Early, well-planned single-stage reconstruction tailored to individual injury patterns leads to excellent functional recovery and outcomes in multi-ligamentous knee injuries.
Dr. Abhishek Vaish, Department of Orthopedics, Indraprastha Apollo Hospitals, New Delhi, India. E-mail: drabhishekvaish@gmail.com
Background and Aims: Multiligamentous knee injuries (MLKIs) are uncommon yet complex, presenting challenges in diagnosis, treatment, and rehabilitation. This study aims to evaluate the incidence, causes, surgical techniques, and functional outcomes of MLKI cases in Indian patients.
Materials and Methods: A prospective study was conducted at a tertiary care center. Patients underwent surgical intervention based on clinical evaluation, employing both single-stage and staged reconstruction strategies. The sequence of ligament repair and graft selection was tailored to each case. Post-operative outcomes were assessed using the knee society score (KSS) and Lysholm score.
Results: 70 MLKI cases were treated between January 2021 and July 2023, with two patients lost to follow-up, all patients had anterior cruciate ligament injuries, with additional ligament involvement observed in posterior cruciate ligament (24%), medial collateral ligament (32%), and posterolateral corner (27%). Meniscal injuries were noted in 40% of cases. Graft selection included semitendinosus and gracilis tendons (54%) and peroneus longus (46%), with an average graft diameter of 8 ± 1 mm. No significant differences in outcomes were found between graft types (P > 0.05). At 6 months post-surgery, the mean KSS improved from 51 ± 10 to 80 ± 5, while Lysholm scores increased from 60 ± 10 to over 80. Notably, 90% of patients achieved excellent results.
Conclusion: Early, well-planned single-stage reconstruction emerges as an effective strategy for managing MLKIs, yielding favorable functional outcomes. Tailoring surgical approaches based on individual injury profiles significantly optimizes recovery.
Keywords: Knee injuries, multi-ligamentous injuries, anterior cruciate ligament, surgical procedures, operative, rehabilitation.
The knee joint, a complex synovial hinge, is stabilized by several intra- and extra-capsular ligaments, including the anterior cruciate ligament (ACL), the posterior cruciate ligament (PCL), the medial collateral ligament (MCL), and the lateral collateral ligament (LCL). Multiligamentous knee injuries (MLKIs), which involve the disruption of two or more of these stabilizing structures, represent severe forms of knee trauma. These injuries are most commonly the result of high-energy trauma, such as road traffic accidents (RTAs), falls from height, or contact sports injuries [1,2,3]. Despite their rarity – estimated globally at 0.072/100,000 person-years – their functional and surgical complexity is significant [1]. MLKIs pose substantial challenges in diagnosis, surgical planning, and post-operative rehabilitation. There remains an ongoing debate regarding the optimal treatment timing (early vs. delayed), surgical strategy (single-stage vs. staged reconstruction), order of ligament repair, and the ideal graft choice [4,5,6,7]. Furthermore, the heterogeneity of injury patterns complicates the establishment of standardized treatment protocols [8]. Although recent literature supports early surgical intervention for better outcomes, there remains a limited consensus on surgical sequencing and graft selection tailored to specific injury combinations [6,9]. Functional outcomes following MLKI surgery are also variable. While tools, such as the knee society score (KSS) and Lysholm score are widely used to assess post-operative success, long-term data across diverse populations remain sparse [10]. Moreover, existing studies are often retrospective or limited by small sample sizes, highlighting a need for prospective research. This single-center prospective study aims to close the gaps pertaining to surgical approaches and functional outcomes of MLKI cases. The study focuses on decision-making in treatment sequencing and graft selection, comparing outcomes with those reported in the present literature and aiming to provide evidence to inform future clinical best practices.
This was a prospective interventional study conducted in the Department of Orthopedics at a tertiary care center between January 2021 and July 2023. Sample size was decided based on statistical Cochran’s formula to power the study.
- n = the required sample size
- Z = the z-value (or Zα/2), which is a constant from the standard normal distribution corresponding to the desired confidence level (e.g., 1.96 for a 95% confidence level, which is standard)
- p = the expected proportion of the attribute in the population (obtained from previous studies or a pilot study; if unknown, 0.5 is often used as it yields the largest sample size)
- d = the desired precision or margin of error (e.g., 0.05 for a ±5% margin of error).
