Giant cell tumor of the tendon sheath (GCTTS) should be considered in the differential diagnosis of painless, slow-growing swellings of the fingers. Accurate pre-operative imaging, particularly MRI, along with meticulous surgical excision and histopathological confirmation, is crucial to achieving optimal outcomes and minimizing recurrence.
Dr. Naman K Parakh, Department of Orthopaedics, Teerthanker Mahaveer Medical College and Research Centre, Moradabad, Uttar Pradesh, India. E-mail: namanparakh1604@gmail.com
Introduction: Giant cell tumor of the tendon sheath (GCTTS) is a benign, slow-growing soft tissue neoplasm that typically arises from the synovial lining of tendon sheaths in the hand and digits. It is the second most common soft tissue tumor of the hand after ganglion cysts. While benign, GCTTS is locally aggressive and has a documented recurrence rate of up to 45%.
Materials and Methods: We present a case series of 8 patients diagnosed with GCTTS involving flexor and extensor tendons of the hand. All patients underwent thorough clinical evaluation and magnetic resonance imaging (MRI), assessment before complete surgical excision. Histopathological confirmation was obtained in each case.
Results: There was a female preponderance with 5 patients being females. The mean age of patients was 30.8 years. At a mean follow-up of 55 months (range: 48–62 months), recurrence was observed in one case.
Conclusion: GCTTS should be considered in the differential diagnosis of digital swellings. MRI is essential for surgical planning, and complete resection with preservation of critical structures minimizes the risk of recurrence. A multidisciplinary approach combining imaging, surgery, and pathology ensures optimal patient outcomes.
Keywords: Giant cell tumor, tendon sheath, flexor tendon, hand tumor, magnetic resonance imaging, recurrence, histopathology.
Giant cell tumor of the tendon sheath (GCTTS) is a benign proliferative lesion, most commonly found in the hands and feet. It is mostly seen in the third to fifth decade of life and has a slight female preponderance [1].
The pathogenesis of GCTTS is unclear. A number of theories suggest inflammatory, traumatic, lipid metabolism disorders, osteoclastic proliferation, autoimmune mechanisms, neoplasia, and metabolic disorders as the underlying cause of GCTTS [2].
Despite its benign nature, local recurrence after surgical excision has been reported in 20% cases. Although radiotherapy may aid in reducing the recurrence, this complication has been an issue in the treatment of cases of GCTTS [3].
We present a series of 8 cases of GCTTS involving the hand, the management strategy, and outcomes supplemented by a review of existing literature pertaining to the epidemiology, presentation, the surgical protocol, and the recurrence rates along with an insight into the cause of recurrence.
This case series was conducted on 8 patients presenting with a hand lesion to a tertiary care center between January 2020 and December 2021. Ethical clearance was obtained from the Institutional Ethics Committee (IEC number- TMU/IEC/2025-26/63). All patients with a confirmed clinico-radiological diagnosis of GCTTS of the hand using standard radiographs and magnetic resonance imaging (MRI) were included in the study. Tendon and bone involvement were studied extensively in the MRI before the surgical procedure. A well-informed consent was taken from all patients.
Surgical technique
All cases were posted for surgical intervention after a Pre-Anesthetic Checkup. Bier’s block was given in all cases and was operated with tourniquet control. A standard mid-lateral or Bruner type volar incision was used depending upon the site of the tumor. Using a ×4.5 magnifying loupe, meticulous dissection was done and the tumor was resected along with its capsule with a margin of normal tissue. The integrity of the tendon was checked continuously during the dissection by flexion and extension of the affected finger. The resected tumor was sent for further histopathological examination. Tendon integrity was checked at the end of the surgical procedure by the proper range of motion of the affected finger. The surgical site was carefully examined for any additional or satellite lesions. A thorough wash with hydrogen peroxide and normal saline was given at the end of the procedure to address any GCT remnants. Closure was done using interrupted non-absorbable sutures (Ethilon 4-0). A standard post-operative antibiotic protocol was followed. Radiotherapy was not used postoperatively in any patient unless there was any evidence of recurrence in follow-up MRI.
