This study aims to assess the functional outcomes of anterior clavicle plating in individuals with midshaft clavicle fractures, specifically those classified as Allman Group 1 fractures. The Constant-Murley score will be used as the primary measure of outcome, focusing on improvements in pain, range of motion, shoulder strength, and the ability to perform activities of daily living (ADL) following surgery. By comparing pre-operative and post-operative Constant-Murley scores, the research will evaluate whether anterior clavicle plating results in significant improvements in shoulder function and recovery when compared to alternative treatment methods. The ultimate objective is to determine the effectiveness of this surgical technique in restoring normal shoulder function in patients with midshaft clavicle fractures.
Dr. K V Prem Kumar, Department of Orthopaedics and Traumatology, Chettinad Hospital and Research Institute, Chettinad Academy and Research Education, Chennai, Tamil Nadu, India. E-mail: drpremkumar.kvk@gmail.com
Introduction: Midshaft clavicle fractures are frequent injuries traditionally treated conservatively, but recent trends emphasize surgical intervention to achieve better functional outcomes. Anterior clavicle plating has become a viable alternative to the traditional superior plating technique for specific fracture types, offering potential benefits, such as reduced irritation from hardware and improved cosmetic appearance. However, further studies are needed to assess its biomechanical stability and overall functional effectiveness.
Objective: The objective of this study is to assess the functional outcomes of anterior clavicle plating in patients with midshaft clavicle fractures-Allman group – 1.
Materials and Methods: This was a prospective observational study conducted on patients who underwent anterior clavicle plating for midshaft clavicle fractures. Post-operative functional outcomes were measured using the Constant-Murley Score (CMS) at 1 month, 3 months, 6 months, and 12 months after surgery.
Results: Forty-two patients participated in the study, with 69% being male. Notable improvements in functional scores were observed at each follow-up point, with the mean CMS rising from 76.12 ± 3.71 at 1 month to 98.26 ± 2.72 at 12 months (P < 0.05). Only 4.8% of patients reported post-operative complications.
Conclusion: Anterior clavicle plating is a safe and effective surgical option for midshaft clavicle fractures, yielding excellent functional outcomes with a low complication rate. This technique is particularly advantageous in tertiary care centres, where comprehensive expertise and resources ensure optimal patient care.
Keywords: Clavicle fractures, fracture fixation, surgical outcomes, post-operative complications, anterior clavicle plating.
Fractures of the clavicle are one among the most common upper limb injuries, accounting for approximately 2.6–5% of all adult fractures and 35–44% of shoulder girdle injuries [1]. Midshaft clavicle fractures are the most prevalent type, constituting nearly 4/5th of all clavicular fractures [2]. These fractures have traditionally been treated with conservative management. However, recent studies suggest that surgical fixation, particularly for displaced fractures, may result in better functional outcomes. Displaced fractures have a higher risk of complications, such as non-union and malunion, making surgical intervention increasingly favoured.
The standard surgical method for treating midshaft clavicle fractures is open reduction and internal fixation (ORIF) with plate osteosynthesis [3]. Among the various plating methods, anterior clavicle plating has emerged as a promising alternative to the more commonly used superior clavicle plating, especially for certain fracture patterns. By positioning the plate on the clavicle’s anterior aspect, this procedure offers benefits, such as less hardware prominence, less irritation of soft tissues, and possibly better cosmetic results [4]. However, concerns regarding the biomechanical stability of anterior plating persist, and further investigation is required to evaluate its full clinical efficacy.
In anterior clavicle plating, the plate is aligned along the natural curve of the clavicle’s anterior surface. Recon plates are typically used as they can be contoured to fit the clavicle’s shape. This technique minimizes the risk of neurovascular injury and hardware irritation while providing adequate stability for fracture healing. In addition, the anterior placement of the plate can improve cosmetic results by reducing the visibility of the hardware [5].
The advantages of anterior clavicle plating include a lower incidence of soft tissue irritation and fewer hardware-related complications when compared to superior plating (Fig. 1).
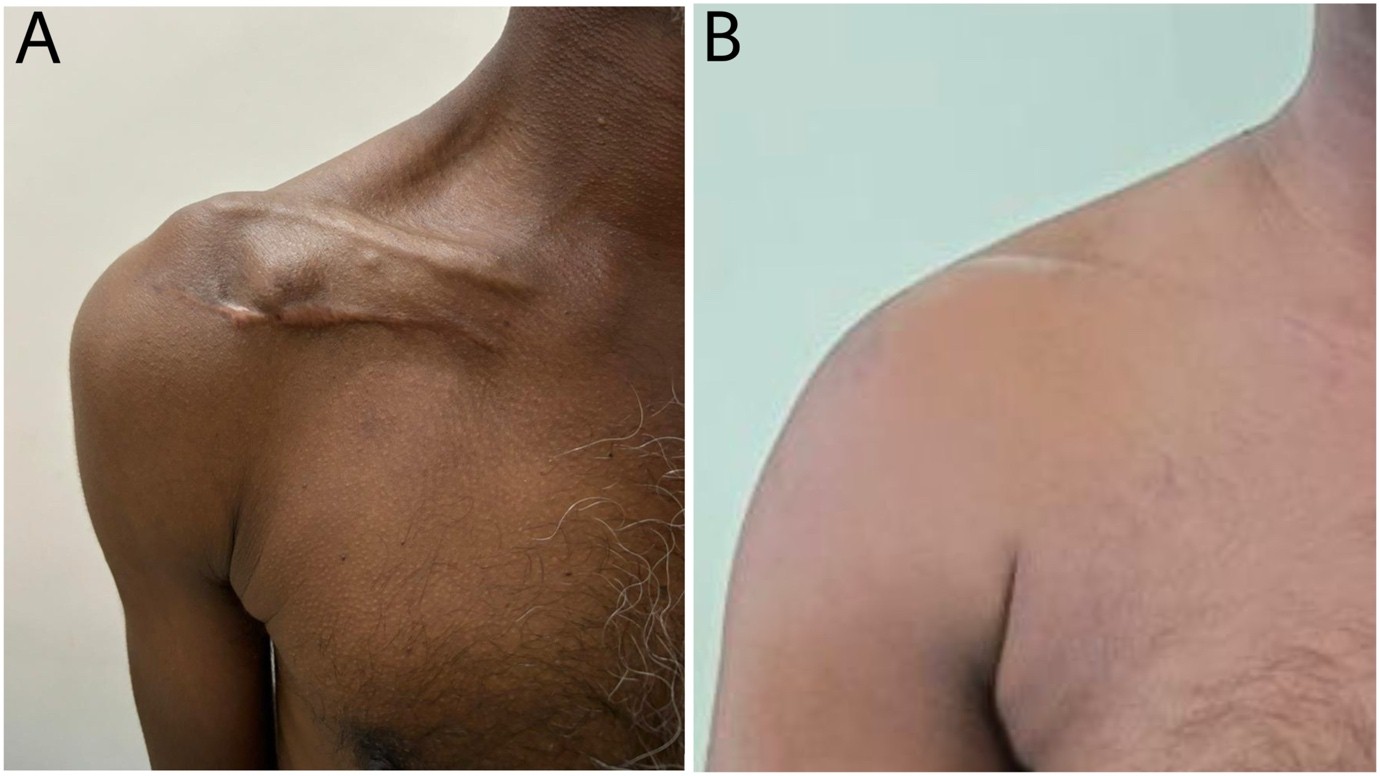
Figure 1: Clinical picture showing comparison of superior (a) and anterior (b) clavicle plating, with superior clavicle plating showing implant prominence.
