UBES is a safe, minimally invasive technique offering durable pain relief, neurological recovery, and excellent functional outcomes.
Dr. Hari Govind Patel, Department of Orthopaedics, Gandhi Medical College, Bhopal, Madhya Pradesh, India. E-mail: harigovindpatel88@gmail.com
Introduction: Unilateral biportal endoscopic surgery (UBES) has emerged as a promising minimally invasive technique for treating lumbar spine disorders. However, a comprehensive evaluation of its long-term outcomes still needs to be improved.
Aims and Objectives: This prospective study aimed to evaluate the efficacy and safety of posterior decompression for lumbar disc prolapse done by unilateral biportal endoscopy (UBE), including neurological improvement, functional status, and complications.
Materials and Methods: Consecutive patients undergoing UBES were included from a tertiary care center, Hamidia Hospital, associated with Gandhi Medical College, Bhopal, Madhya Pradesh. Demographic data, pre-operative clinical characteristics, and surgical details were collected. Neurological improvement was assessed at preoperative, 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively. Functional assessment using Visual Analog Scale (VAS) scores, Oswestry disability index (ODI), and Macnab criteria was performed at pre-operative, 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively at each follow-up visit.
Results: 50 patients of lumbar disc prolapse (66% male and 34% female) with a mean age of 40.38 ± 9.76 were enrolled, who underwent posterior decompression by UBE surgeries, most performed at L4-L5 (42%) and L5-S1 (40%) levels. Neurological status significantly improved postoperatively, with sustained enhancement in 1 year (96% improvement). Functional assessment revealed significant reductions in ODI scores (from 84.52 ± 4.04 preoperatively to 14.18 ± 3.2 [P = 0.001] at 1 year), VAS scores for back and leg pain (from 8.40 ± 0.756 preoperatively to 0.40 ± 0.495 [P = 0.001] at 1 year), and Macnab criteria outcomes as excellent at 1 year in 96% of patients.
Conclusion: UBES demonstrates favorable outcomes for lumbar disc prolapse on 1-year follow-up, including neurological improvement, pain relief, and functional outcomes. UBES represents a promising minimally invasive approach for treating lumbar spine disorders, potentially enhancing patient quality of life.
Keywords: Unilateral biportal endoscopic surgery, lumbar spine, minimally invasive surgery, short-term outcomes, pain relief.
Lumbar disc herniation remains one of the leading causes of low back pain and radiculopathy, significantly affecting quality of life and functional capacity worldwide [1]. With rapid advancements in minimally invasive spine surgery, unilateral biportal endoscopic discectomy (UBED) has gained considerable attention as it offers superior visualization, reduced muscle trauma, faster post-operative recovery, and preservation of spinal stability compared with traditional open or microdiscectomy techniques [2,3,4,5]. Over recent years, UBED has been increasingly adopted due to its dual-portal system, which allows independent viewing and working channels, enabling more precise decompression of neural elements while minimizing collateral tissue damage [6]. Despite expanding clinical use, high-quality prospective evidence evaluating UBED outcomes remains limited. Current literature is dominated by retrospective analyses or short-term follow-up studies, leaving important questions unanswered regarding long-term pain relief, neurological recovery, functional improvement, and complication rates [7,8]. In addition, variations in surgical expertise and technique create uncertainties about its reproducibility across different clinical settings. Consequently, there is a need for robust prospective data to determine the true clinical effectiveness of UBED in managing prolapsed intervertebral discs [9]. To fill this gap, the present study conducts a single-center prospective analysis to assess clinical outcomes following UBED in patients with lumbar disc herniation. By systematically evaluating pain scores, functional outcomes, neurological improvement, and procedure-related complications, this research aims to provide stronger evidence on the efficacy, safety, and applicability of UBED as a minimally invasive surgical option for treating prolapsed intervertebral discs.
