Intramedullary nailing is an effective and biomechanically sound treatment for pathological long bone fractures, offering pain relief, early mobilization, and improved quality of life through individualized surgical planning.
Dr. Manmohan Singh, Department of Orthopaedic Surgery, Guru Gobind Singh Medical College, Faridkot, Punjab, India. E-mail: doctormanmohan@yahoo.com
Introduction: Pathological fractures resulting from metastatic bone involvement, multiple myeloma (MM), and atypical femoral fractures present complex therapeutic challenges. Intramedullary (IM) nailing offers a biomechanically stable solution that facilitates early mobilization and enhances functional outcomes. This case series aims to evaluate the clinical and radiological results of IM fixation in pathological fractures, emphasizing pain relief and early functional outcomes.
Case Series: We report a series of five patients with pathological fractures of long bones who underwent IM nailing, including cases of carcinoma breast, MM, hepatocellular carcinoma, and large B-cell lymphoma involvement. The cohort encompassed the geriatric age group and fracture locations, predominantly involving the femur and humerus. Surgical management utilized long IM nails and locked humeral nails. Results demonstrated significant pain reduction, early weight-bearing capability, and satisfactory union rates, with a low incidence of complications.
Conclusion: IM nailing represents an effective and dependable approach for stabilizing pathological long bone fractures, promoting rapid symptomatic improvement and functional recovery. This series substantiates the role of fixation as a cornerstone in the surgical management of pathological fractures, providing valuable insights into fixation techniques and patient outcomes.
Keywords: Pathological fractures, intramedullary nailing, metastatic bone disease, atypical femoral fractures.
Pathologic fracture of the long bones is a common complication of bone metastases [1]. They are Substantially impacting quality of life and functional capacity. These fractures occur when normal physiological loads exceed the mechanical strength of bone weakened by underlying disease processes, most commonly metastatic deposits from primary malignancies, including breast, prostate, lung, kidney, and thyroid cancers. The incidence of pathological fractures is rising due to improved diagnosis and treatment of metastatic disease, leading to prolonged patient survival and increased skeletal involvement. As patients with cancer live longer, the incidence of metastatic bone disease (MBD) is also increasing; however, accurate figures are not readily available for how many of these patients will develop skeletal metastases [2]. The surgical management of pathological fractures presents unique challenges distinct from traumatic fracture care. These fractures occur in the context of a progressive systemic disease and are characterized by impaired healing potential due to the abnormal bone environment created by tumor infiltration. It is reported that 23% of pathological fractures occur in the femoral subtrochanteric region [3]. The primary goals of surgical intervention are pain relief, restoration of function, prevention of further fracture progression, and maintenance of skeletal stability for the remainder of the patient’s life. Given the palliative nature of treatment in most cases, surgical strategies must balance durability of fixation with operative morbidity while considering patient life expectancy. Intramedullary (IM) fixation has emerged as the preferred surgical technique for pathological fractures of long bones, offering several biomechanical and clinical advantages over alternative fixation methods. IM nails offer several advantages: they protect a long segment of bone, the necessary dissection is relatively small, blood supply to the periosteum is preserved, and rigid fixation can be achieved by locking with proximal and distal interlocking screws [4]. In addition, IM nails function as load-sharing devices that allow immediate weight-bearing and early mobilization, critical factors in maintaining quality of life for patients with limited life expectancy. The technique permits treatment through relatively small incisions with reduced operative time and blood loss compared to extensive plate fixation or prosthetic reconstruction. The biomechanical superiority of IM implants in pathological bone has been well-established, with studies demonstrating superior load distribution along the mechanical axis of bone and reduced stress concentration compared to extramedullary fixation. The goal of surgery is to obtain a rigid mechanical construct, which allows for early mobility and weight bearing [5]. Despite the established benefits of IM fixation, the optimal techniques, indications, and outcomes in various clinical scenarios require continued investigation. The heterogeneous nature of pathological fractures, varying tumor biology, different anatomical locations, and diverse patient populations necessitates comprehensive analysis of treatment outcomes to guide clinical decision-making and optimize patient care.
Case 1
A 70-year-old male with left subtrochanteric fracture of the femur.
Presentation
A 70-year-old male presented with an inability to bear weight for 2 days. He reported a 30-day history of progressive pain and swelling around the left hip. Two days prior, he sustained a trivial fall in the bathroom, resulting in sudden exacerbation of hip pain. His medical history was significant for diffuse large B-cell lymphoma.