Of the 8 patients included in the study, 5 were female and 3 were male. The mean age of the patients was 30.8 years (range: 26–38 years). The most common location was the index finger (4/8), whereas the flexor tendons were more commonly affected (5/8). The mean duration of symptoms before surgical intervention was 10.3 months (Table 1).
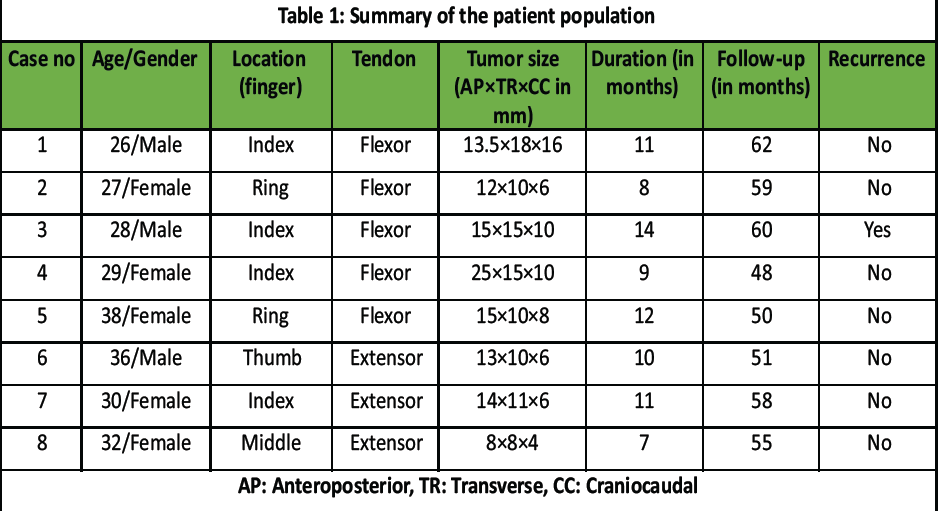
Table 1: Summary of the patient population
2 of the tumors were abutting the adjoining tendon, whereas 1 involved the digital neurovascular structure. None of the tumors had evidence of underlying bone erosion.
All patients had complete joint function after the surgery with mild-to-moderate pain in the immediate post-operative period which later subsided with medications. The mean follow-up period was 55 months. Recurrence was reported in 1 patient who underwent repeat surgical excision of the tumor.
On gross appearance, the tumor masses were firm and lobulated with a fibrous capsule of varying thickness. Histological examination showed hemosiderin deposition and the tumors were composed of 4 cellular types – macrophagic mononuclear cells, epithelioid histiocyte-like cells, xanthomatous cells, and osteoclast-like giant cells. Mitotic figures and apoptotic bodies were found in all the specimens (Figs. 1 and 2).