Study design
This prospective observational study was employed to evaluate the outcomes of unilateral biportal endoscopic surgery (UBES) for lumbar disc prolapse in 50 patients. The study was conducted by the principles outlined in the Declaration of Helsinki and approved by the Institutional Ethics Committee.
Patient selection
The required sample size was computed using the standard formula based on an estimated prevalence of lumbar disc prolapse of 1.7% (P = 0.017), with a confidence level of 95% (Z = 3.84) and an allowable margin of error of 13% (d = 0.13). The minimum calculated sample size was 32 subjects [10]. Furthermore, all consecutive patients meeting the inclusion criteria and operated during the study period were enrolled to enhance the power of the study. Patients undergoing UBES for symptomatic lumbar spine disorders at a tertiary care center, Hamidia Hospital, associated with Gandhi Medical College, Bhopal, Madhya Pradesh, were considered for inclusion in the study. Inclusion criteria comprised adult patients (age ≥18 years) diagnosed clinically and radiologically by X-ray and magnetic resonance imaging (Fig. 1a and b) with lumbar disc herniation or disc prolapse refractory to conservative management for at least 3 months. Patients with previous lumbar spine surgery, significant comorbidities precluding surgery, or incomplete follow-up data were excluded.
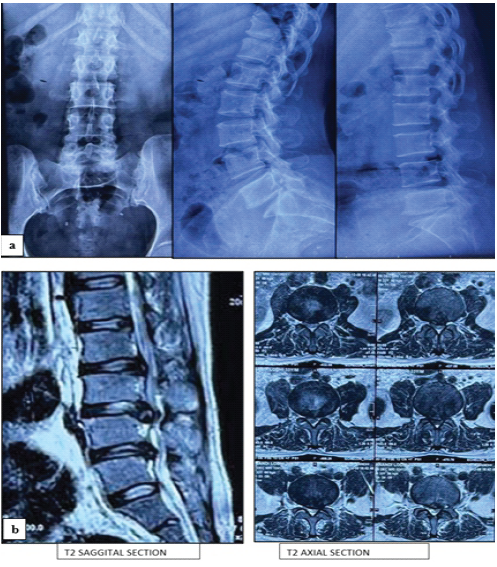
Figure 1: (a) Pre-operative X-ray anteroposterior and dynamic view, (b) Pre-operative magnetic resonance imaging.
Data collection
Demographic data (age, sex, occupation), pre-operative clinical characteristics (pathology, level of surgery), and surgical details (operative time, intra-op and post-operative complications) were collected prospectively. The pre-operative neurological status was assessed using standardized criteria, and comparisons were made at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively. Functional assessment was performed using the Oswestry disability index (ODI), Visual Analog Scale (VAS) scores for back and leg pain, and Macnab criteria outcomes at pre-operative, 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively.
Outcome measures
The primary outcome measures included changes in VAS scores for back and leg pain, ODI scores, and Macnab criteria. Pain relief was defined as a reduction in VAS score by ≥50%. Functional improvement was assessed using the ODI, with lower scores indicating better functional status and Macnab criteria, categorized as excellent, good, fair, or poor [11]. Complications, reoperation rates, and length of hospital stay were also recorded.
Surgical technique
All surgeries were performed by experienced spine surgeons proficient in UBES techniques. Patients were placed in the prone position under general anesthesia. A standard posterior approach was employed, and the surgical level was confirmed using fluoroscopy (Fig. 2a). Two small portals were created unilaterally, allowing for direct visualization of the targeted pathology. Sequential dilation of the portals was performed, followed by inserting the endoscope and working instruments (Fig. 2b). Decompression of neural structures, including discectomy, laminectomy, and foraminal decompression, was performed as indicated, under direct monitoring on the endoscope (Fig. 2c,d,e). Hemostasis was achieved, and the portals were closed (Fig. 2f).