This method may also improve patient comfort and compliance during the recovery process, supporting early mobilization and functional restoration [6]. Anterior plating has proven to be particularly effective in treating coronal split fractures and vertical fractures, as compared to superior plating. However, more study is required to fully assess the functional results of anterior clavicle plating, especially in tertiary medical facilities where patients with different fracture patterns and treatment requirements are treated.
This research work aims to assess the functional and radiological outcomes of anterior clavicle plating for midshaft clavicle fractures in a tertiary care setting, focusing on its effectiveness in promoting fracture healing and minimizing complications.
Objectives
- To evaluate the functional outcomes of anterior clavicle plating in patients with midshaft clavicle fractures
- To examine post-operative complications related to anterior clavicle plating, such as neurovascular damage, implant prominence, and infections at the surgical site
- To assess the radiological union of the fracture using the Zanca view.
The Department of Orthopedics in a tertiary care hospital and research institute carried out this prospective descriptive study for a duration of 1 year. Patients who presented with midshaft clavicle fractures to the Orthopedic Department were included. Patients were chosen based on pre-defined inclusion criteria and their willingness to provide informed consent. Inclusion criteria were patients aged 18 years or older with closed clavicle fractures, specifically fractures of the midshaft of the clavicle (Allman group 1), comminuted fractures, fractures with displacement >2 cm, and segmental fractures. Patients excluded from the study were those younger than 18 or older than 80 years, those with open clavicle fractures, polytrauma, acromioclavicular joint dislocation, a history of malignancy, local infection at the fracture site, or any associated fractures in the shoulder.
Data were collected using a semi-structured pro forma, which captured both sociodemographic and clinical information, as well as functional outcomes measured by the Constant-Murley Score (CMS). With a total score ranging from 0 to 100, the CMS evaluates the range of motion (40 points), strength (25 points), activities of daily life (20 points), and pain (15 points). All eligible patients underwent anterior clavicle plating and were evaluated post-operatively through clinical examinations, shoulder mobility assessments, radiological imaging, and the CMS at 1 month, 3 months, 6 months, and 1 year. Radiological assessment of fracture union was done using the Zanca view.
The Statistical Package for the Social Science version 21 and MS Excel were used for statistical analysis. Frequencies and percentages were used to express descriptive statistics. For longitudinal analysis, repeated measures-analysis of variance (RM-ANOVA) was employed, and paired t-tests were utilized to compare the post-operative CMSs. When the P < 0.05, it was seen as statistically significant. All costs related to investigations, surgery, and post-operative care were covered by the patients, although financial assistance was offered to those in need upon verification of their economic status.
Before participation, informed consent was obtained from all individuals, ensuring they were fully aware of the study’s purpose, methodology, potential risks, and measures taken to maintain data confidentiality. Participants were given the opportunity to ask questions and voluntarily agreed to take part in the research. Participants also consented to the use of their data and images for academic publications, with the assurance that their anonymity would be preserved.
The sociodemographic characteristics, fracture diagnosis, and AO clavicle grading of the study participants are summarized in Table 1.
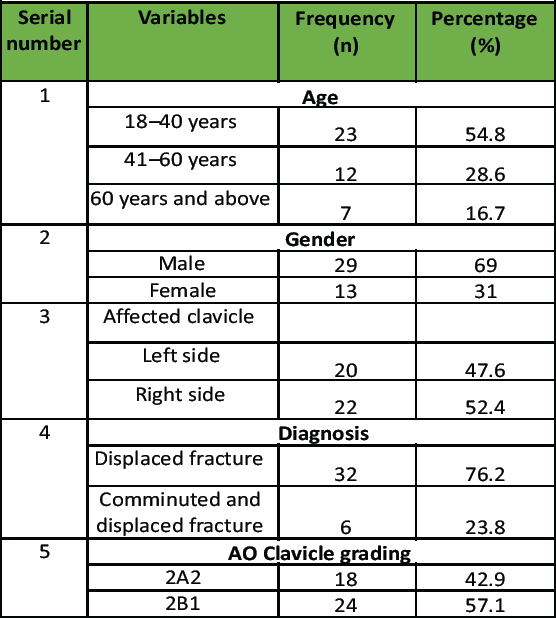
Table 1: Distribution of sociodemographic variables, diagnosis, and AO clavicle grading (n=42)
About 42 participants were recruited in this research work, with most (54.8%) falling within the 18–40-year age group, followed by 28.6% between 41 and 60 years, and 16.7% aged 60 years or older. Males comprised 69% of the study population, while females accounted for 31%. Fractures were slightly more common on the right clavicle (52.4%) than the left (47.6%). Most participants (76.2%) had displaced middle-third clavicle fractures, followed by comminuted displaced fractures (23.8%). The most frequently observed AO clavicle grading was 2B1, seen in 24 cases (57.1%). Fig. 2 shows the Intraoperative images with key surgical steps, including incision marking (Fig. 2a), fracture reduction (Fig. 2b), plate fixation (Fig. 2c), and confirmation of implant positioning using intraoperative C-arm imaging (Fig. 2d).