Ethical approval was obtained from the institutional review board. Patients aged 18–60 years with clinical and radiological evidence of MLKI (defined as injury to two or more ligaments, including the ACL, PCL, MCL, LCL or posterolateral corner (PLC) were included. Exclusion criteria were open knee injuries, isolated meniscal tears without ligament injury, or patients unwilling to consent. Pre-operative assessment included detailed history taking, physical examination using standard tests (Lachman, anterior/posterior drawer, varus/valgus stress, dial test), magnetic resonance imaging (MRI), and stress radiographs. Surgery was planned based on clinical findings and confirmed by MRI. All patients underwent arthroscopic or combined open-assisted single-stage reconstruction, depending on the structures involved. ACL and PCL reconstructions were done arthroscopically. MCL or PLC injuries requiring surgical management were addressed using open techniques. Grafts used included ipsilateral semitendinosus-gracilis (STG) autografts or peroneus longus (PL) autografts when hamstring quality was poor. Graft fixation methods included suspensory (cortical button) and aperture (interference screw) devices. Post-operatively, patients were placed in hinged knee braces. Weight-bearing was allowed as tolerated from day 2 with the brace locked in extension. Gradual range-of-motion exercises began within the 1st week after surgery. Standardized rehabilitation protocols were followed.
Patients were assessed at 6 weeks, 12 weeks, and 6 months using the KSS and Lysholm score.
The KSS system [33] is divided into two primary components – the knee score and the functional score, each with a maximum of 100 points, giving a total possible score of 200.
- The knee score (0–100 points) evaluates pain (50 points), range of motion (25 points), and stability (25 points), with deductions for deformities, such as flexion contracture, extension lag, or misalignment.
- The functional score (0–100 points) assesses the patient’s ability to walk and climb stairs (50 points each), with deductions for the use of walking aids, such as canes or crutches.
Scores are typically interpreted as follows: 85–100 points indicate excellent results, 70–84 good, 60–69 fair, and below 60 poor. This structured scoring system provides a standardized and objective method to quantify both clinical and functional outcomes after knee surgeries, including ligament reconstruction. The Lysholm KSS [34] is a patient-reported outcome measure (PROM) widely used to assess knee function, particularly following ligamentous injuries and reconstructive surgeries. It consists of eight parameters – limp, support, locking, instability, pain, swelling, stair climbing, and squatting – with a total score of 100 points. Higher scores indicate better knee function and stability. Based on the total score, results are graded as excellent (95–100), good (84–94), fair (65–83), and poor (<65). The Lysholm score provides a simple yet comprehensive assessment of a patient’s functional recovery and subjective satisfaction after treatment. Complications were recorded and divided into major (recurrent or residual instability, deep infection) and minor (superficial infection).
Seventy patients were included. Two patients were lost to follow-up. The mean age was 30.1 ± 8.4 years (range, 18–58 years). with 85% of the participants being male. The predominant mode of injury was RTAs (80%), followed by sports injuries (15%) and falls (5%). Right-sided injuries were more frequent (58%). The average time between injury and surgery was 8.25 ± 5 weeks. Chronic injuries (>6 months duration) were seen in 12 patients, all of whom exhibited thigh muscle wasting. ACL injuries were present in all patients. PCL involvement was noted in 16 (24%), MCL in 22 (32%), and PLC in 18 (27%). LCL injuries occurred in 12 patients (17%) (Fig. 1). Meniscal injuries were observed in 40% of cases, with medial meniscus involvement being more common.
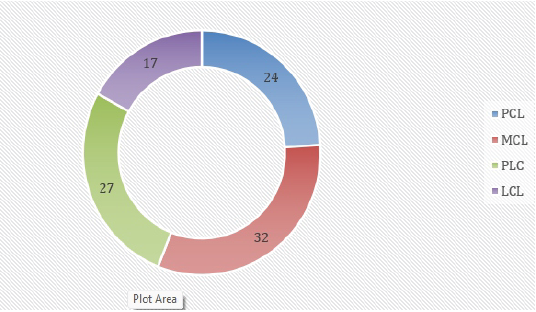
Figure 1: Pattern and percentage incidence of associated injuries.