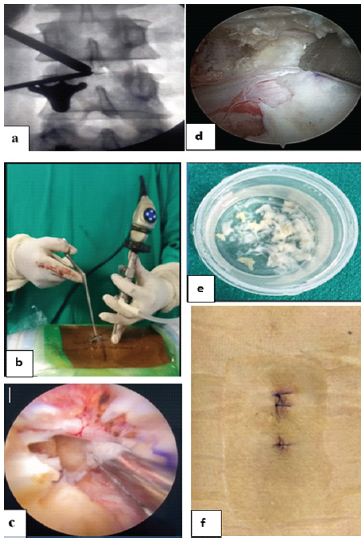
Figure 2: Intraop images. (a) Fluoroscopic image (b) image showing disc removal with Kerrison punch (cand d) endoscopic images (e) disc sample. (f) Post-operative image of surgical wound closure.
Statistical analysis
Data were compiled using MS Excel and analyzed using IBM Statistical Package for the Social Sciences software version 20. Categorical data were expressed as frequencies and proportions, whereas continuous data were expressed as means and standard deviations with ranges. The Chi-square test was used to assess the improvement in ODI and MACNAAB scores over various follow-ups, whereas paired t-tests and repeated-measures analysis of variance were used to assess the improvement in VAS scores at various follow-ups. P < 0.05 was considered statistically significant.
Ethical considerations
The Institutional Review Board approved the study protocol of Hamidia Hospital, associated with Gandhi Medical College, Bhopal, Madhya Pradesh, IRB Number 91/IEC/2023 on April 25, 2023, and all patients provided written informed consent before enrollment. Patient confidentiality was maintained throughout the study process.
This study was conducted on a total of 50 patients with lumbar disc prolapse and lumbar canal stenosis, who underwent posterior decompression by unilateral biportal endoscopy (UBE). The findings of the present study are tabulated (Table 1).
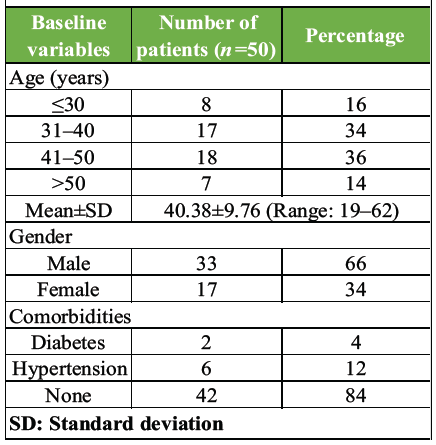
Table 1: Distribution of patients according to baseline variables
The study included a total of 50 patients with a mean age of 40.38 ± 9.76 years, ranging from 19 to 62 years. The majority of patients were in the 41–50-year age group (36.0%), followed closely by those aged 31–40 years (34.0%). In terms of gender distribution, males were predominant, comprising 66.0% (n = 33) of the cohort, whereas females accounted for 34.0% (n = 17). Regarding comorbidities, a large proportion of the participants (84.0%) did not report any associated medical conditions. Among those with comorbidities, 12.0% (n = 6) had hypertension and 4.0% (n = 2) had diabetes mellitus (Table 1).
The most common spinal level operated on was L4-L5, accounting for 42.0% of cases, followed closely by L5-S1 in 40.0% of patients. The mean procedure time was 72.58 ± 19.24 min, with a range between 48 and 160 min. Most surgeries (66.0%) lasted between 60 and 120 min, while 28.0% were completed in 60 min or less, and only 6.0% extended beyond 120 min. Intraoperatively, complications were rare, with only one case (2.0%) of dural tear reported; the remaining 98.0% experienced no complications. Postoperatively, 4.0% of patients developed disc infections, whereas the vast majority (96.0%) had an uncomplicated recovery (Table 2).