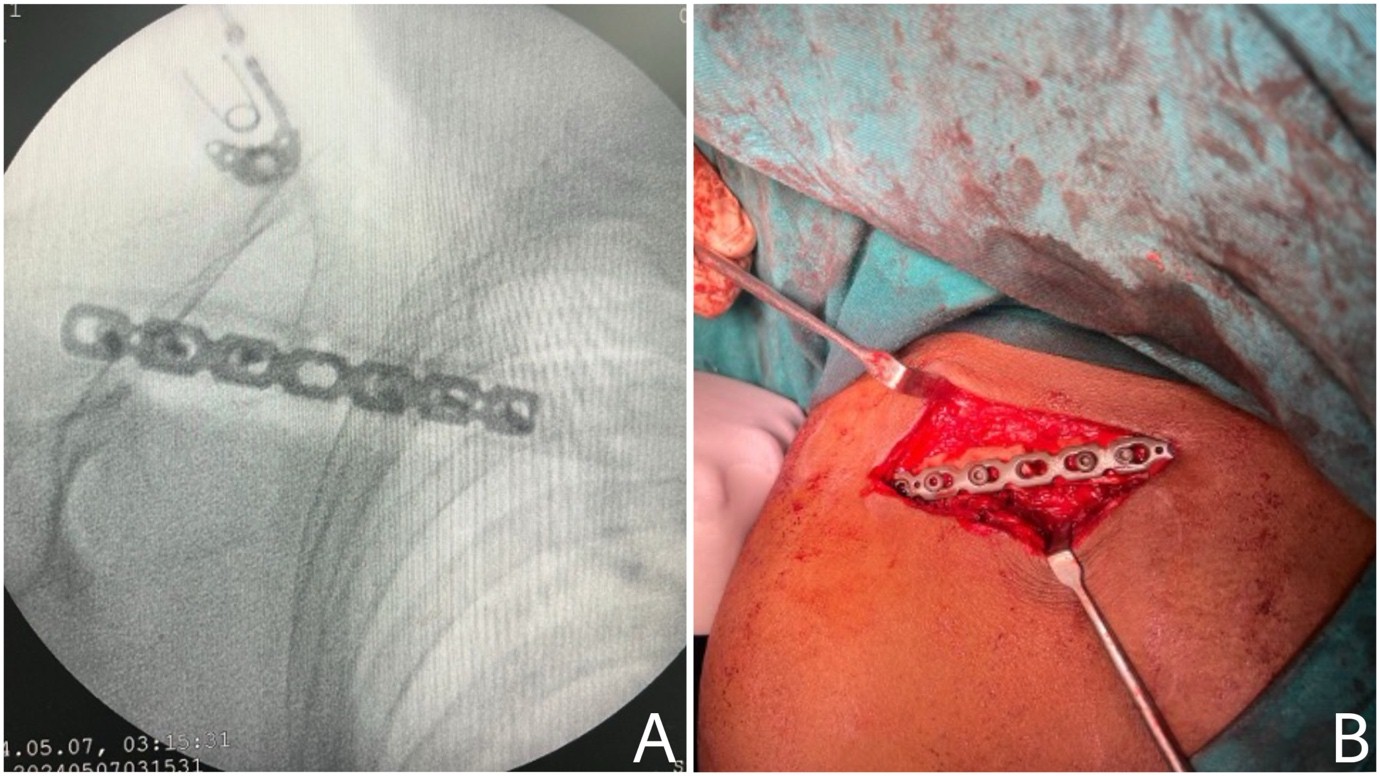
Figure 2: Intraoperative images illustrating the surgical procedure. *(a) Intraoperative C-arm imaging confirming proper implant positioning (b) Plate fixation following reduction.
The post-operative functional outcomes of patients who underwent anterior clavicle plating, as assessed by the CMS, are presented in Table 2.
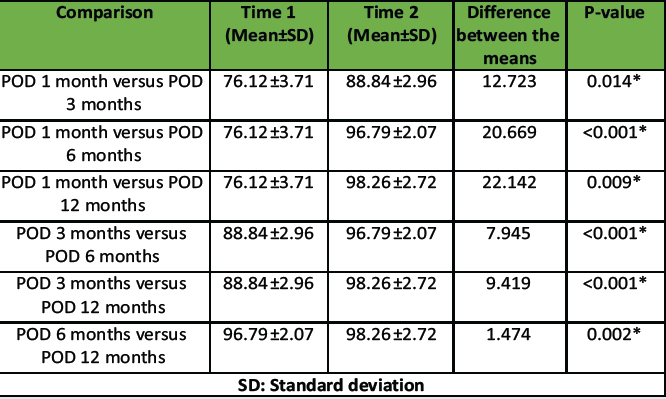
Table 2: Post-operative Constant-Murley score in patients undergoing anterior clavicle plating procedure
The post-operative CMSs revealed significant improvements in functional outcomes over time. At 1-month post-operatively, the mean score was 76.12 ± 3.71, which showed a statistically significant increase at 3 months (88.84 ± 2.96, P = 0.014). The score further improved at 6 months (96.79 ± 2.07) and 12 months (98.26 ± 2.72), demonstrating a significant mean difference compared to earlier time points (P < 0.001 for most comparisons). Fig. 3 shows a Line diagram illustrating the progressive increase in the CMS over time, indicating continuous improvement in shoulder function.
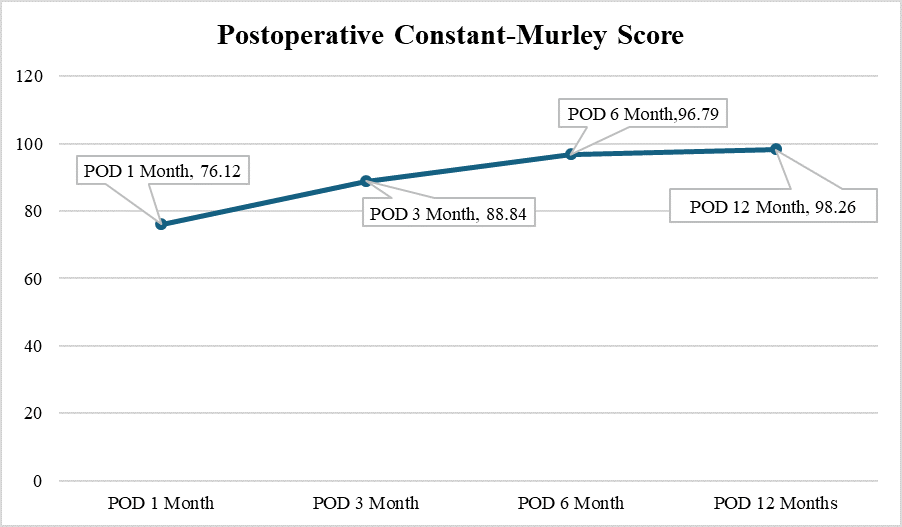
Figure 3: Line diagram showing the increase in post-operative constant-Murley score during the follow-up period.
