CMC fracture dislocations are a rare hand injury that are at risk of being missed on initial presentation and imaging, but can be safely treated with bridge plating with optimal functional and patient-reported outcomes, even with a subacute presentation with concern for devitalized bone.
Miss Taylor Coates, Western University of Health Sciences of the Pacific-Northwest, 200 Mullins Dr, Lebanon - 97355, Oregon, USA. E-mail: taylor.coates@westernu.edu
Introduction: Fracture dislocations of the second and third carpometacarpal (CMC) joints are a rare injury, often associated with high-energy trauma that can lead to significantly compromised hand function if missed.
Case Report: A 23-year-old female presented with a subacute right second and third CMC fracture dislocations after a rollover ATV accident. Open reduction and fixation of the second and third CMC fracture dislocations with a bridge plating construct was performed. At 12 weeks postoperatively, there were no complaints of pain. Hardware was removed at 5 months postoperatively. One year postoperatively, the patient had no significant stiffness, pain, or functional deficits.
Conclusion: Despite the subacute presentation and concern for devitalized bone, repair of the second and third CMC base fracture dislocations with bridge plating is a safe option for the CMC joints without fusion with good results.
Keywords: Carpometacarpal fracture-dislocation, orthopedics, bridge plating, hand injury.
Carpometacarpal (CMC) joint injuries are uncommon and encompass 0.2–1% of all hand injuries, often occurring due to high-energy trauma [1]. Injury mechanisms often involve axial loading and hyperextension of the wrist, such as with a motor vehicle accident or a fall [2]. Clinically, patients present with notable swelling, deformity, and loss of function of the hand and wrist [3,4]. This injury pattern can be a challenge to diagnose and may be missed on initial radiographs, with further characterization often needed using advanced imaging such as computed tomography (CT) [2,5]. In this report, we present a case of CMC fracture dislocations to the second and third metacarpal bases, with associated fourth metacarpal base and capitate fractures and a displaced ulna shaft fracture, successfully treated with surgical fixation of the second and third CMC fracture dislocations and capitate with bridge plating of the CMC joints. This case report aims to highlight this rare injury and propose bridge plating as a safe option for the CMC joint fracture dislocations without fusion despite the subacute presentation and concern for devitalized bone.
History of presenting illness
The patient was a 23-year-old right-hand dominant female preschool teacher who sustained a crush injury to the right hand and arm when she was riding in an ATV that rolled over. She was seen at a local trauma center and discharged in a splint. The patient presented to the clinic 3 weeks post-injury with complaints of numbness and tingling in the radial digits and diffuse swelling of the hand. Radiographs and a CT scan of the right hand were performed, which demonstrated right second and third CMC fracture dislocations, right fourth metacarpal base and capitate fractures, and a right displaced ulna shaft fracture (Fig. 1 and 2). There was also concern for acute carpal tunnel syndrome due to the numbness in the radial digits. Surgery was recommended for fixation of the second and third metacarpal fracture dislocations and capitate, as well as carpal tunnel release.

Figure 1: Pre-operative radiographs of the right hand in splint (a) oblique view, (b) lateral view, and (c) posteroanterior view. X-rays show second and third carpometacarpal base fracture dislocations, fourth metacarpal base and capitate fractures, and displaced ulna shaft fracture.
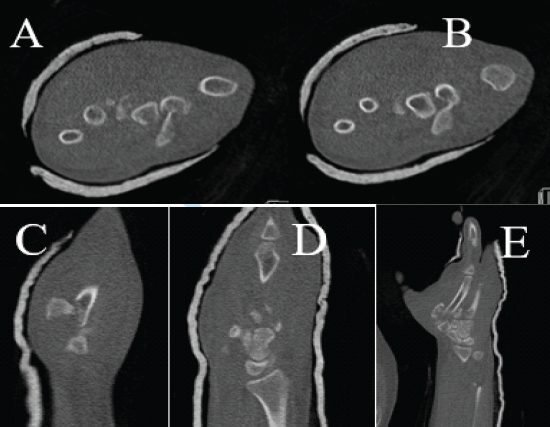
Figure 2: Pre-operative CT of the right hand in splint. (a, b, c, d, e) CT shows second and third carpometacarpal base fracture dislocations, fourth metacarpal base and capitate fractures, and displaced ulna shaft fracture.