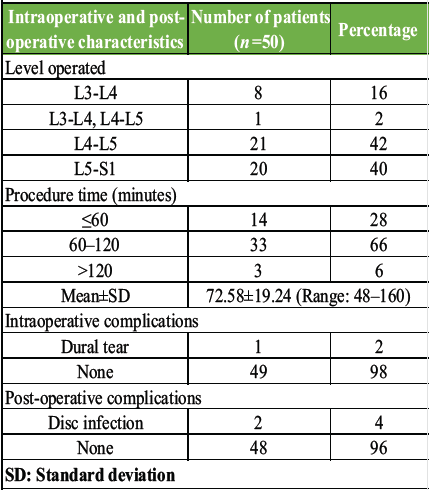
Table 2: Intraoperative and postoperative characteristics of the study population
The ODI scores in this study showed a significant and progressive improvement following surgery. Preoperatively, patients had a mean ODI score of 84.52 ± 4.04, with the majority (74%) categorized as having complete disability (81–100%), and the remaining 26% as crippled (61–80%). At 2 weeks postoperatively, the mean ODI improved to 61.8 ± 5.7, with 72% still in the “crippled” category and 28% in the “severe disability” range, showing a statistically significant improvement (P = 0.03). By 6 weeks, the mean ODI had decreased to 47.5 ± 6.9, with the majority (76%) in the “severe disability” category and 22% in “moderate disability” (P = 0.01). Continued improvement was seen at 3 months, where the mean ODI dropped to 35.8 ± 6.2, with 80% of patients now classified as having “moderate disability” and 20% as “severe disability” (P = 0.001). At 6 months, the mean ODI further improved to 23.08 ± 4.8, with 60% in the “moderate disability” range and 40% achieving “minimal disability” (P = 0.001). Finally, at 1 year postoperatively, all patients (100%) achieved minimal disability, with a mean ODI of 14.18 ± 3.2 (P = 0.001). The trend across all time intervals was highly statistically significant (P = 0.001), indicating a consistent and meaningful recovery following surgical intervention (Table 3).
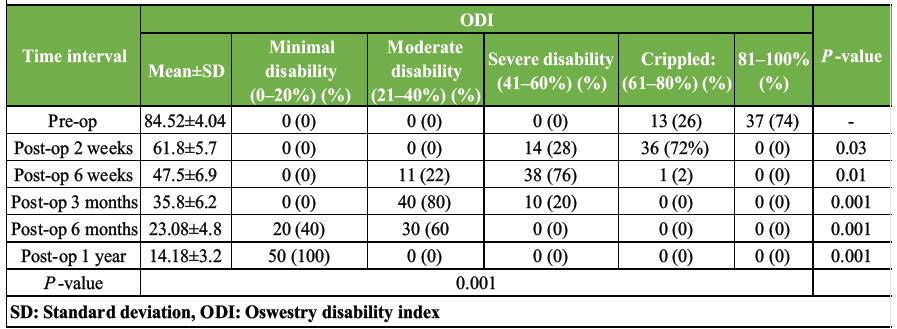
Table 3: Comparison of ODI score before and after treatment
The Macnab criteria outcomes showed a clear and statistically significant improvement in patient satisfaction and functional recovery following surgery over the 1-year follow-up period. At 2 weeks postoperatively, the majority of patients (92%) reported only fair outcomes, with just 8% rating their recovery as good, and none reporting excellent or poor outcomes. By 6 weeks, improvement was noted, with 34% of patients reporting good outcomes and 66% still at fair level (P = 0.042). At 3-month post-operative, 68% reported good results, and 30% experienced excellent recovery, with only 2% still in the fair category (P = 0.001). This positive trend continued at 6 months, where 94% rated their outcome as excellent, 4% as good, and only 2% remained in the fair category (P = 0.001). Finally, at 1 year, 96% of patients rated their outcome as excellent, and the remaining 4% reported a good outcome. There were no patients in the fair or poor categories. The overall P-value across all time intervals was 0.001, confirming a statistically significant and steady improvement in functional outcomes as per Macnab criteria following surgical intervention (Table 4).