These findings indicate a progressive enhancement in shoulder function following anterior clavicle plating, with substantial recovery occurring within the first 6 months and further minor improvements up to 1 year post-surgery. Fig. 4 shows the sequential radiographs demonstrating the progression of fracture healing over time. The pre-operative X-ray (Fig. 4a) showed a midshaft clavicle fracture, while the immediate post-operative X-ray (Fig. 4b) confirmed proper fracture alignment and stabilization following anterior clavicle plating. The 1-year follow-up X-ray in Zanca view (Fig. 4c) revealed complete bone union and stable implant positioning, indicating successful healing and restoration of clavicular integrity.
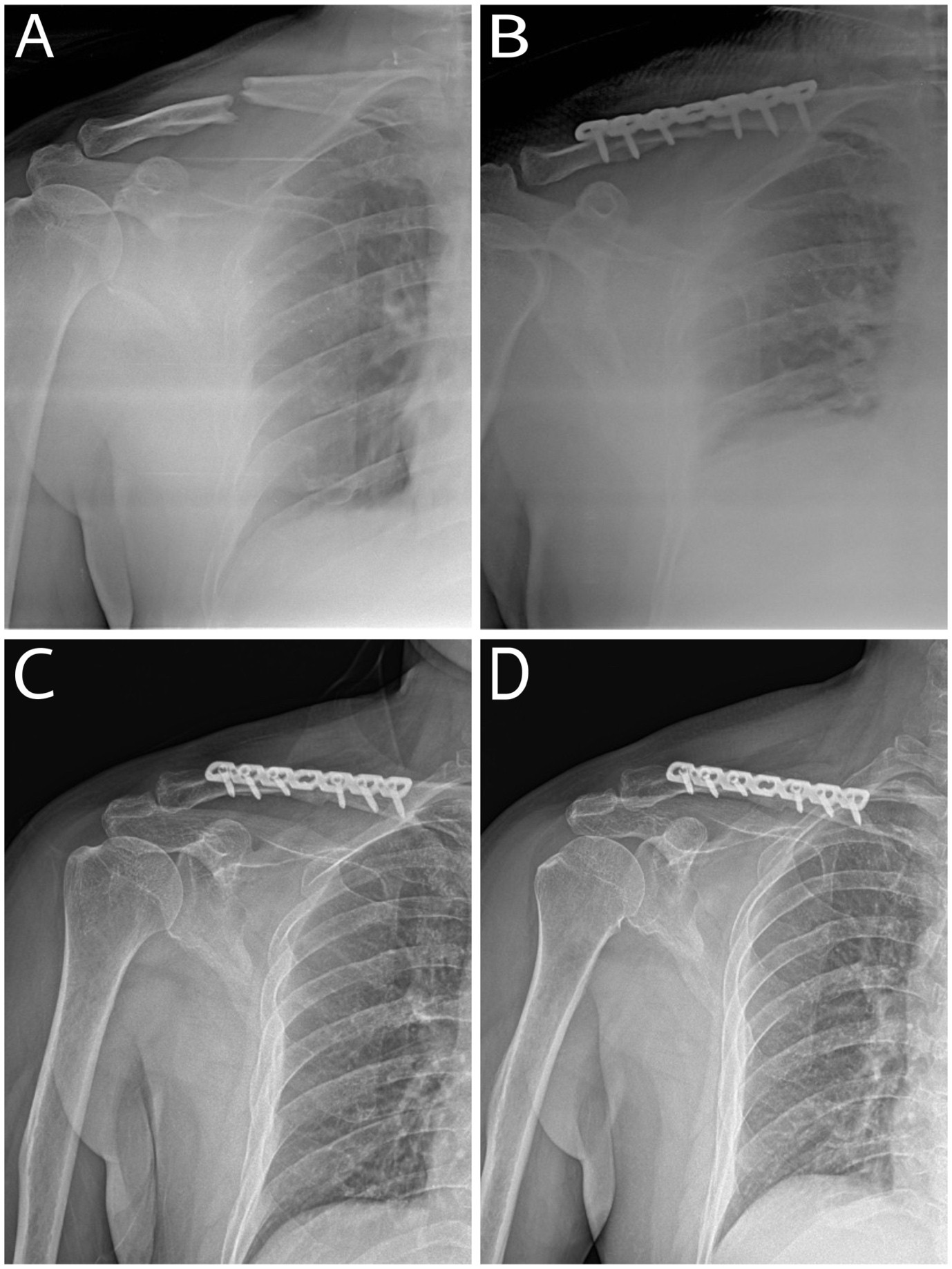
Figure 4: X-rays showing the progression of fracture healing over time. *(a) Pre-operative X-ray, (b) Immediate post-operative X-ray, (c) 3 months follow-up (d) 6 months follow-up.
Table 3 shows the RM-ANOVA Test of within-subject effects for the anterior clavicle plating procedure. The RM-ANOVA for within-subject effects in patients undergoing the anterior clavicle plating procedure demonstrated a statistically significant difference across the time points (F = 746.204, df = 3, P < 0.001). This indicates a significant improvement in functional outcomes over time following the procedure. Post-operative complications were observed in 4.8% of cases, including one patient suffering from a supraclavicular nerve sensory deficit and one suffering from a surgical site infection. Fig. 5 shows the clinical images demonstrating the range of motion in a patient 1 year after anterior clavicle plating.
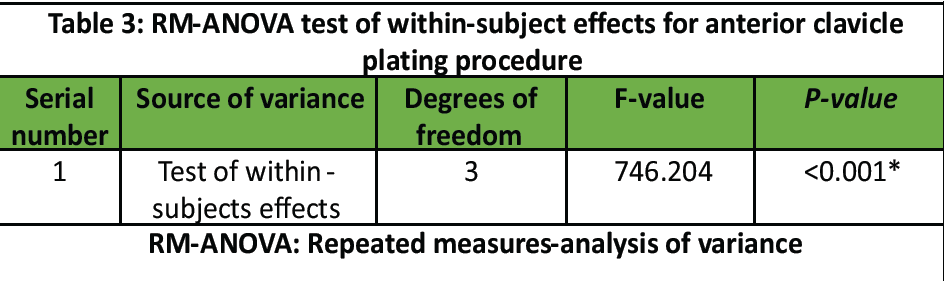
Table 3: RM-ANOVA test of within-subject effects for anterior clavicle plating procedure

Figure 5: Clinical pictures of a patient demonstrating the range of movements after 1 year of surgery.