The tendon grafts used included STG in 54% and PL in 46%. The average graft diameter was 8 ± 1 mm. No significant difference in outcome was observed between graft types or fixation methods (P > 0.05). Clinical assessments revealed that the Lachman test was positive in 89% and the anterior drawer test in 86% of cases pre-operatively. MRI could not detect ligament injuries in six patients who had positive clinical test results, underscoring the importance of thorough examination. At 6 months, the mean KSS improved from 51 ± 10 to 80 ± 5. Lysholm scores improved from 60 ± 10 to over 80. Sixty-three patients (90%) had excellent results; seven had good outcomes. Two patients developed superficial infections (resolved with antibiotics), and one required revision for instability.
MLKIs are relatively rare injuries but clinically significant due to their complexity, potential for long-term instability, and high functional demands from an often young, active patient population. The incidence in our series mirrors recent epidemiological data from Westermann et al. [1] and Lindsey et al. [3], with young adult males predominating and RTAs accounting for the majority of cases. This injury pattern is particularly relevant in low- and middle-income countries (LMICs), where the increasing use of high-speed vehicles has been associated with a rise in MLKI incidence [23]. Public health interventions, including road safety campaigns and the adoption of protective sports equipment, remain crucial in preventing these serious knee injuries. Accurate diagnosis of MLKIs requires a combination of thorough clinical evaluation and imaging. While MRI is an invaluable tool, our data, similar to Al Mohammad et al. [2] and Fischenich et al. [12] – show that it may fail to identify certain ligament injuries, particularly in chronic or partially healed cases (Table 1). This underscores the continued importance of validated clinical tests, such as Lachman, posterior drawer, and dial tests. Scoping reviews [23] recommend that in resource-limited settings, clinical diagnosis should be prioritized when imaging is inconclusive or unavailable.
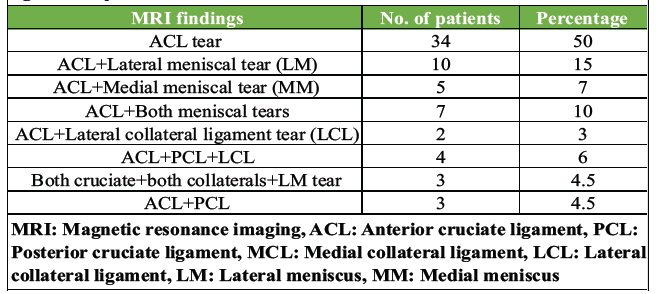
Table 1: MRI findings after the injury, showing the combination of knee ligament injuries
The optimal timing for surgery remains a subject of ongoing debate. Our findings are consistent with those of Harner et al. [6] and Mook et al. [19], as well as the recent meta-analysis by Vaishya et al. [24,32], support early reconstruction – ideally within 3 weeks – to facilitate graft placement and reduce arthrofibrosis risk. However, in cases with severe soft tissue compromise or delayed presentation, often seen in rural LMIC contexts, delayed surgery may be unavoidable. Yoon et al. [8] highlights that while delayed intervention can still yield acceptable results, early timing is associated with faster neuromuscular recovery. In our cohort, single-stage reconstruction yielded excellent functional outcomes without increasing complication rates, aligning with the findings of Ishibashi et al. [5] and Joutoku et al. [4]. Recent systematic reviews [26,29] indicate that single-stage procedures reduce hospital stay, rehabilitation time, and costs – critical advantages in LMIC settings. Staged approaches remain indicated for cases with severe swelling, vascular repair, or open injuries [14,16], but their higher rehabilitation demands and resource implications make them less feasible in many environments. Graft selection remains a critical factor in MLKI reconstruction. The STG autografts were our primary choice; PL autografts were used when the quality of the hamstring was found to be suboptimal, a finding also supported by Goyal et al. [10]. Moreover, a recent systematic review [31] demonstrates comparable biomechanical strength and functional outcomes. Our findings of no significant difference in outcomes between fixation methods are consistent with those of Crum et al. [11] and recent biomechanical analyses [25]. Graft choice should remain individualized, taking into account the patient’s anatomy, prior surgeries, and the availability of suitable grafts. We followed a medial or posterolateral repair-first strategy, followed by reconstruction of the PCL and ACL. Excellent clinical outcomes were seen with this approach (Fig. 2, 3, 4, 5). This sequence, supported by Kim et al. [9] and LaPrade et al. [18], restores coronal stability before addressing sagittal stability, minimizing graft tension imbalances. Literature suggests that sequencing errors can compromise biomechanical restoration [27], emphasizing the need for standardized, biomechanically informed protocols.