On examination, the left lower limb was externally rotated and shortened. There was marked tenderness over the left hip and thigh, without open wounds or neurovascular deficits.
Investigations
Plain radiographs of the pelvis and femur (anteroposterior and lateral views) demonstrated a subtrochanteric, lytic lesion confined within the cortex of the left femur (Fig. 1). The contralateral femur appeared normal. Magnetic resonance imaging confirmed a pathological subtrochanteric fracture secondary to lymphoma (Fig. 2).

Figure 1 : Anteroposterior (AP) and lateral radiographs of the pelvis and left femur demonstrating a subtrochanteric lytic lesion confined within the cortex of the left femur (70-year-old male with large B-cell lymphoma). The subtrochanteric location and lytic appearance are characteristic of pathological fracture secondary to lymphoma.
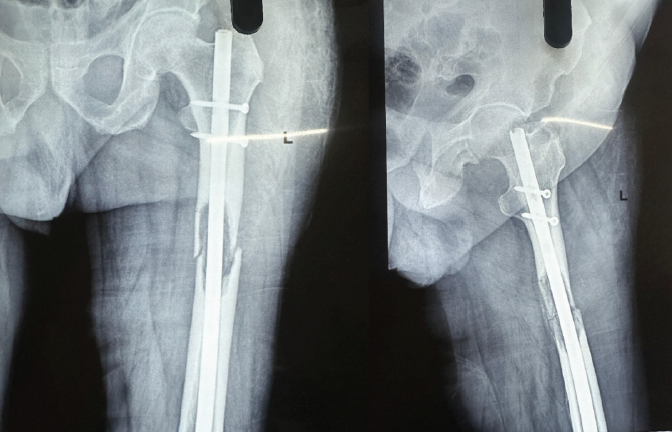
Figure 2 : Postoperative anteroposterior (AP) and lateral radiographs of the left femur following intramedullary nailing with long femoral nail and proximal interlocking screws. The radiographs demonstrate acceptable fracture reduction and proper implant positioning. The locked intramedullary nail provides rigid fixation spanning the pathological lesion, allowing early weight-bearing and mobilization.
Intervention
As the patient was elderly, needed early mobilization, and had a displaced pathological subtrochanteric fracture, we planned for surgical management with IM nailing. The patient was operated under spinal anaesthesia, using traction table in the supine position. Incision of around 5 cm was taken from the greater trochanter extending proximally. The entry point was made over the tip of the greater trochanter after dissecting the soft tissues. The guide was passed in the center of the medullary canal till the distal femur, gradual progressive reaming was done using flexible reamers. Interlocking femoral nail was inserted with proximal and distal locking. The intraoperative sample was taken from the medullary cavity and was sent for histopathological examination. The wound was closed in layers. The post-operative X-ray (Fig. 3) showed acceptable fracture reduction, and the patient was mobilized off the bed from the 2nd post-operative day with partial weight-bearing. Postoperatively patient was given 5 mg Zoledronic acid intravenously along with antibiotics and analgesics.

Figure 3 : Anteroposterior (AP) and lateral radiographs of the left hip and femur demonstrating left subtrochanteric lytic lesion confined within the cortex (60-year-old male with hepatocellular carcinoma metastasis). The lytic appearance and location are consistent with metastatic bone disease from primary hepatocellular carcinoma.
Histopathological examination confirmed the diagnosis of diffuse B-cell lymphoma.
Outcome
Full weight-bearing was started at 6 weeks. Patient was able to weight bear initially with crutches, latter he started walking independently by 6 months with no pain.
At present 1-year follow-up, the patient is comfortable with no pain and difficulty in walking and having good hip and knee range of motion. We are still following up the patient regularly to check for implant failure and refracture.
Case 2
A 60-year-old male with a left subtrochanteric fracture of femur.
Presentation
A 60-year-old male patient came with a complaint of pain in the left hip and inability to walk. The patient was previously diagnosed with hepatocellular carcinoma. On examination, tenderness was present at the left hip and thigh region, the left lower limb was externally rotated, shortened, with no wound and distal neurovascular deficit.
Investigations
Plain radiographs of the left hip with femur anteroposterior and lateral views revealed a left subtrochanteric lytic lesion confined within the cortex (Fig. 4).