Orthopedic surgeons often prefer non-operative management for non-displaced middle-third clavicle fractures, typically using a sling or a figure-of-8 brace. This conservative approach has shown effectiveness in promoting healing for many patients. Nevertheless, the treatment of acutely displaced clavicle midshaft fractures remains a point of contention within the medical field [7]. While the majority of middle-third clavicle fractures heal without significant complications, non-surgical management has been associated with an increased risk of non-union and lower patient satisfaction regarding functional outcomes and overall recovery. These concerns fuel the ongoing debate over the best approach for displaced fractures, underscoring the need for continued research and tailored treatment plans for individual patients [8]. Surgery is usually advised for midshaft fractures in the clavicle, under certain circumstances, such as open or impending open fractures, fractures involving displacement over 2 cm, “floating shoulder” injuries, fractures that result in significant shortening (more than 2 cm), multiple injuries where clavicle fixation could improve mobility and painful non-union, There is ongoing debate regarding the optimal surgical approach for the treatment of displaced mid-3rd fractures and various techniques for surgical stabilization have been suggested, including ORIF with plate osteosynthesis [9,10,11,12,13,14], intramedullary fixation [15,16,17,18], and external fixation [19,20,21]. This article discusses the assessment of functional outcomes and complications of anterior clavicle plating in the management of midshaft clavicle fractures at a tertiary care centre. About 42 patients were recruited in this study who had fractures of the mid-3rd of the clavicle and underwent anterior plating during a period of 1 year. The results are discussed below in detail with reference to findings of similar studies in the literature.
54.8% of the patients were between the age groups of 18 and 40 years. Similar findings were reported in studies conducted in various locations, where the mean age of patients with clavicle fractures predominantly fell within the middle-aged group [7,22,23,24]. Age plays a significant role in the treatment outcomes of clavicle fractures, as younger individuals typically exhibit better fracture healing capacity due to higher bone turnover rates and fewer comorbidities [25]. In contrast, older patients may experience delayed healing or complications, such as non-union or malunion, due to factors, such as osteoporosis and reduced regenerative potential [26]. About 69% of the participants were male, which could be due to the reason that male clavicles have a higher median breaking load (approximately 1200 N) compared to female clavicles (around 800 N) [27]. In addition, men are more likely to participate in high-risk activities, such as contact sports, which contribute to a higher incidence of clavicle fractures [28]. Furthermore, men typically have greater bone density and muscle mass, which can aid in achieving better fixation and faster functional recovery following treatment. In contrast, women, particularly those who are postmenopausal, often have reduced bone density due to osteoporosis, which increases the likelihood of complications, such as delayed healing, non-union, or implant-related issues. The right clavicle was fractured in 52.4% of participants, whereas 47.6% had a fracture in the left clavicle. In support of our finding, previous research work has shown that the right clavicle tends to be shorter, which may predispose it to fractures under certain conditions [29]. On the contrary, it has also been observed that the non-dominant side, typically the left for right-handed individuals, exhibits greater bone density, particularly in the middle and distal thirds, which may lead to increased fracture risk due to reduced flexibility [30]. Research works have reported that AO classification of clavicle fractures may help in predicting complications [31], but it does not necessarily correlate with long-term functionality [32], as other factors, such as surgical technique and patient characteristics, also play crucial roles in recovery and complication rates [33]. Although plating remains the standard surgical approach for managing displaced midshaft clavicle fractures, there is ongoing debate regarding the optimal plate positioning to achieve the best functional and biomechanical outcomes. Jupiter and Leffert [34] proposed that superior plating may provide biomechanical advantages over anterior plating, as the superior aspect of the clavicle is the primary load-bearing surface. This technique is thought to offer enhanced stability by directly counteracting the forces acting on the clavicle. However, one of the key limitations of superior plating is its susceptibility to the downward force exerted by the arm, which can compromise screw fixation in the osteoporotic or osteopenic lateral fragment. This mechanical disadvantage increases the likelihood of screw pullout, particularly in patients with reduced bone mineral density. Conversely, Kloen et al. [12] advocated for anterior plate positioning, arguing that this method functions as an inferior buttress and provides better support for the osteopenic lateral bone. The enhanced stability of the medial fixation in this approach strengthens the overall construct and minimizes the risk of screw loosening or pullout in the lateral fragment, which is a common concern with superior plating. In a biomechanical study evaluating various clavicle fracture plating techniques, Celestre et al. [35] assessed the mechanical properties of superior and anterior plating in terms of load-to-failure and bending stiffness. Their findings indicated that superior plating offered greater resistance to mechanical failure and superior bending stiffness when compared to anterior-inferior plating. However, anterior plating demonstrated superior axial compression stiffness, highlighting its potential advantage in maintaining fracture alignment under physiological loads. Notably, the study reported no statistically significant difference between the two plating techniques, suggesting that both methods have comparable biomechanical properties in clinical settings. Iannotti et al. [36] conducted a biomechanical study using a transverse osteotomy model to evaluate the influence of plate positioning on the mechanical stability of midshaft clavicle fractures. Their findings demonstrated that clavicles plated on the superior surface exhibited significantly greater biomechanical stability compared to those plated on the anterior aspect. This suggests that superior plating may offer enhanced resistance to mechanical forces acting on the clavicle during physiological activities. However, despite this advantage, their study did not find a statistically significant difference in load to failure between the two plating techniques, indicating that both methods may be biomechanically comparable in terms of their ability to withstand external forces before failure occurs. Similarly, Harnroongroj and Vanadurongwan [37] investigated the mechanical performance of different plating positions using a complex osteotomy model designed to replicate an unstable midshaft clavicle fracture. Their results indicated that anterior-inferior plating provided greater overall mechanical strength compared to superior plating. However, when applied to a simple transverse osteotomy model, anterior-inferior plating failed before superior plating, suggesting that the choice of plate positioning may need to be tailored to the specific fracture configuration. This highlights the importance of considering fracture morphology when determining the optimal surgical approach, as different plating techniques may offer distinct advantages depending on the stability of the fracture. The selection of the ideal plate position for midshaft clavicle fractures appears to be influenced by fracture pattern and stability rather than a universal biomechanical superiority of one technique over the other. While anterior plating may not significantly compromise mechanical stability, it has been suggested that this technique could impact post-operative outcomes, including complication rates and overall patient satisfaction. Given these findings, anterior plating may be particularly beneficial in cases involving unstable fractures, as observed in the present study. By providing a more robust fixation in unstable fracture configurations, anterior-inferior plating may contribute to improved fracture healing and reduce the likelihood of implant-related complications, thereby enhancing the overall clinical outcomes for patients undergoing surgical intervention for midshaft clavicle fractures. Clinical outcomes following clavicle fracture treatment have shown considerable variation, with a wide range of functional assessment tools being utilized. Among these, the CMS has been validated as a reliable prognostic indicator of shoulder function, demonstrating strong correlations with patient-reported outcomes and quality-of-life measures [38]. In comparative studies, the CMS at 1 year was significantly higher for surgical interventions (92.7) compared to conservative treatment, underscoring the benefits of operative management [39]. In the present study, patients who underwent anterior clavicle plating achieved predominantly good to excellent functional outcomes.