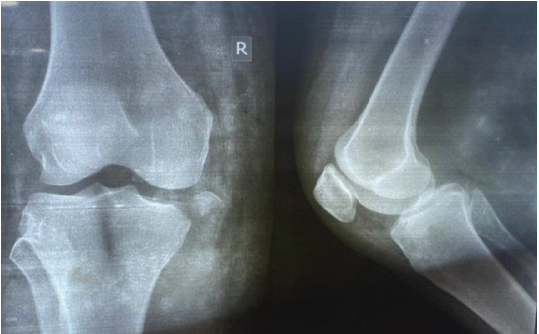
Figure 2: Anteroposterior and lateral view of radiograph of the knee showing medial condyle fracture with medial collateral ligament avulsion.

Figure 3: Post-operative anteroposterior and lateral view of radiograph of the knee showing medial condyle fracture fixed with cannulated cancellous screws in the distal femur and proximal tibia.

Figure 4: Patient attained full flexion and extension at 6 months post-operatively.

Figure 5: Patient performing squatting and sitting cross-legged at 6-months post-operatively.
Our accelerated rehabilitation program – with early passive mobilization and progressive weight-bearing – produced significant improvements in KSS (Table 2) and Lysholm scores (Table 3) at 6 months, consistent with global best practices [20,28]. Indian series [24,25] and recent rehabilitation-focused reviews [26] confirm that structured, multidisciplinary rehabilitation is essential for optimal outcomes, particularly to prevent stiffness. Notably, 90% of our patients achieved excellent results, exceeding the pooled return-to-function rates reported by King et al. [21].
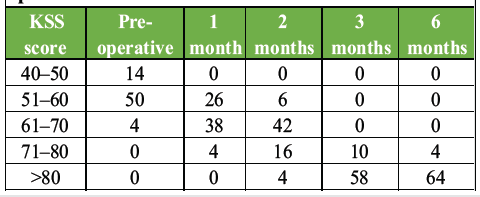
Table 2: Knee severity score (KSS) pre- and post-operative intervals
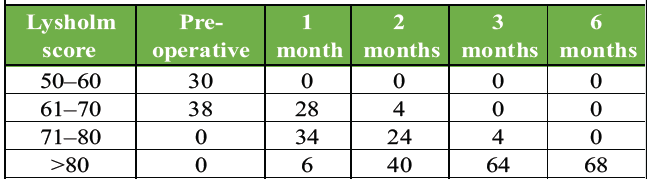
Table 3: Lysholm scores at pre- and post-operative intervals
Limitations of this study include its single-center design, relatively short follow-up, and absence of a control group. However, strengths include its prospective design, consistent surgical techniques, and uniform rehabilitation protocols. Future research should include multicentric randomized trials, longer follow-up to assess osteoarthritic progression, and incorporation of PROMs [23,29]. Technological advances, such as 3D gait analysis and imaging biomarkers could further refine the assessment of biomechanical restoration [27,30].
This study reinforces that early and well-planned single-stage reconstruction is a reliable and effective approach for managing MLKIs. By aligning surgical strategies with the specific injury pattern and patient profile, optimal stability and function of the knee can be restored. The findings highlight the importance of individualized surgical planning and graft selection in achieving favorable outcomes. Overall, a tailored, patient-centric approach to MLKI reconstruction fulfills the aim of improving knee function and long-term recovery, supporting its adoption as a preferred management strategy.
• Early diagnosis and timely surgical intervention are crucial for optimal recovery in MLKIs
• A single-stage, well-planned reconstruction provides excellent functional outcomes and reduces rehabilitation time
• Tailoring the surgical approach – including graft choice and repair sequence – to the specific injury pattern enhances stability and recovery
• Clinical examination remains indispensable, as MRI may miss certain ligament injuries
• A structured, multidisciplinary rehabilitation protocol is key to regaining full knee function and preventing stiffness.