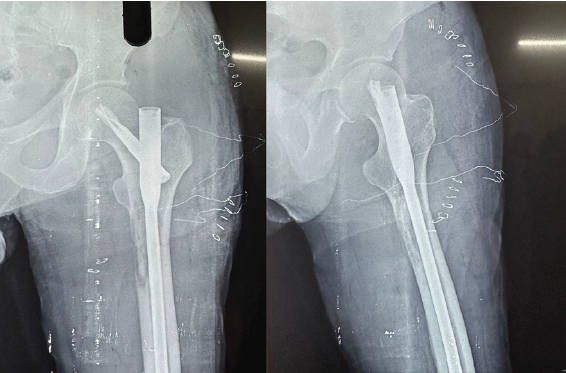
Figure 4 : Postoperative anteroposterior (AP) and lateral radiographs of the left femur following intramedullary fixation with PFNA2 (Proximal Femoral Nail Antirotation 2). The radiographs show acceptable fracture reduction with proper implant positioning and interlocking. The PFNA2 provides biomechanical stability across the pathological lesion site.
Intervention
We planned surgical management with Proximal Femoral Nail Antirotation Asia II (PFNA2). The intraoperative sample was taken from the medullary cavity and was sent for histopathological examination. The post-operative X-ray (Fig. 2) showed acceptable fracture reduction, and the patient was mobilized off the bed from the 1st post-operative day with partial weight-bearing. Histopathological examination confirmed the diagnosis metastasis secondary to hepatocellular carcinoma. Patient was given 5 mg i/v zolendronic acid along with analgesics and antibiotics.
Outcome
At present 1-year follow-up, the patient has no pain and difficulty in walking and having good hip and knee range of motion.
Case 3
A 89-year-old male with a fracture left shaft of humerus.
Presentation
A 89-year-old male patient was referred from the oncology outpatient department (OPD) to orthopedics OPD with complaint of pain in the left shoulder. The patient was a known case of chronic myeloid leukemia and was on chemotherapy for 2 years.
Investigations
Plain radiograph of the left arm showed lytic lesion of the proximal shaft humerus (Fig. 5). Skeletal survey of the patient revealed multiple lytic lesions over the skull characteristic for multiple myeloma (MM). On further workup, Myeloma profile revealed a serum Calcium – of 7.7 mg/dL, serum beta-2 microglobulin – above 20,000 ng/mL, M band on serum protein electrophoresis.

Figure 5 : Plain radiograph of the left arm showing lytic lesion of the proximal shaft of humerus (89-year-old male with multiple myeloma). Skeletal survey revealed multiple lytic lesions over the skull characteristic of multiple myeloma involvement. The proximal humeral shaft location is the second most common site for long bone metastases and pathological fractures.
Intervention
Patient was managed with closed reduction and internal fixation using IM humerus nailing (Fig. 6) along with biopsy.
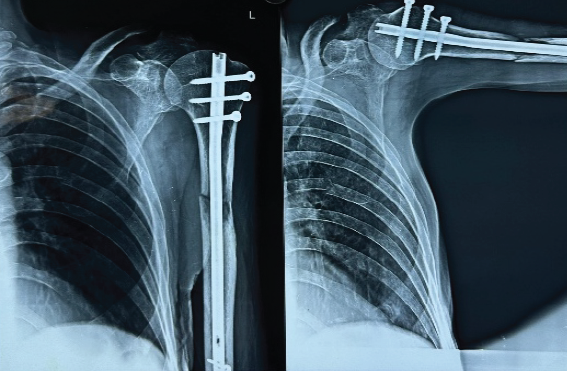
Figure 6 : Postoperative radiograph of the left humerus following closed reduction and internal fixation using intramedullary humerus nailing. The intramedullary nail provides stable fixation through the lytic lesion, allowing early mobilization and rehabilitation despite the patient’s advanced age (89 years) and systemic disease burden.
Histopathological examination revealed typical plasma cells consistent with the diagnosis of MM. Patient was given 5 mg zolendronate i/v along with chemotherapy, namely, VrD regimen (Ortezomib, lenalidomide, and dexamethasone).
Outcome
- The patient’s function recovered, and his pain was rapidly relieved.
- On 9 month follow-up patient had adequate range of motion without pain.
Case 4
A 57-year-old female with fracture left distal shaft femur.