The paired t-test analysis of the post-operative CMS demonstrated significant improvements in functional outcomes over time, highlighting the efficacy of anterior clavicle plating in restoring shoulder function. The most notable progress was observed within the first 6 months after surgery, during which patients experienced substantial improvements in pain reduction, range of motion, strength, and activities of daily living. Similar results were observed by Maheshwari et al., [40] In their study, where the mean Constant-Murley shoulder scores significantly improved at 1-month, 2-month, and 4-month follow-ups, indicating a positive correlation between the scores and functional recovery. This rapid recovery phase can be attributed to effective surgical fixation, early rehabilitation, and the natural healing process of the fracture. Beyond the 6-month mark, functional gains were more gradual, with minor improvements noted up to 1-year post-surgery, likely reflecting the continued adaptation and strengthening of the shoulder. These findings underscore the significance of long-term follow-up and rehabilitation to maximize functional recovery after clavicle fracture treatment. The findings from the RMs ANOVA test, which demonstrated a statistically significant improvement in functional outcomes over time following anterior clavicle plating, align with the progressive nature of fracture healing and rehabilitation. This improvement can be attributed to the stabilization achieved through surgical fixation, which facilitates early mobilization, reduces pain, and promotes better alignment for optimal healing. In addition, the structured rehabilitation protocols post-surgery play a critical role in restoring shoulder strength, range of motion, and overall function. The consistent and gradual improvement across time points also highlights the significance of long-term follow-up and adherence to physiotherapy to achieve maximal functional recovery. These results further support the efficacy of anterior clavicle plating as a reliable intervention for managing midshaft clavicle fractures. Several studies have documented poor outcomes with conservative treatment, particularly in displaced or comminuted mid‑shaft clavicle fractures [41,42,43,44] Postacchini et al., [45] reported a 10.5% non-union rate even under carefully monitored conservative care. In a comparative cohort, Han et al. [46] observed a lower union rate (87.3% vs. 98.0%), longer time to union, and instances of malunion only in the non-operative group, despite comparable patient‑reported outcomes. Micheloni et al. [47] also demonstrated residual strength deficits and delayed healing in non-operatively managed patients with displaced mid‑shaft fractures. Even in adolescents, Kim et al. [48] reported that operative groups achieved faster functional recovery and improved alignment compared to conservative treatment using figure‑of‑8 bracing. With respect to post-operative complications, one patient experienced surgical site infection (superficial), and another suffered from supraclavicular nerve sensory deficit (hypoesthesia) without motor deficit. The incidence of these complications is relatively low, reflecting the safety and efficacy of anterior clavicle plating when performed using standard surgical techniques and with appropriate post-operative care. Mannan et al., [49] in their study reported similar findings, where 3.3% of the patients experienced superficial infection. Surgical site infections can be attributed to factors, such as prolonged surgical duration, poor wound hygiene, or patient-related factors, such as diabetes or smoking. After antero-inferior clavicle plating, the most common nerve issue is numbness or tingling around the incision because the small skin nerves (supraclavicular nerves) run unpredictably across the mid-clavicle [50]. Some patients notice early numbness that often improves over time, though a few may have mild persistent symptoms [51,52]. These changes are generally related to the surgical exposure itself and are not unique to anterior versus superior plate position; overall complication rates are similar between the two approaches [53]. Risk can be lowered by gentle soft-tissue handling, identifying and preserving visible nerve branches, and using smaller or minimally invasive exposures when appropriate [54,55]. Major nerve problems (such as brachial plexus irritation or palsy) are uncommon and are seen mainly in difficult cases, e.g., delayed fixation or non-unions with scarred tissue [56,57]. Preventive steps include careful release of adherent tissue, avoiding over-lengthening during reduction, using drill sleeves and appropriate screw lengths, and close post-operative monitoring [57]. Neurovascular injuries, although rare, emphasize the importance of meticulous surgical techniques to avoid damage to surrounding structures. Despite these complications, anterior plating is generally considered safe, with comparable outcomes to superior plating [58].
Anterior clavicle plating is a safe and effective surgical option for midshaft clavicle fractures, yielding excellent functional outcomes with a low complication rate. Placing the plate on the anterior aspect of the clavicle helps reduce risks associated with the superior approach, such as discomfort caused by prominent hardware and possible injury to underlying neurovascular structures. Anterior clavicle plating is better than superior clavicle plating in certain fracture patterns. This technique is particularly advantageous in tertiary care centres, where comprehensive expertise and resources ensure optimal patient care.
Anterior clavicle plating has gained recognition as an effective alternative to traditional superior clavicle plating, especially in cases involving specific fracture types, such as coronal split fractures and vertical split fractures. This approach presents multiple benefits, such as a lower risk of neurovascular injury and reduced hardware irritation, while still maintaining sufficient stability for proper fracture healing. By placing the plate on the anterior side of the clavicle, the technique minimizes the risks inherent in the superior approach, including discomfort from prominent hardware and potential harm to the underlying neurovascular structures. Furthermore, anterior plating supports optimal alignment and secure fixation, promoting successful healing and reducing the chances of complications, such as non-union or malunion.
