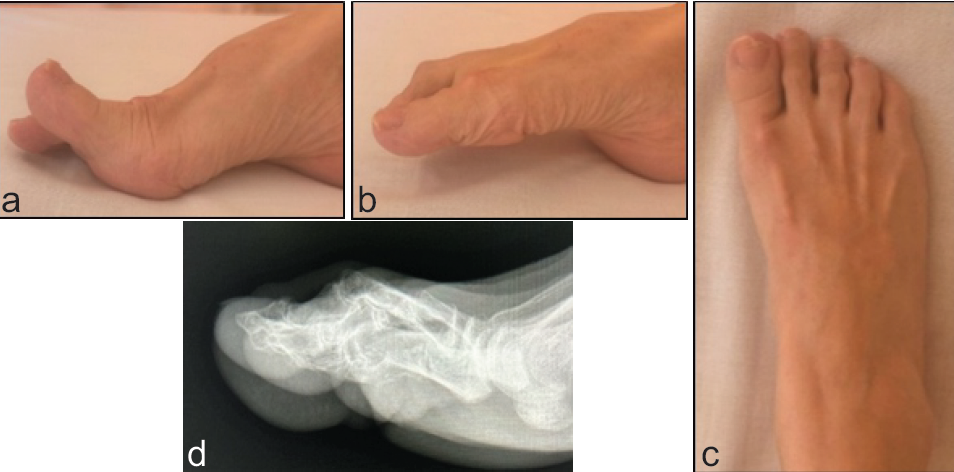
Figure 5: The appearance of the right metatarsophalangeal joint 1 year after the surgery. (a) Maximum active dorsiflexion is confirmed. (b) Maximum active plantar flexion is confirmed. (c) Overall appearance of the right foot. There is no recurrence of hallux hyperdorsiflexion and stiffness. (d) The hallux was observed to maintain a neutral alignment on plain radiograph.
Furthermore, the patient’s JSSF scale improved from 23 to 85, and there were significant improvements in gait. The patient was highly satisfied with the overall post-operative recovery and outcome.
The clinical management of common toe deformities, such as lesser toe deformity and hallux rigidus, has been extensively documented in numerous previous reports [5,6]. These conditions are often managed with treatment protocols that are widely recognized and implemented. However, when faced with an unusual case, such as the present case, a tailored approach to treatment is essential. The patient was undergoing treatment for schizophrenia; however, no reports were identified suggesting an association between schizophrenia or its treatment and toe tendonitis. Nevertheless, it cannot be conclusively stated that such an association does not exist. It is inferred that, based on the circumstances, neglecting the tenosynovitis that occurred near the MTP joint resulted in significant adhesions, ultimately leading to hyperextension. According to previous reports, persistent stiffness in the toe joints may negatively affect an individual’s gait [7,8]. This was evident in our patient who reported considerable difficulty in achieving a normal gait pattern due to stiffness. Consequently, there was a clear need for a targeted intervention to meet not only the patient’s desire for improvement but also the clinical necessity to restore function. Rehabilitation is typically the first treatment choice for toe joint stiffness [9,10]. While there are no reports that directly demonstrate rehabilitation as the primary treatment option for hallux hyperdorsiflexion in conditions caused by degenerative changes, following the examples of hallux rigidus, it is fundamental to first apply conservative therapy [6,10]. In accordance with this principle, the patient was prescribed a protocol of continuous rehabilitation exercises. Despite performing these exercises, the patient could achieve only limited relief from pain and no substantial improvement in the ROM of the joint. Due to the lack of progress, a surgical intervention was considered, and it ultimately led to a clinical recovery. Surgical solutions for individualized cases involve advantages and challenges. The primary benefit lies in the ability to confirm the restoration of passive ROM during the operation. However, surgery of the toe joints requires careful consideration of several factors. The distal portion of the tendon is delicate and prone to damage. Moreover, there is a significant likelihood that manipulation of the dorsal or plantar tendons might be required during surgery. In the present case, lengthening of the EHL was unavoidable to achieve proper alignment of the MTP joint, and all these procedures were technically demanding. Determining the appropriate tension of the joint intraoperatively is essential to ensure post-operative functionality. Although there are extensive studies on the surgical treatment of the extensor and flexor tendons in the hand, the number of studies on tendon treatment in the foot is limited [11]. It is estimated that reports on treatments for EHL rupture could serve as references for reinforcing the weakness associated with EHL lengthening. Kurashige reported the use of an autograft of the extensor hallucis capsularis (EHC), an accessory tendon of the EHL, in the treatment of chronic rupture of the main EHL [12]. The anatomical course of the EHC has been extensively studied, and it is known to be divided into several subtypes [13,14,15]. However, some individuals do not possess the EHC. Pre-operative planning to determine whether to use the EHC as reinforcement material is relatively difficult. In the present case, considering the limited site of the surgery on the distal part of the toe, it was preoperatively determined that reinforcement of the edge-to-edge EHL connection site could be achieved by partially harvesting the proximal part of the EHL on the same side, and intraoperatively, it was determined that this method would be effective. Eventually, the approach was successfully executed. Joseph and Barhorst has reported cases similar to the present case, where the EHL suture site was reinforced using an autograft from the same side of the EHL and further supported with augmentation [16]. Alternatively, Mowlavi et al. reported success in applying the robust Massachusetts General Hospital Repair technique for ruptures in the inherently thin EHL [11]. Kim et al., reconstructed a neglected EHL rupture by applying interposed scar tissue to tolerate the dorsiflexion force [17]. Among the various methods used to reinforce fragile parts, it is evident that physicians have been striving to measure the strength around the EHL connection site. In the post-operative phase, meticulous rehabilitation is essential to mitigate the risk of complications, particularly when tendon manipulation is involved. Early ROM exercise intervention may be effective in preventing the occurrence of contractures and can be beneficial [18]. However, excessive stress can cause rupture at the lengthened or connected site. Therefore, it is vital to effectively communicate intraoperative observations and critical information among the medical team to ensure safe and practical rehabilitation practices.