References
- 1. Pinheiro IN, Pedrinha IS, Maia PA, Cortes AR, Albuquerque RP, Barretto JM. Epidemiological study on multiligament knee injuries. Rev Bras Ortop (Sao Paulo) 2022;57:675-81. [Google Scholar] [PubMed]
- 2. Al Mohammad B, Gharaibeh MA. Magnetic resonance imaging of anterior cruciate ligament injury. Orthop Res Rev 2024;16:233-42. [Google Scholar] [PubMed]
- 3. Hunter CD, Featherall J, McNamara N, Greis PE, Maak TG, Aoki SK, et al. Investigating the ligament involvement in high-energy and polytraumatic multiligament knee injuries compared with low-energy or isolated injuries. Orthop J Sports Med 2025;13:23259671241312251. [Google Scholar] [PubMed]
- 4. Joutoku Z, Kondo E, Muranaka Y, Iwasaki K, Onodera T, Yagi T, et al. Clinical outcome of bicruciate ligament reconstruction in multiple-ligament knee injuries: Comparison with bicruciate reconstruction and collateral ligament surgery. Orthop J Sports Med 2025;13:23259671251319532. [Google Scholar] [PubMed]
- 5. Ishibashi Y, Kimura Y, Sasaki E, Sasaki S, Yamamoto Y, Tsuda E. Acute primary repair of extraarticular ligaments and staged surgery in multiple ligament knee injuries. J Orthop Traumatol 2020;21:18. [Google Scholar] [PubMed]
- 6. Herman ZJ, Kaarre J, Wackerle AM, Lott A, Apseloff NA, Lesniak BP, et al. Timing of surgery and rehabilitation after multiligamentous knee reconstruction. Curr Rev Musculoskelet Med 2024;17:476-83. [Google Scholar] [PubMed]
- 7. Hirschmann MT, Iranpour F, Müller W, Friederich NF. Surgical treatment of complex bicruciate knee ligament injuries in elite athletes: What long-term outcome can we expect? Am J Sports Med 2010;38:1103-9. [Google Scholar] [PubMed]
- 8. Sundararajan SR, Sambandam B, Rajagopalakrishnan R, Rajasekaran S. Comparison of KD3-M and KD3-L multiligamentous knee injuries and analysis of predictive factors that influence the outcomes of single-stage reconstruction in KD3 injuries. Orthop J Sports Med 2018;6:2325967118794367. [Google Scholar] [PubMed]
- 9. Kim SJ, Kim SH, Jung M, Kim JM, Lee SW. Does sequence of graft tensioning affect outcomes in combined anterior and posterior cruciate ligament reconstructions? Clin Orthop Relat Res 2015;473:235-43. [Google Scholar] [PubMed]
- 10. Goyal T, Paul S, Choudhury AK, Sethy SS. Full-thickness peroneus longus tendon autograft for anterior cruciate reconstruction in multi-ligament injury and revision cases: Outcomes and donor site morbidity. Eur J Orthop Surg Traumatol 2023;33:21-7. [Google Scholar] [PubMed]
- 11. Crum RJ, De Sa D, Kanakamedala AC, Obioha OA, Lesniak BP, Musahl V. Aperture and suspensory fixation equally efficacious for quadriceps tendon graft fixation in primary ACL reconstruction: A systematic review. J Knee Surg 2020;33:704-21. [Google Scholar] [PubMed]
- 12. Fischenich KM, Pauly HM, Button KD, Fajardo RS, DeCamp CE, Haut RC, et al. A study of acute and chronic tissue changes in surgical and traumatically-induced experimental models of knee joint injury using magnetic resonance imaging and micro-computed tomography. Osteoarthritis Cartilage 2017;25:561-9. [Google Scholar] [PubMed]
- 13. Owens BD, Neault M, Howard RS, DeBerardino TM, Taylor DC. Multiple ligament knee injuries: A clinical and functional analysis of 30 cases. Am J Sports Med 2007;35:418-23. [Google Scholar] [PubMed]
- 14. Wascher DC. High-velocity knee dislocation with vascular injury. Treatment principles. Clin Sports Med 2000;19:457-77. [Google Scholar] [PubMed]
- 15. Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med 2010;38:804-9. [Google Scholar] [PubMed]
- 16. Stannard JP, Brown SL, Farris RC, McGwin G Jr., Volgas DA. The posterolateral corner of the knee: Repair versus reconstruction. Am J Sports Med 2005;33:881-8. [Google Scholar] [PubMed]