References
- 1. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002;11:452-6. [Google Scholar] [PubMed]
- 2. Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: Epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; An observational study. BMC Musculoskelet Disord 2017;18:82. [Google Scholar] [PubMed]
- 3. Jiang H, Qu W. Operative treatment of clavicle midshaft fractures using a locking compression plate: Comparison between mini-invasive plate osteosynthesis (MIPPO) technique and conventional open reduction. Orthop Traumatol Surg Res 2012;98:666-71. [Google Scholar] [PubMed]
- 4. Chen CE, Juhn RJ, Ko JY. Anterior-inferior plating of middle-third fractures of the clavicle. Arch Orthop Trauma Surg 2010;130:507-11. [Google Scholar] [PubMed]
- 5. Teunissen JS, Al Shaer S, Van Der Heijden BP, Selles RW, Hovius SE, Zöphel OT, et al. The association between plate location and hardware removal following ulna shortening osteotomy: A cohort study. J Hand Surg Eur Vol 2022;47:831-8. [Google Scholar] [PubMed]
- 6. Rivera-Saldívar G, Manrique-Ávila JA. Superior versus anteroinferior plating for mid-shaft clavicle fractures: A randomized clinical trial. Cir Cir 2024;92:141-9. [Google Scholar] [PubMed]
- 7. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD, Evidence-based orthopaedic trauma working group. Treatment of acute midshaft clavicle fractures: Systematic review of 2144 fractures: On behalf of the evidence-based orthopaedic trauma working group. J Orthop Trauma 2005;19:504-7. [Google Scholar] [PubMed]
- 8. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997;79:537-9. [Google Scholar] [PubMed]
- 9. Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury 1999;30:497-500. [Google Scholar] [PubMed]
- 10. Poigenfürst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: Results of 122 operations. Injury 1992;23:237-41. [Google Scholar] [PubMed]
- 11. Mullaji AB, Jupiter JB. Low-contact dynamic compression plating of the clavicle. Injury 1994;25:41-5. [Google Scholar] [PubMed]
- 12. Kloen P, Sorkin AT, Rubel IF, Helfet DL. Anteroinferior plating of midshaft clavicular nonunions. J Orthop Trauma 2002;16:425-30. [Google Scholar] [PubMed]
- 13. Rockwood CA, Green DP, Bucholz RW, editors. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006. [Google Scholar] [PubMed]
- 14. Post M. Current concepts in the treatment of fractures of the clavicle. Clin Orthop Relat Res 1989;245:89-101. [Google Scholar] [PubMed]
- 15. Ngarmukos C, Parkpian V, Patradul A. Fixation of fractures of the midshaft of the clavicle with Kirschner wires. Results in 108 patients. J Bone Joint Surg Br 1998;80:106-8. [Google Scholar] [PubMed]
- 16. Boehme D, Curtis RJ Jr., DeHaan JT, Kay SP, Young DC, Rockwood CA Jr. Non-union of fractures of the mid-shaft of the clavicle. Treatment with a modified Hagie intramedullary pin and autogenous bone-grafting. J Bone Joint Surg Am 1991;73:1219-26. [Google Scholar] [PubMed]
- 17. Capicotto PN, Heiple KG, Wilbur JH. Midshaft clavicle nonunions treated with intramedullary Steinman pin fixation and onlay bone graft. J Orthop Trauma 1994;8:88-93. [Google Scholar] [PubMed]
- 18. Hoogervorst P, Van Dam T, Verdonschot N, Hannink G. Functional outcomes and complications of intramedullary fixation devices for midshaft clavicle fractures: A systematic review and meta-analysis. BMC Musculoskelet Disord 2020;21:395. [Google Scholar] [PubMed]
- 19. Schuind F, Pay-Pay E, Andrianne Y, Donkerwolcke M, Rasquin C, Burny F. External fixation of the clavicle for fracture or non-union in adults. J Bone Joint Surg Am 1988;70:692-5. [Google Scholar] [PubMed]
- 20. Nowak J, Rahme H, Holgersson M, Lindsjö U, Larsson S. A prospective comparison between external fixation and plates for treatment of midshaft nonunions of the clavicle. Ann Chir Gynaecol 2001;90:280-5. [Google Scholar] [PubMed]
- 21. Barlow T, Upadhyay P, Barlow D. External fixators in the treatment of midshaft clavicle non-unions: A systematic review. Eur J Orthop Surg Traumatol 2014;24:143-8. [Google Scholar] [PubMed]
- 22. Li H. Surgical and nonsurgical treatment of clavicular midpiece fracture in adults: A case-control study. Zhongguo Gu Shang 2012;25:278-81. [Google Scholar] [PubMed]
- 23. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998;80:476-84. [Google Scholar] [PubMed]
- 24. Shrestha R. Outcome of surgical management of clavicle shaft fracture in adult. Int J Sci Res Arch 2024;13:2216-21. [Google Scholar] [PubMed]
- 25. Clark D, Nakamura M, Miclau T, Marcucio R. Effects of aging on fracture healing. Curr Osteoporos Rep 2017;15:601-8. [Google Scholar] [PubMed]
- 26. Meinberg EG, Clark D, Miclau KR, Marcucio R, Miclau T. Fracture repair in the elderly: Clinical and experimental considerations. Injury 2019;50 Suppl 1:S62-5. [Google Scholar] [PubMed]
- 27. Hoyer HE, Kindt R, Lippert H. Studies on the biomechanics of the human clavicle. Z Orthop Ihre Grenzgeb 2008;118:915-22. [Google Scholar] [PubMed]
- 28. Kostecki B, Jurek A, Klocek K, Hajduk A, Mrozek L, Zwolski M, et al. Clavicle fractures – epidemiology, biomechanics of injury and treatment methods. J Educ Health Sport 2023;14:216-32. [Google Scholar] [PubMed]
- 29. Mays S, Steele J, Ford M. Directional asymmetry in the human clavicle. Int J Osteoarchaeol 1999;9:18-28. [Google Scholar] [PubMed]
- 30. Teodoro Ezequiel Guerra M, Isabel Pozzi M, Busin G, Crestana Zanetti L, Antônio Lazzarotto Terra Lopes J, Orso V. Densitometric study of the clavicle: Bone mineral density explains the laterality of the fractures. Rev Bras Ortop 2014;49:468-72. [Google Scholar] [PubMed]
- 31. Josue-Coicou Charles S, Chen S, Mittwede P, Moloney G, Lin A. Podium presentation title: BMI and fracture pattern as predictors of postoperative complications in midshaft clavicle fractures. Arthroscopy J Arthrosc Related Surg 2023;39:e29. [Google Scholar] [PubMed]
- 32. Lopiz Y, Rodriguez-Zamorano P, Díaz MD, García-Fernandez C, Marco F. Long-Term Functional Outcomes after Surgical Treatment of Displaced Midshaft Clavicle Fractures: A Retrospective Cohort Study. [Preprint]; 2024. [Google Scholar] [PubMed]