Surgical technique
A dorsal longitudinal incision was made centered over the right third metacarpal. The extensor tendons were protected, and the fracture fragments were identified. A fragment of the fourth metacarpal base articular surface was found rotated and located distal and radial to the capitate. The second and third metacarpal shafts were significantly displaced. The distal second metacarpal shaft was identified in the first webspace. Given the delayed presentation, there was significant shortening and some early callus formation. Ten pounds of traction were utilized through finger traps to help reduce the second and third metacarpals. After the metacarpals were well-aligned, the third metacarpal base articular surface was reduced but a significant piece was found to still be missing from the second metacarpal base. This fracture fragment was located deep within the palm adjacent to the flexor tendons. It had minimal soft-tissue attachment intact and contained about 70% of the second metacarpal articular surface. Although this bone fragment was possibly devitalized, the operating surgeon attempted to salvage the bone, given the large portion of the articular surface it contained. The bone fragment was secured to the second metacarpal shaft and trapezoid with a 0.045 Kirschner wire (K-wire). The third metacarpal was then provisionally fixed with another 0.045 K-wire. Due to the instability and subacute nature of the injury, two 2.4 mm LC-DCP (Synthes Inc, West Chester, PA) were contoured and secured in a bridge plating construct across the second and third CMC joints. This construct also stabilized the capitate fracture. The provisional K-wires were removed, and the second, third, and fourth metacarpal fractures were stable and well-reduced with appropriate passive range of motion of the fingers. The fourth metacarpal did not require fixation. A carpal tunnel release and ulnar shaft fixation were then performed. Postoperatively, the patient was placed in a volar splint and allowed immediate finger range of motion.
Post-operative course
Two weeks postoperatively, the patient’s numbness was improving; she was transitioned to a removable orthosis and was started in hand therapy (Fig. 3). Six weeks postoperatively, the patient was allowed to begin light use and aggressive passive range of motion. At 12 weeks postoperatively, radiographs demonstrated healing of the fractures and no recurrent dislocations (Fig. 4). The patient had no complaints of pain and was using her hand for activities of daily living. There was significant stiffness in the metacarpophalangeal (MCP) joints (index finger 0–25°, middle finger, ring finger, and small finger 0–45°) but a full range of motion in the interphalangeal joints. The patient was offered removal of hardware at this time, but elected to wait 2 months until her winter break. At 4 months postoperatively, the patient’s DASH score had improved from 83.33 preoperatively to 11.67 postoperatively.
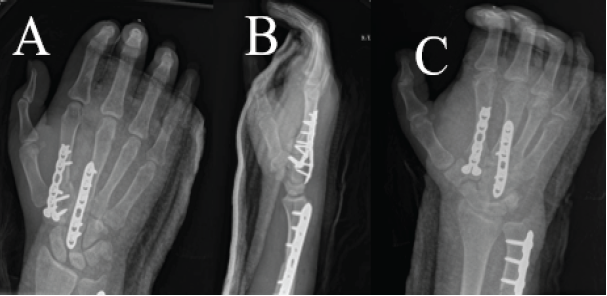
Figure 3: Two-week post-operative radiographs of the right hand in a volar splint. (a) Posteroanterior view, (b) lateral view, and (c) oblique view. X-rays show bridge plating of the second and third carpometacarpal base fracture dislocations with stabilization of the capitate fracture through the construct and fixation of ulna shaft fracture.
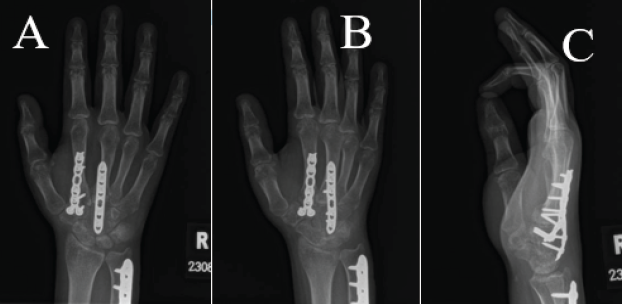
Figure 4: Three-month post-operative radiographs of the right hand. (a) Posteroanterior view, (b) oblique view, and (c) lateral view. X-rays show bridge plating of the second and third carpometacarpal base fracture dislocations and fixation of ulna shaft fracture.