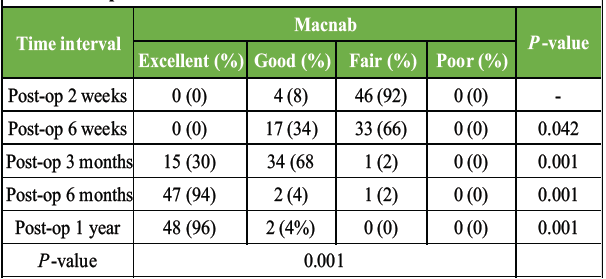
Table 4: Comparison of Macnab before and after treatment
The VAS scores demonstrated a marked and statistically significant reduction in pain levels over 1 year following the surgical procedure. Preoperatively, patients reported a high mean VAS score of 8.40 ± 0.756, indicating severe pain. At 2 weeks postoperatively, the mean score dropped significantly to 3.82 ± 0.691 (P = 0.001), reflecting substantial early pain relief. Continued improvement was observed at subsequent follow-ups, with the score decreasing to 2.86 ± 0.729 at 6 weeks, 1.90 ± 0.614 at 3 months, and 0.98 ± 0.742 at 6 months. By 1 year postoperatively, the mean VAS score had further declined to 0.40 ± 0.495, indicating minimal residual pain. Each of these reductions was statistically significant (P = 0.001), highlighting the sustained efficacy of the surgical intervention in alleviating pain over time (Fig. 3).
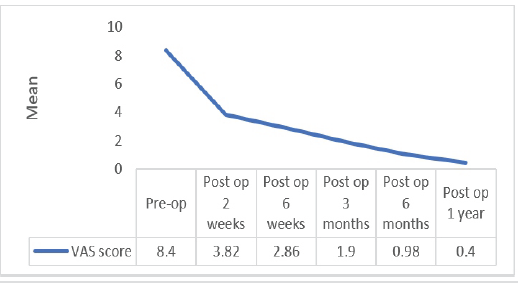
Figure 3: Comparison of Visual Analog Scale score before and after treatment.
UBES has emerged as a promising minimally invasive technique for treating lumbar spine disorders, offering significant advantages in terms of reduced tissue trauma, faster recovery, and improved patient outcomes. In this study, we evaluated the long-term outcomes of UBES for lumbar disc prolapse, considering various factors such as neurological improvement and functional status. Our findings demonstrate significant improvements in neurological status following UBES, with most patients experiencing improvement in neurological deficits in 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively. This aligns with previous studies indicating the efficacy of UBES in relieving neural compression and restoring neurological function [12,13]. Notably, the sustained improvement observed for 1 year postoperatively suggests the durability of surgical outcomes. Functional assessment using the ODI, VAS scores, and Macnab criteria revealed substantial improvements in pain relief and functional status following UBES. The significant reductions in ODI scores and VAS scores for back and leg pain at all post-operative time points reflect the effectiveness of UBES in alleviating symptoms and improving overall quality of life. These findings are consistent with previous literature supporting the favorable functional outcomes of UBES for lumbar spine disorders [14,15]. As assessed by the Macnab criteria, patient satisfaction and functional outcome were high at all follow-up time points, with most patients reporting excellent or good outcomes. This underscores patients’ subjective satisfaction with the surgical results and highlights the overall success of UBES in meeting patient expectations. Our results align with previous studies reporting high patient satisfaction rates following UBES [16,17]. In Soliman’s [18] prospective case series of 43 patients, outcomes based on the modified Macnab criteria were excellent in 78%, good in 17%, and poor in 5%, demonstrating high effectiveness in symptom relief; notably, the present study achieved a slightly higher rate of “Excellent” outcomes with no poor or fair results. Kim et al. [19] reported that 81% of patients experienced “Good” or “Excellent” outcomes 2 years after unilateral laminotomy with bilateral decompression using a 30° arthroscope. Similarly, Kim and Jung [20] found 51.7% “Excellent” and 41.4% “Good” outcomes 18 months after UBESS. Pao et al. [11] also supported UBE’s effectiveness, with 58% “Excellent” and 35.8% “Good” results in their cohort study. Dural tear in one patient is the only intraoperative complication. These results are comparable to the findings reported by Kim et al. [21] who observed a 3.2% incidence of dural tears in patients undergoing biportal endoscopic spinal surgery. Disc infection in two patients occurred postoperatively. Supporting data from Kpegeol et al. [22] and Chiu et al. [23] further highlight the lower disc infection rates seen with endoscopic decompression. While our study contributes valuable insights into the long-term outcomes of UBES, several limitations should be acknowledged. The study was conducted at a single center with a relatively small sample size, limiting the generalizability of the findings. The follow-up period also precludes assessment of more long-term outcomes and recurrence rates. Future multicenter studies with larger cohorts and longer follow-up durations are warranted to confirm our findings and evaluate the durability of surgical outcomes.