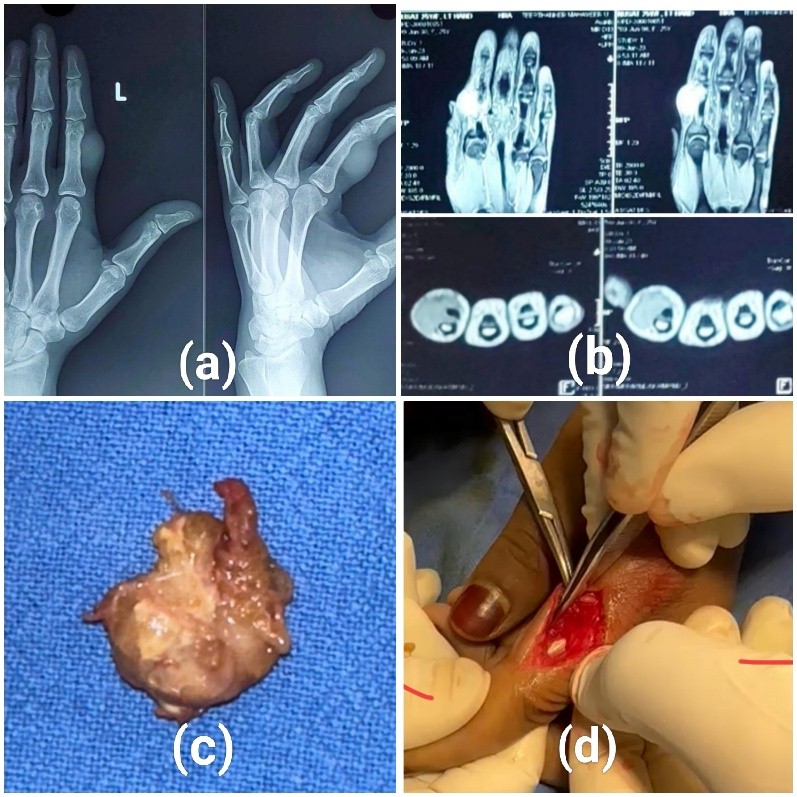
Figure 1: Case of giant cell tumor of the tendon sheath of the flexor digitorum profundus tendon of the index finger. (a) Plain radiograph of the affected hand. (b) Coronal and axial sections of the magnetic resonance imaging of the affected hand showing tumor over the lateral aspect of the index finger at the level of A3 pulley. (c) Gross appearance of the resected tumor. (d) Surgical site after complete resection of the tumor.
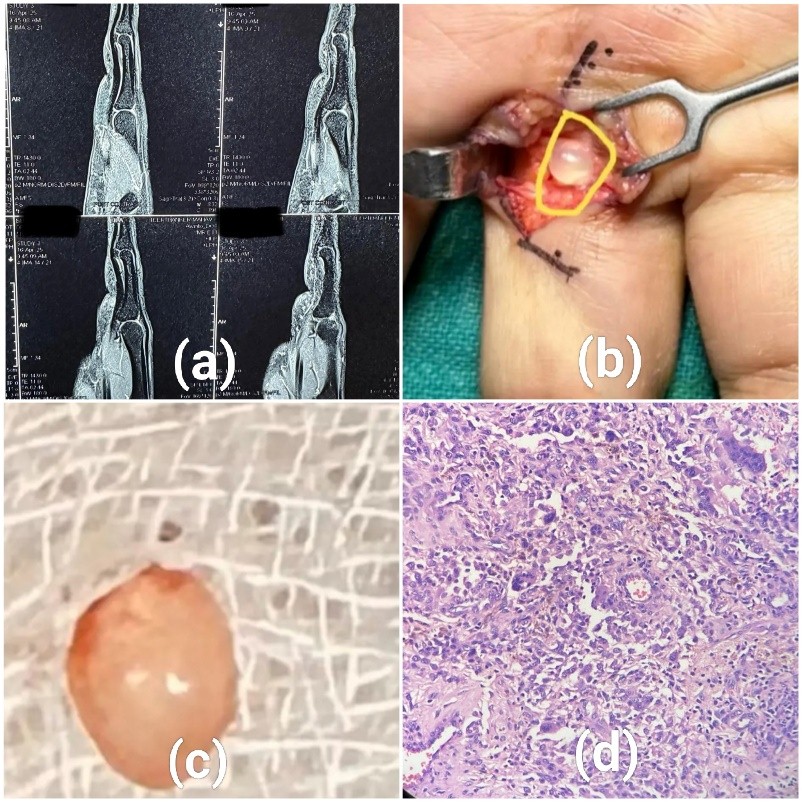
Figure 2: Case of giant cell tumor of the tendon sheath of the flexor tendon of middle finger. (a) Sagittal magnetic resonance images showing a small tumor over the flexor digitorum tendon of the middle finger. (b) Intraoperative image of the tumor. (c) Gross appearance of the tumor after complete resection. (d) Microscopic imaging of the tumor.