- 17. Fanelli GC, Edson CJ. Surgical treatment of combined PCL-ACL medial side injuries of the knee: 2- to 10-year follow-up. Arthroscopy 2002;18:703-7. [Google Scholar] [PubMed]
- 18. LaPrade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: An in vitro biomechanical study. Am J Sports Med 2010;38:330-8. [Google Scholar] [PubMed]
- 19. Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: A systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am 2009;91:2946-57. [Google Scholar] [PubMed]
- 20. Engebretsen L, Risberg MA, Robertson B, Lew WD, Johanessen EA. Current concepts in treatment of anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc 2009;17:857-63. [Google Scholar] [PubMed]
- 21. King AH, Krych AJ, Prince MR, Pareek A, Stuart MJ. Surgical outcomes and return to sport following multiligament knee injury: A systematic review and meta-analysis. J Bone Joint Surg Am 2020;102:1670-8. [Google Scholar] [PubMed]
- 22. Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med 2001;30:718-27. [Google Scholar] [PubMed]
- 23. Makaram NS, Murray IR, Geeslin AG, Chahla J, Moatshe G, LaPrade RF. Diagnosis and treatment strategies of the multiligament injured knee: A scoping review. Br J Sports Med 2023;57:543-50. [Google Scholar] [PubMed]
- 24. Vaishya R, Patralekh MK, Vaish A, Tollefson LV, LaPrade RF. Effect of timing of surgery on the outcomes and complications in multi-ligament knee injuries: An overview of systematic reviews and a meta-analysis. Indian J Orthop 2024;58:1175-87. [Google Scholar] [PubMed]
- 25. Amit J, Subhash R, Pranodan P, Bibek B. Graft options for the reconstruction of multi-ligament knee injury: A systematic review. Inidan J Orthop 2025;59:453-63. [Google Scholar] [PubMed]
- 26. De Fortuny LM, Santoli A, Giovanoulis V, Vasiliadis AV, Perelli S, Monllau JC, et al. How do surgically treated multiligamentous knee injuries affect overall complication rate and especially stiffness? A systematic review. Knee Surg Relat Res 2025;37:18. [Google Scholar] [PubMed]
- 27. Sleem B, Nassar JE, Tollefson LV, LaPrade RF. Management and reconstruction strategies for multiligament knee injuries: Advances in diagnosis, surgical techniques, and rehabilitation. J Arthrosc Surg Sports Med 2025;6:112-24. [Google Scholar] [PubMed]
- 28. Pardiwala DN, Subbiah K, Thete R, Jadhav R, Rao N. Multiple ligament knee injuries: Clinical practice guidelines. J Arthrosc Surg Sports Med 2022;3:40-9. [Google Scholar] [PubMed]
- 29. LaPrade RF, Floyd ER, Carlson GB, Moatshe G, Chahla J, Monson JK. Multiple ligament anatomic-based reconstructions of the knee: State of the art. J Arthrosc Surg Sports Med 2022;3:18-33. [Google Scholar] [PubMed]
- 30. Held MF, North D, Von Bormann RB, Wascher DC, Richter DL, Schenck RC. Advances and trends in multiligament injuries of the knee relevant to low-resource settings. J Arthrosc Surg Sport Med 2020;1:118-25. [Google Scholar] [PubMed]
- 31. Opoku M, Abdramane AM, Abdirahman A, Fang M, Li Y, Xiao W. Can peroneus longus tendon autograft become an alternative to hamstring tendon autograft for anterior cruciate ligament reconstruction: A systematic review and meta-analysis of comparative studies. J Orthop Surg Res 2025;20:719. [Google Scholar] [PubMed]
- 32. Vaishya R, Gupta BM, Mamdapur GM, Vaish A. Multiligamentous knee injury: A scientometric assessment of global publications during 2008-2023. Indian J Orthop 2024;58:1213-23. [Google Scholar] [PubMed]
- 33. Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new knee society knee scoring system. Clin Orthop Relat Res 2012;470:3-19. [Google Scholar] [PubMed]
- 34. E Albuquerque RP, Giordano V, Calixto A, Malzac F, Aguiar C, Do Amaral NP, et al. Analysis on the modified lysholm functional protocol among patients with normal knees. Rev Bras Ortop 2015;46:668-74. [Google Scholar] [PubMed]