Our study demonstrates favorable outcomes of UBES for lumbar disc prolapse after 1 year of follow-up, with significant improvements in neurological status, functional outcomes, and patient satisfaction. UBES represents a promising minimally invasive approach for treating lumbar spine disorders, offering effective symptom relief and enhancing patient quality of life.
UBE is a minimally invasive spinal surgery technique offering superior visualization, minimal tissue disruption, reduced postoperative pain, and faster recovery compared to traditional methods. It is particularly effective for lumbar disc herniation and spinal stenosis, enabling precise decompression with preserved spinal stability. Clinical outcomes show significant improvement in pain, function, and patient satisfaction. However, UBE has a steep learning curve, requiring specialized training and equipment, limiting its adoption in resource-poor settings. While promising, further long-term comparative studies are needed to fully assess its benefits and potential complications, supporting broader integration into modern spine care practices.
References
- 1. Qi L, Luo L, Meng X, Zhang J, Yu T, Nie X, et al. Risk factors for lumbar disc herniation in adolescents and young adults: A case-control study. Front Surg 2023;9:1009568. [Google Scholar] [PubMed]
- 2. Kim M, Lee S, Kim HS, Park S, Shim SY, Lim DJ. A comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for lumbar disc herniation in the Korean: A meta-analysis. Biomed Res Int 2018;2018:9073460. [Google Scholar] [PubMed]
- 3. Choi DJ, Jung JT, Lee SJ, Kim YS, Jang HJ, Yoo B. Biportal endoscopic spinal surgery for recurrent lumbar disc herniations. Clin Orthop Surg 2016;8:325-9. [Google Scholar] [PubMed]
- 4. Kwon O, Yoo SJ, Park JY. Comparison of unilateral biportal endoscopic discectomy with other surgical technics: A systemic review of indications and outcomes of unilateral biportal endoscopic discectomy from the current literature. World Neurosurg 2022;168:349-58. [Google Scholar] [PubMed]
- 5. Liawrungrueang W, Lee HJ, Kim SB, Park SM, Cholamjiak W, Park HJ. A systematic review of biportal endoscopic spinal surgery with interbody fusion. Asian Spine J 2025;19:275-91. [Google Scholar] [PubMed]
- 6. Kim JE, Choi DJ, Park EJ, Lee HJ, Hwang JH, Kim MC, et al. Biportal endoscopic spinal surgery for lumbar spinal stenosis. Asian Spine J 2019;13:334-42. [Google Scholar] [PubMed]
- 7. Park DY, Upfill-Brown A, Curtin N, Hamad CD, Shah A, Kwon B, et al. Clinical outcomes and complications after biportal endoscopic spine surgery: A comprehensive systematic review and meta-analysis of 3673 cases. Eur Spine J 2023;32:2637-46. [Google Scholar] [PubMed]
- 8. Deng C, Li X, Wu C, Xie W, Chen M. One-hole split endoscopy versus unilateral biportal endoscopy for lumbar degenerative disease: A systematic review and meta-analysis of clinical outcomes and complications. J Orthop Surg Res 2025;20:187. [Google Scholar] [PubMed]