GCTTS is the second most common tumor of the hand following ganglion cysts. The differential diagnosis of GCTTS includes neurofibroma, pyogenic granuloma, desmoidoma, and malignant fibrous histiocytoma [2].
As reported by multiple studies, it has a peak incidence in the third to fifth decade of life and has a slight female preponderance. These tumors usually occur on the volar surface of the hand most commonly involving the index finger. This is consistent with the findings in our study where the mean age is 30.8 years with a majority of patients being females (62.5%) and the index finger and flexor tendons are more commonly affected than the others [1,3,4,5].
MRI is the gold standard for the diagnosis of GCTTS. Although, various authors have postulated the use of clinical examination, fine needle aspiration cytology and Ultrasonography as the diagnostic modalities with good results. All the patients in our study underwent MRI for the diagnosis of GCTTS and the excised tumor was later sent for histopathological examination to confirm the presence of hemosiderin deposition and giant cells [3,4,5,6,7,8].
Associated bony involvement in GCTTS of the hand presents as bony erosions on plain radiographs and MRI and poses a further risk of complications like degenerative joint changes and stiffness of fingers. Involvement of surrounding neurovascular structures increases the chances of incomplete tumor excision. Hence, intra and extraosseous involvement of the tumor is a predictive factor for recurrence in such cases [3].
Recurrence in GCTTS is the most important complication which needs further evaluation for its causes and methods of prevention. Meticulous excision of the tumor while having proper exposure, complete removal of the tendon sheath and satellite lesions along with evaluation for local invasion of the tumor preferably with the use of a microscope or magnification significantly reduces the incidence of recurrence in cases of GCTTS. In addition to this, radiotherapy may serve as an adjuvant to further eliminate the possibility of recurrence [2,4,6].
The variable demography, diagnostic modalities, recurrence rates, and the use of radiotherapy in existing literature warrant a detailed insight into these aspects of the tumor to further strengthen a management plan to achieve better surgical outcomes (Table 2).
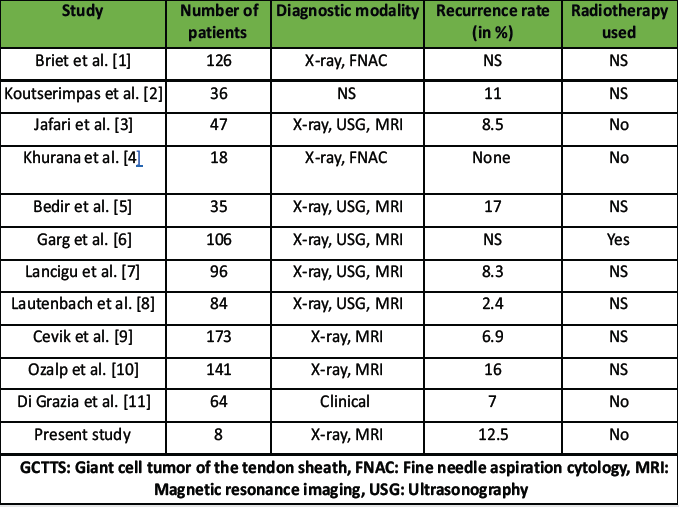 Table 2: Summary of previous studies on GCTTS of the hand highlighting the diagnostic modalities, recurrence rate, and use of radiotherapy
Table 2: Summary of previous studies on GCTTS of the hand highlighting the diagnostic modalities, recurrence rate, and use of radiotherapy
GCTTS is a benign but locally aggressive tumor commonly affecting the hand. Clinical suspicion, MRI evaluation, and histopathological confirmation are essential for diagnosis. Complete and meticulous surgical excision under magnification remains the treatment of choice, ensuring minimal recurrence. Long-term follow-up is necessary to monitor for recurrence, particularly in recurrent or inadequately excised lesions.