The present case study highlights the importance of a customized approach in treating rare conditions, such as hallux hyperdorsiflexion and stiffness. This report underscores the potential of surgical intervention as a viable alternative when conservative treatments are not successful. However, the advantages and challenges of surgical intervention should be taken into account to address the various irregular conditions of individuals.
Surgery was performed to address hyperdorsiflexion and stiffness of the hallux. In this case, favorable clinical outcomes were achieved by reinforcing the weak areas through partial transfer of the extensor hallucis longus (EHL). For individualized lesion management, especially in challenging surgeries, it is crucial to adopt treatments that not only comprehensively consider the patient’s background and the extent of the lesion’s impact on daily life but also carefully weigh the benefits of the surgery against the associated patient burden and potential concerns.
References
- 1. Chartier C, ElHawary H, Baradaran A, Vorstenbosch J, Xu L, Efanov JI. Tendon: Principles of healing and repair. Semin Plast Surg 2021;35:211-5. [Google Scholar] [PubMed]
- 2. Kage V, Basti A, Tashildar A, Jain A. Combined effect of myofascial release and passive stretching on plantar pressure in individual with hamstring tightness- an experimental study. J Bodyw Mov Ther 2024;37:412-6. [Google Scholar] [PubMed]
- 3. Brantingham, JW, Wood TG. Hallux rigidus. J Chiropr Med 2022;1:31-7. [Google Scholar] [PubMed]
- 4. Dietz FR, Albright JC, Dolan L. Medium-term follow-up of Achilles tendon lengthening in the treatment of ankle equinus in cerebral palsy. Iowa Orthop J 2006;26:27-32. [Google Scholar] [PubMed]
- 5. De Cesar Netto C, Schmidt EL, Lalevee M, Mansur NS. Flexor tenodesis procedure in the treatment of lesser toe deformities. Arch Orthop Trauma Surg 2022;142:3125-37. [Google Scholar] [PubMed]
- 6. Honert EC, Bastas G, Zelik KE. Effect of toe joint stiffness and toe shape on walking biomechanics. Bioinspir Biomim 2022; 213:066007. [Google Scholar] [PubMed]
- 7. Riddick RC, Farris DJ, Brown NA, Kelly LA. Stiffening the human foot with a biomimetic exotendon. Sci Rep 2021;11:22778. [Google Scholar] [PubMed]
- 8. Anderson MR, Ho BS, Baumhauer JF. Republication of “current concepts review: Hallux rigidus”. Foot Ankle Orthop 2023;8:1-11 [Google Scholar] [PubMed]
- 9. Lam A, Chan JJ, Surace MF, Vulcano E. Hallux rigidus: How do I approach it? World J Orthop 2017;8:364-71. [Google Scholar] [PubMed]
- 10. Mohaddis M, Maqsood SA, Ago E, Singh S, Naim Z, Prasad S. Enhancing functional rehabilitation through orthotic interventions for foot and ankle conditions: A narrative review. Cureus 2023;15:e49103. [Google Scholar] [PubMed]
- 11. Mowlavi A, Schall J, Wilhelmi BJ. Extensor hallucis longus tenorrhaphy by using the Massachusetts General Hospital repair. J Foot Ankle Surg 2004;43:412-8. [Google Scholar] [PubMed]
- 12. Kurashige T. Chronic extensor hallucis longus tendon rupture treated with double-bundle autograft of extensor hallucis capsularis: A case report. SAGE Open Med Case Rep 2019;7: 1-6 [Google Scholar] [PubMed]
- 13. Zielinska N, Tubbs RS, Ruzik K, Olewnik Ł. Classifications of the extensor hallucis longus tendon variations: Updated and comprehensive narrative review. Ann Anat 2021;238:151762. [Google Scholar] [PubMed]
- 14. Park JH, Choi YJ, Lee M, Kim D, Kwon HW, Park KR, et al. Anatomical characteristics of extensor hallucis longus tendon variations and its clinical implications: A Korean cadaveric study. Int J Environ Res Public Health 2022;19:9833. [Google Scholar] [PubMed]
- 15. Olewnik Ł, Podgórski M, Polguj M, Ruzik K, Topol M. A cadaveric study of the morphology of the extensor hallucis longus – a proposal for a new classification. BMC Musculoskelet Disord 2019;20:310. [Google Scholar] [PubMed]
- 16. Joseph RM, Barhorst J. Surgical reconstruction and mobilization therapy for a retracted extensor hallucis longus laceration and tendon defect repaired by split extensor hallucis longus tendon lengthening and dermal scaffold augmentation. J Foot Ankle Surg 2012;51:509-16. [Google Scholar] [PubMed]
- 17. Kim WJ, Jung KJ, Ahn H, Yeo ED, Lee HS, Won SH, et al. Reconstruction of a neglected, extensor hallucis longus tendon rupture using interposed scar tissue: A case report and literature review. Int J Environ Res Public Health 2021;18:12157. [Google Scholar] [PubMed]
- 18. Hege AR, Choubisa C, Chitale N, Phansopkar P. Physiotherapy management post-operative to total extensor hallucis longus rupture: A case report. Cureus 2023;15:e50434. [Google Scholar] [PubMed]