Presentation
A 57-year-old female patient with an inability to bear weight for the past 12 days. She was a known case of breast carcinoma from the past 2 years.
Investigations
Radiograph of the left thigh revealed an extra-articular distal femur fracture.
Intervention
The patient was managed with interlocking distal femur nailing along with biopsy. Biopsy revealed metastasis secondary to medullary breast cancer. Partial weight bearing was started on post-operative day 1. Patient was given 5 g i/v zoledronate along with chemotherapy, analgesics, and antibiotics.
Outcome
Post-operative follow-up at 1 year revealed good knee range of motion and pain relief.
Case 5
A 55-year-old male with a right shaft of humerus fracture.
Presentation
A 55-year-old male with complaints of right arm and shoulder pain. The patient was known case of MM since 3 years. On examination, no external wound was present; tenderness was present on the right arm with no distal neurovascular deficit.
Investigation
Radiograph of right arm shows pathological fracture of right shaft of humerus (Fig. 7).

Figure 7 : Plain radiograph of the right arm showing pathological fracture of the right shaft of humerus (55-year-old male with multiple myeloma for 3 years). The lytic lesion at the humeral shaft demonstrates tumor involvement characteristic of multiple myeloma-related pathological fracture.
Intervention
Patient was managed with closed reduction and internal fixation using IM humerus nailing (Fig. 8) along with biopsy.

Figure 8 : Postoperative radiograph of the right humerus following closed reduction and internal fixation using intramedullary humerus nailing. The locked intramedullary nail secures the pathological fracture, enabling functional recovery and pain relief. The minimally invasive approach minimizes soft tissue trauma and operative morbidity.
Outcome
The patient is functionally recovered, and his pain settled.
Case 6
41-year-old female with a left proximal femur lytic lesion.
Presentation
A 41-year-old female with complaints of left hip and thigh pain. The patient was known case of Ca breast. On examination, no external wound was present; tenderness was present on the left thigh laterally with no distal neurovascular deficit.
Investigation
Radiograph of pelvis with both hips shows lytic lesion of the left proximal femur.
Intervention
Patient was managed with closed reduction and internal fixation using IM PFNA2 figure, along with biopsy.
Outcome
The patient is functionally recovered, and his pain settled. However, patient lost to follow-up after 3 months. Table 1.
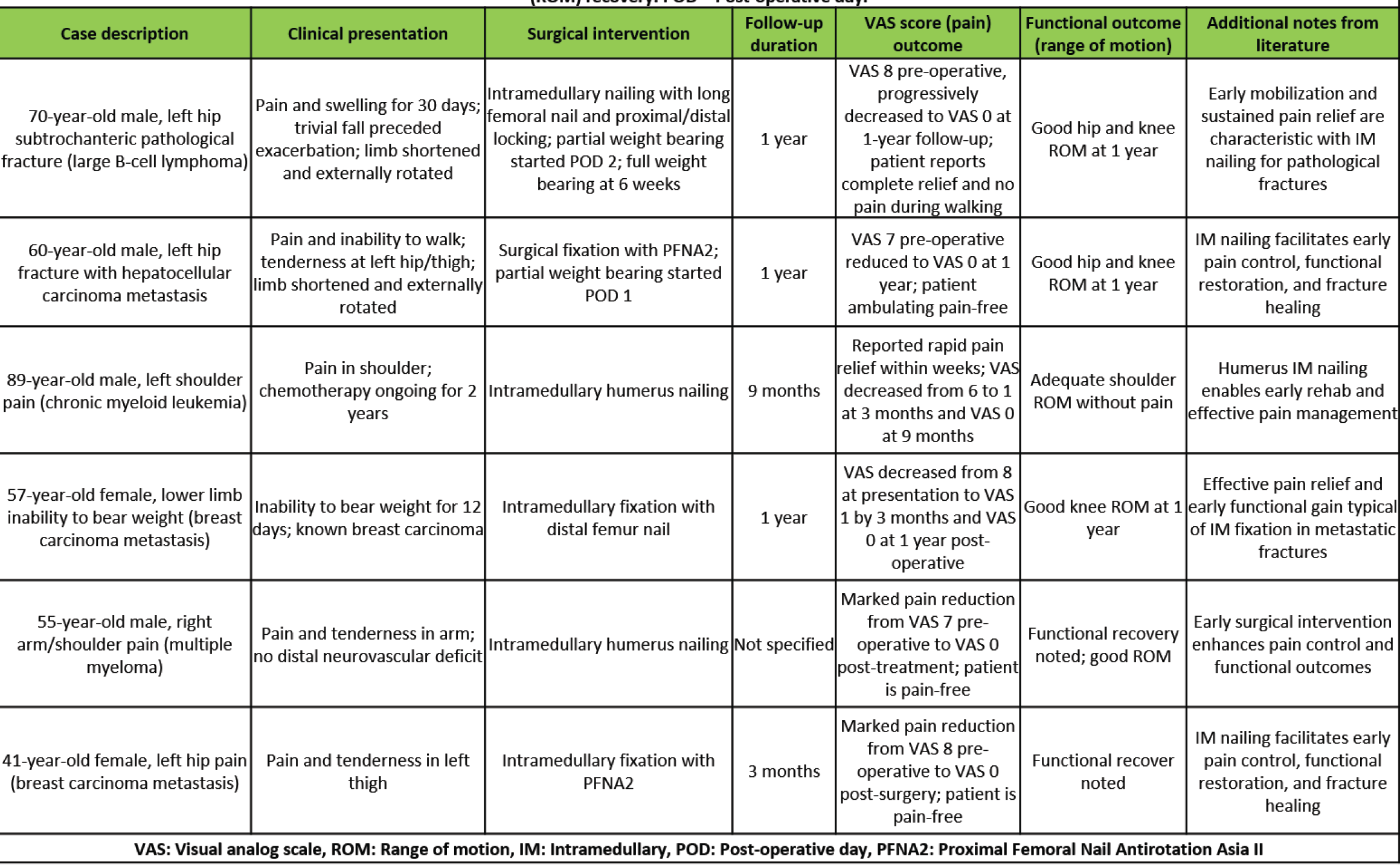
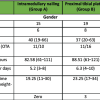
Table 1: This table presents a comprehensive clinical summary of all six cases managed with intramedullary fixation for pathological fractures. It demonstrates the VAS (Visual Analog Scale) pain scores, ranging from 0 (no pain) to 10 (worst pain), showing significant pain reduction across all cases. Functional outcomes are measured by range of motion (ROM) recovery. POD = Post-operative day.