Similar to other studies, there were limitations to our study. It is a single-center study with a short-term follow-up and hence provides only a preliminary insight into long-term outcomes and the occurrence of recurrence in this small group of patients.
GCTTS presents a slow-growing, benign lesion most commonly seen in the hands and feet. The diagnosis and management of this disease hold paramount importance to prevent recurrence and morbidity in the affected population. Meticulous dissection and a vigilant approach to identify satellite or additional lesions are important to prevent the risk of recurrence in GCTTS.
References
- 1. Briët JP, Becker SJ, Oosterhoff TC, Ring D. Giant cell tumor of tendon sheath. Archives of Bone and Joint Surgery. 2015 Jan 15;3(1):19. [Google Scholar] [PubMed]
- 2. Koutserimpas C, Kastanis G, Ioannidis A, Filippou D, Balalis K. Giant cell tumors of the tendon sheath of the hand: an 11-year retrospective study. Statistics. 2018 Sep 1;10:11. [Google Scholar] [PubMed]
- 3. Jafari D, Shariatzadeh H, Najd Mazhar F, Razavipour M, Okhovatpour MA. Giant cell tumor of tendon sheath of the hand: experience with forty-seven cases. Journal of Research in Orthopedic Science. 2015 Feb 10;2(1):0-. [Google Scholar] [PubMed]
- 4. Khurana A, Singh JP, Preeti, Littlefield Z, Young S, Shah A. Demystifying giant cell tumours of tendon sheath (GCTTS): a case series of 18 cases with review of literature. Indian Journal of Orthopaedics. 2023 Nov;57(11):1858-73. [Google Scholar] [PubMed]
- 5. Bedir R, Balik MS, Sehitoglu I, Güçer H, Yurdakul C (2014) Giant cell tumour of the tendon sheath: analysis of 35 cases and their Ki-67 proliferation indexes. J Clin Diagn Res 8(12):FC12-5. 10.7860/JCDR/2014/10553.5311 [Google Scholar] [PubMed] [CrossRef]
- 6. Garg B, Kotwal PP. Giant cell tumour of the tendon sheath of the hand. Journal of Orthopaedic Surgery. 2011 Aug;19(2):218-20. [Google Scholar] [PubMed]
- 7. Lancigu R, Rabarin F, Jeudy J, et al. Giant cell tumors of the tendon sheaths in the hand: review of 96 patients with an average follow-up of 12 years. Orthop Traumatol Surg Res 2013; 99(4 Suppl): 251–254. [Google Scholar] [PubMed]
- 8. Lautenbach M, Kim S, Millrose M, Eisenschenk A. Nodular giant cell tumour of the tendon sheath of the hand: Analysis of eighty-four cases—diagnostic decisions and outcome. International Orthopaedics (SICOT). 2013;37(11):2211–2215. doi: 10.1007/s00264-013-1994-2. [Google Scholar] [PubMed] [CrossRef]
- 9. Çevik HB, Kayahan S, Eceviz E, Gümüştaş SA. Tenosynovial giant cell tumor in the hand: experience with 173 cases. The Journal of Hand Surgery (Asian-Pacific Volume). 2020 Jun;25(02):158-63. [Google Scholar] [PubMed]
- 10. Ozalp T, Yercan H, Kurt C, Ozdemir O, Coskunol E. Giant-cell tumors of the tendon sheath involving the hand or the wrist: an analysis of 141 patients. Acta orthopaedica et traumatologica turcica. 2004 Jan 1;38(2):120-4. [Google Scholar] [PubMed]
- 11. Di Grazia S, Succi G, Fraggetta F, Perrotta RE. Giant cell tumor of tendon sheath: study of 64 cases and review of literature. Il Giornale di Chirurgia-Journal of the Italian Surgical Association. 2013 May 1;34(5):149-52. [Google Scholar] [PubMed]