- 9. Kwon H, Park JY. The role and future of endoscopic spine surgery: A narrative review. Neurospine 2023;20:43-55. [Google Scholar] [PubMed]
- 10. Singh V, Malik M, Kaur J, Kulandaivelan S, Punia S. A systematic review and meta-analysis on the efficacy of physiotherapy intervention in management of lumbar prolapsed intervertebral disc. Int J Health Sci (Qassim) 2021;15:49-57. [Google Scholar] [PubMed]
- 11. Pao JL, Lin SM, Chen WC, Chang CH. Unilateral biportal endoscopic decompression for degenerative lumbar canal stenosis. J Spine Surg 2020;6:438-46. [Google Scholar] [PubMed]
- 12. Lee CW, Yoon KJ, Jun JH. Biportal endoscopic spinal surgery for lumbar spinal stenosis. Asian Spine J 2018;12:569-71. [Google Scholar] [PubMed]
- 13. Kim HS, Paudel B, Jang JS, Lee K, Oh SH, Jang IT, et al. Percutaneous endoscopic lumbar discectomy for all types of lumbar disc herniations (LDH) including severely difficult and extremely difficult LDH cases. Pain Physician 2018;21:E401-8. [Google Scholar] [PubMed]
- 14. Ahn Y. Transforaminal percutaneous endoscopic lumbar discectomy: Technical tips to prevent complications. Expert Rev Med Devices 2012;9:361-6. [Google Scholar] [PubMed]
- 15. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931-9. [Google Scholar] [PubMed]
- 16. Kim JE, Choi DJ. Clinical and radiological outcomes of unilateral biportal endoscopic decompression by 30° Arthroscopy in lumbar spinal stenosis: Minimum 2-year follow-up. Clin Neurol Neurosurg 2019;178:101-7. [Google Scholar] [PubMed]
- 17. Choi DJ, Choi CM, Jung JT, Lee SJ, Kim YS. Learning curve associated with complications in biportal endoscopic spine surgery: Challenges and strategies. Asian Spine J 2016;10:624-9. [Google Scholar] [PubMed]
- 18. Soliman HM. Irrigation endoscopic discectomy: A novel percutaneous approach for lumbar disc prolapse. Eur Spine J 2013;22:1037-44. [Google Scholar] [PubMed]
- 19. Kim JE, Choi DJ, Park EJ. Biportal endoscopic spinal surgery for recurrent lumbar disc herniations. Clin Orthop Surg 2018;10:147-52. [Google Scholar] [PubMed]
- 20. Kim N, Jung SB. Percutaneous unilateral biportal endoscopic spine surgery using a 30-degree arthroscope in patients with severe lumbar spinal stenosis: A technical note. Clin Spine Surg 2019;32:324-9. [Google Scholar] [PubMed]
- 21. Kim HS, Choi SH, Shim DM, Lee IS, Oh YK, Woo YH. Advantages of new endoscopic unilateral laminectomy for bilateral decompression (ULBD) over conventional microscopic ULBD. Clin Orthop Surg 2020;12:330-6. [Google Scholar] [PubMed]
- 22. Kpegeol CK, Jain VS, Ansari D, Ammanuel SG, Page PS, Josiah DT. Surgical site infection rates in open versus endoscopic lumbar spinal decompression surgery: A retrospective cohort study. World Neurosurgery X 2024;22:100347. [Google Scholar] [PubMed]
- 23. Myers D. Endoscopic Decompression Versus Open Laminectomy for Lumbar Spinal Stenosis: A Prospective Safety Study. Yale School of Medicine Physician Associate Program Theses; 2022. p. 136. [Google Scholar] [PubMed]