At 5 months post-operation, the patient returned for hardware removal. At that time, the patient’s MCP joint motion had improved: Index finger flexion of 45°, and middle, ring, and small finger MCP joint flexion to 70°. Six weeks post-hardware removal, the patient’s motion had improved to 60° of flexion in the index finger, while MCP joint motion in the other fingers remained unchanged (Fig. 5). Wrist range of motion was 45° flexion and 50° extension. Three months post-hardware removal, the patient was doing well and using her hand normally (Fig. 6). Final DASH score at 1 year postoperatively was 2.5.

Figure 5: Six weeks status post removal of hardware of the right hand.
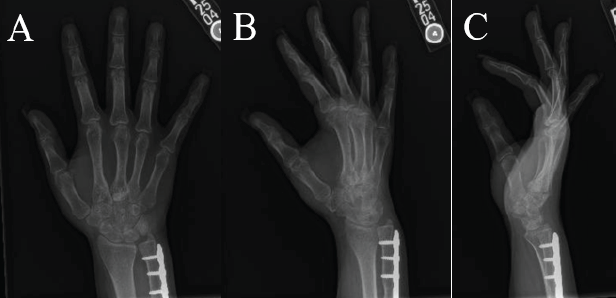
Figure 6: Three months status post removal of hardware radiographs of the right hand. (a) posteroanterior view, (b) oblique view, (c) lateral view. X-rays show appropriate healing post removal of bridge plating of the second and third metacarpals with fixation of ulna shaft fracture.
CMC fracture dislocation of the second and third metacarpals is a rare injury resulting from high-energy trauma that often requires surgical fixation to treat [6]. While fracture-dislocation at the base of the first metacarpal (Bennett fracture-dislocation) is well-recognized as the most common metacarpal fracture-dislocation injury pattern, second and third metacarpal base fracture dislocations with associated capitate fractures are less commonly reported [7,8]. Dorji and Thrinley reported a similar rare case of missed fracture-dislocation of the second and third CMC joints initially misdiagnosed as a blunt trauma to the hand, but that was successfully treated with open reduction and percutaneous pinning with K-wires [9]. In the setting of possible devitalized bone or extensive comminution of the articular surface, bridge plating helps restore the alignment of the joint while minimizing disruption to the soft tissues and bloody supply. It also provides greater stability than K-wires to allow more aggressive early range of motion, which can be particularly helpful in the setting of polytrauma. This case report demonstrates that it is a safe and effective alternative to K-wires or joint fusion. Given the rarity of intra-articular fractures of the second through fifth metacarpal bases, there is no consensus regarding gold standard treatment for these injuries, and management depends on fracture injury pattern and patient presentation [12]. Non-operative management includes closed reduction and immobilization. However, unstable fractures involving dislocation often require internal fixation [1]. Concerning second metacarpal base fractures, a review by Bushnell et al. documented 13 case reports encompassing 15 patients from 1979 to 2001, with nine patients treated surgically and five non-operatively [12,13]. Cases treated with surgery had favorable outcomes, and this approach is preferred more so to restore the function of the extensor carpi radialis brevis muscle than to restore joint congruity, given the minimal motion of the second CMC joint. Third metacarpal base fractures are rare, but surgical treatment is favored to restore musculotendinous function [13]. In this case, surgical fixation with bridge plating was a viable option to avoid arthrodesis of the CMC joints. Despite the concern for devitalized bone and the subacute nature of presentation of the injury, this case showed excellent functional results at 1-year follow-up.
CMC fracture dislocations are a rare injury that may be missed based on initial clinical presentation and imaging, but are important to recognize given the potential for long-term functional deficits. To date, no research has presented a case of second and third metacarpal base fracture dislocations treated with open reduction and bridge plating construct. This case report highlights a rare injury and supports bridge plating as a safe treatment alternative for CMC fracture dislocations with good functional outcomes, even in a subacute setting with concern of devitalized bone.
Open reduction with bridge plating provides a safe and effective treatment option for subacute presentations of rare CMC fracture dislocations, offering preservation of joint function and avoiding the need for CMC fusion.