Pathological fractures in long bones resulting from metastatic lesions, MM, and atypical femoral fractures represent considerable surgical challenges due to compromised bone quality, patient systemic disease burden, and the need for durable fixation that supports early mobilization. IM nailing has emerged as a preferred method for stabilizing such fractures because it provides biomechanical advantages through load sharing along the entire bone shaft and allows spanning of existing and impending lesions, thereby reducing the risk of subsequent fractures. This feature is particularly beneficial in MBD where multifocal involvement is common. Orthopedic surgeons, when performing Intramedullary IM fixation for these fractures, should be prepared to utilize accessory equipment and should adopt creative techniques for reduction and fixation [6]. IM nailing is considered the treatment of choice for both complete and incomplete atypical fractures, as it provides stable fixation and allows early weight-bearing. Prophylactic nailing for incomplete fractures reduces progression to complete fracture and associated morbidity. Less invasive procedure with less blood loss and shorter hospital stays also benefits patients [7]. Literature reports consistently show satisfactory union rates and functional improvement following IM fixation in atypical femur fractures. Functional outcomes in patients undergoing IM fixation for pathological fractures have been reported to improve significantly, as measured by tools such as the musculoskeletal tumor society scoring system. Early pain relief and return to function enable patients to proceed with systemic oncologic therapies and improve quality of life. Pathological fracture of the femur seriously deteriorates the quality of life of cancer patients: most of these fractures require surgery with a solid and durable system of fixation to achieve pain control and early restoration of full weight-bearing, regardless of the patient’s predicted life span [8]. Humerus is the second most common site for long bone metastases following femur. Although humerus is not the weight-bearing bone pathological fractures of the humerus severely restrict the use of the involved arm and hand, and surgical stabilization of symptomatic impending, or pathological fractures. Stabilization with IM nailing for pathological fractures of the humeral diaphysis has the advantage of a small incision, less soft-tissue dissection, short operative time, and early rehabilitation [9]. Early surgery should be performed for the fracture of the proximal humerus caused by MM [10]. While intraoperative and post-operative complications remain a concern, proper implant selection, careful surgical technique, and multidisciplinary perioperative care can mitigate risks effectively. This series further highlights the importance of individualized surgical planning integrating patient prognosis, lesion characteristics, and multidisciplinary oncologic treatment strategies to optimize implant choice and rehabilitation protocols. Ongoing advancements in implant design, surgical technique, and adjuvant therapies hold promise for improving outcomes in this complex patient population. Complication rates were low, with no implant failures or infections in this small series. Integration of systemic oncological therapies with surgical management is essential for optimizing patient outcomes.