- 33. Patel YC, Lathiya HR, Shah SA, Majumda S, Gohil PD. A study of functional outcome of clavile fractures treated by clavicle plating. Int J Orthop Sci 2023;9:559-66. [Google Scholar] [PubMed]
- 34. Jupiter JB, Leffert RD. Non-union of the clavicle. Associated complications and surgical management. J Bone Joint Surg Am 1987;69:753-60. [Google Scholar] [PubMed]
- 35. Celestre P, Roberston C, Mahar A, Oka R, Meunier M, Schwartz A. Biomechanical evaluation of clavicle fracture plating techniques: Does a locking plate provide improved stability? J Orthop Trauma 2008;22:241-7. [Google Scholar] [PubMed]
- 36. Iannotti MR, Crosby LA, Stafford P, Grayson G, Goulet R. Effects of plate location and selection on the stability of midshaft clavicle osteotomies: A biomechanical study. J Shoulder Elbow Surg 2002;11:457-62. [Google Scholar] [PubMed]
- 37. Harnroongroj T, Vanadurongwan V. Biomechanical aspects of plating osteosynthesis of transverse clavicular fracture with and without inferior cortical defect. Clin Biomech (Bristol) 1996;11:290-4. [Google Scholar] [PubMed]
- 38. Akbar AA, Mustari MN, Latief J, Hamid F, Bausat A, Laidding SR, et al. Comparison of constant and murley scores between operatively and nonoperatively managed midshaft clavicle fractures in Makassar, Indonesia. Gazz Med Ital Arch Sci Med 2023;182:202-7. [Google Scholar] [PubMed]
- 39. Kumar K, Kapila R, Singh R, Chaudhary P. Clinical and radiological outcome of three treatment modalities for fracture clavicle: A comparative prospective study. J Clin Sci Res 2024;13:207-15. [Google Scholar] [PubMed]
- 40. Maheshwari P, Peshin C, Agarwal D. Functional outcomes in surgically treated clavicle fractures: A longitudinal observational study. Cureus 2023;15:e48081. [Google Scholar] [PubMed]
- 41. Matsubara Y, Nakamura Y, Sasashige Y, Yokoya S, Adachi N. Long-term conservative treatment outcomes for midshaft clavicle fractures: A 10-to-30-year follow-up. J Orthop Surg Res 2023;18:952. [Google Scholar] [PubMed]
- 42. Kumar AV, Ramachandra Kamath K, Salian PR, Krishnamurthy SL, Annappa R, Keerthi I. Operative stabilisation versus non-operative management of mid-shaft clavicle fractures. SICOT J 2022;8:45. [Google Scholar] [PubMed]
- 43. Pal CP, Shakunt RK, Kumar D, Goyal A, Tyagi AP, Pippal TC. Functional outcome of conservative and surgical management in mid-third clavicle fractures. J Orthop Traumatol Rehabil 2015;8:11-5. [Google Scholar] [PubMed]
- 44. Micheloni GM, Tarallo L, Porcellini G, Catani F. Comparison between conservative treatment and plate fixation for displaced middle third clavicle fracture: Clinical outcomes and complications. Acta Biomed 2019;90:48-53. [Google Scholar] [PubMed]
- 45. Postacchini R, Gumina S, Farsetti P, Postacchini F. Long-term results of conservative management of midshaft clavicle fracture. Int Orthop 2010;34:731-6. [Google Scholar] [PubMed]
- 46. Han X, Zhang Y, Zhang X, Tan J. Comprehensive comparison between conservative therapy and surgical management for completely displaced and comminuted mid-shaft clavicle fractures. Int Orthop 2024;48:1871-7. [Google Scholar] [PubMed]
- 47. Pal CP, Shakunt RK, Kumar D, Goyal A, Tyagi A, Aditya P, et al. Functional outcome of conservative and surgical management in mid-third clavicle fractures. J Orthop Traumatol Rehabil 2015;8:11. [Google Scholar] [PubMed]
- 48. Kim HY, Yang DS, Bae JH, Cha YH, Lee KW, Choy WS. Clinical and radiological outcomes after various treatments of midshaft clavicle fractures in adolescents. Clin Orthop Surg 2020;12:396-403. [Google Scholar] [PubMed]
- 49. Mannan M, Hafeez U, Hassan A, Tahir R, Ajnin S. Functional outcomes of clavicle open reduction and internal fixation (ORIF). Cureus 2024;16:e72048. [Google Scholar] [PubMed]
- 50. Nathe T, Tseng S, Yoo B. The anatomy of the supraclavicular nerve during surgical approach to the clavicular shaft. Clin Orthop Relat Res 2011;469:890-4. [Google Scholar] [PubMed]
- 51. Ou L, Yang L, Zhao J, Su W. Cutaneous paresthesia after internal plate fixation of clavicle fractures and underlying anatomical observations. Medicine (Baltimore) 2018;97:e12729. [Google Scholar] [PubMed]
- 52. Lemieux V, Afsharpour S, Nam D, Elmaraghy A. Incisional paresthesia following clavicle plate fixation: Does it matter to patients? BMC Musculoskelet Disord 2021;22:928. [Google Scholar] [PubMed]
- 53. Nolte PC, Tross AK, Studniorz J, Grützner PA, Guehring T, Schnetzke M. No difference in mid-term outcome after superior vs. Anteroinferior plate position for displaced midshaft clavicle fractures. Sci Rep 2021;11:22101. [Google Scholar] [PubMed]
- 54. Liu LT, Chen JC, Yang TC, Tseng HJ, Yen SH, Lu CC, et al. Minimally invasive plate osteosynthesis with mini-open technique and supraclavicular nerve preservation reduces postoperative numbness in acute displaced midshaft clavicle fracture. Medicina (Kaunas) 2024;60:1669. [Google Scholar] [PubMed]
- 55. You JM, Wu YS, Wang Y. Comparison of post-operative numbness and patient satisfaction using minimally invasive plate osteosynthesis or open plating for acute displaced clavicular shaft fractures. Int J Surg 2018;56:21-5. [Google Scholar] [PubMed]
- 56. Cao Z, Hou Y, Su X, Teng M, Ji W, Li M. Brachial plexus injury after clavicle fracture operation: A case report and literature review. BMC Surg 2021;21:337. [Google Scholar] [PubMed]
- 57. Ashman BD, Tewari A, Castle J, Hasan SS, Bhatia S. Intraoperative neuromonitoring for brachial plexus neurolysis during delayed fixation of a clavicular fracture presenting as thoracic outlet syndrome: A case report. JBJS Case Connect 2018;8:e85. [Google Scholar] [PubMed]
- 58. El-Safty AM, Mesbah H, Hesham B, Refaat M. Superior versus anterior plating of midshaft clavicle fractures: 6 months follow up (union rates, risks, and complications: Hardware irritation and need for removal). Egypt Orthop J 2024;59:274-8. [Google Scholar] [PubMed]