IM nailing is a dependable and effective modality for the treatment of pathological fractures of long bones arising from metastatic disease, MM. It offers biomechanical advantages that enable early mobilization, rapid pain relief, and significant functional recovery. Prophylactic and definitive nailing for atypical femoral fractures associated with long-term antiresorptive therapy prevents fracture progression and promotes reliable healing. Individualized surgical planning, incorporating lesion characteristics, patient prognosis, and systemic oncologic treatment, remains essential to optimizing outcomes. This case series reinforces the role of IM fixation as a cornerstone of orthopedic management in pathological fractures, contributing valuable insights to operational strategies and patient care in a complex clinical setting. IM nailing is an effective and biomechanically sound treatment for pathological long bone fractures, offering pain relief, early mobilization, and improved quality of life through individualized surgical planning.
A lytic lesion in the diaphysis of a long bone presenting with a pathological fracture managed by IM nailing is consistent with the current best practices. IM nailing offers mechanical stability, pain relief, and facilitate early mobilization, particularly for mid-shaft lesions and patients with limited prognosis. Long-term outcomes are satisfactory, but late complications such as mechanical failure may occur. Consideration of adjunct therapies such as cement augmentation and radiotherapy is appropriate based on individual patient factors and oncologic prognosis.
References
- 1. Arpornsuksant P, Morris CD, Forsberg JA, Levin AS. What factors are associated with local metastatic lesion progression after intramedullary nail stabilization? Clin Orthop Relat Res 2022;480:932-45. [Google Scholar] [PubMed]
- 2. DiCaprio MR, Murtaza H, Palmer B, Evangelist M. Narrative review of the epidemiology, economic burden, and societal impact of metastatic bone disease. Ann Jt 2022;7:28. [Google Scholar] [PubMed]
- 3. Ormsby NM, Leong WY, Wong W, Hughes HE, Swaminathan V. The current status of prophylactic femoral intramedullary nailing for metastatic cancer. Ecancermedicalscience 2016;10:698. [Google Scholar] [PubMed]
- 4. Willeumier JJ, Van Der Linden YM, Van De Sande MA, Dijkstra PD. Treatment of pathological fractures of the long bones. EFORT Open Rev 2016;1:136-45. [Google Scholar] [PubMed]
- 5. Scolaro JA, Lackman RD. Surgical management of metastatic long bone fractures: Principles and techniques. J Am Acad Orthop Surg 2014;22:90-100. [Google Scholar] [PubMed]
- 6. Klahs KJ, Heh E, Yousaf M, Tadlock J, Thabet AM. Operative challenges of intramedullary nailing for subtrochanteric blastic pathological femur fracture: A case report. J Surg Case Rep 2023;2023:rjac630. [Google Scholar] [PubMed]
- 7. Wu K, Lin T, Lee CH. Intramedullary nailing versus cemented plate for treating metastatic pathological fracture of the proximal humerus: a comparison study and literature review. J Orthop Traumatol. 2023 Aug 24;24(1):45. doi: 10.1186/s10195-023-00721-7. PMID: 37620629; PMCID: PMC10449752. [Google Scholar] [PubMed] [CrossRef]
- 8. Piccioli A, Rossi B, Scaramuzzo L, Spinelli MS, Yang Z, Maccauro G. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014;45:412-7. [Google Scholar] [PubMed]
- 9. Choi ES, Han I, Cho HS, Park IW, Park JW, Kim HS. Intramedullary nailing for pathological fractures of the proximal humerus. Clin Orthop Surg 2016;8:458-64. [Google Scholar] [PubMed]
- 10. Xu GQ, Wang G, Bai XD, Wang XJ. Intramedullary nailing for pathological fractures of the proximal humerus caused by multiple myeloma: A case report and review of literature. World J Clin Cases 2022;10:3518-26. [Google Scholar] [PubMed]