Preserving a previously transferred anterior latissimus dorsi tendon during reverse shoulder arthroplasty can help maintain internal rotation and optimize post-operative function.
Dr. Chang Hee Baek, Department of Orthopaedic Surgery, Yeosu Baek Hospital, 50, Yeosu 1-ro, Yeosusi, Jeollanam-do, Yeosu-si, Republic of Korea. Email: yeosubaek@gamail.com
Introduction: Anterior latissimus dorsi tendon transfer (LDT) is a joint-preserving procedure for irreparable subscapularis (SSC) tears, providing pain relief and functional improvement. However, progressive glenohumeral osteoarthritis may develop over time. When arthritic changes become advanced, conversion to reverse total shoulder arthroplasty (rTSA) may be required. This report describes the long-term survivorship of anterior LDT and subsequent conversion to rTSA with preservation of the transferred tendon.
Case Report: A 61-year-old woman underwent anterior LDT for an irreparable SSC tear. Ten years later, she developed painful dysfunction and radiographic evidence of advanced glenohumeral osteoarthritis. rTSA was performed while preserving the LDT insertion on the lesser tuberosity. At the 2-year follow-up, pain decreased markedly (Visual Analog Scale 6→1), functional scores improved (Constant 56→87; American Shoulder and Elbow Surgeons 59→87), and range of motion was enhanced (forward elevation 165°, external rotation 50°, internal rotation T12). Radiographs confirmed stable fixation of prosthetic components, and ultrasonography demonstrated an intact, well-preserved LDT.
Conclusion: Anterior LDT can provide durable functional benefit for up to a decade in irreparable SSC tears. When degenerative progression necessitates arthroplasty, conversion to rTSA with preservation of the tendon transfer can achieve excellent outcomes, particularly in maintaining internal rotation strength.
Keywords: Irreparable subscapularis tear, latissimus dorsi tendon transfer, reverse shoulder arthroplasty.
Irreparable subscapularis (SSC) tears can lead to limited active forward elevation (FE) and internal rotation (IR) of the shoulder, often accompanied by anterosuperior subluxation and pseudoparalysis [1]. Tendon transfer procedures have been introduced as joint-preserving alternatives for patients with irreparable SSC [2,3]. Among these, anterior latissimus dorsi tendon transfer (LDT) has gained attention as a viable option with relatively low complication rates [4,5]. Compared with pectoralis major transfer, LDT better replicates the native line of pull of the SSC tears, thereby restoring IR strength and shoulder kinematics with encouraging short-term outcomes [5]. Although post-operative results following anterior LDT are generally promising, the risk of progressive glenohumeral osteoarthritis remains a concern [6,7]. In a long-term study, Baek et al. reported that anterior LDT for irreparable SSC tears provided sustained improvements in shoulder pain, active range of motion (ROM), and IR strength for a mean follow-up of 8.7 years. However, radiographic findings revealed a decrease in acromiohumeral distance (AHD) and progression of arthritic change of the glenohumeral joint, highlighting the potential risk for degenerative changes despite clinical benefits [8]. Here, we present the case of a 61-year-old patient who underwent anterior LDT 10 years earlier for an irreparable SSC tear and later developed progressive glenohumeral osteoarthritis. The patient presented with painful shoulder dysfunction and restricted ROM, and reverse total shoulder arthroplasty (rTSA) was performed while preserving the LDT to maintain IR function.
A 61-year-old right-hand-dominant woman presented with progressive shoulder pain and loss of function. Ten years earlier, she had undergone anterior LDT for an irreparable SSC tear without arthritic change (Fig. 1).
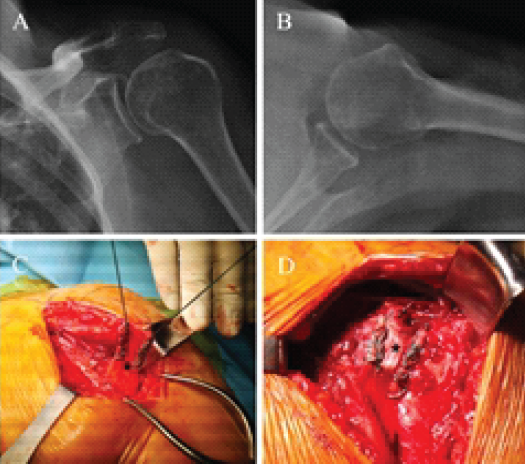
Figure 1: Pre-operative radiograph and anterior latissimus dorsi tendon transfer. (a) Anteroposterior and (b) axil radiograph of left shoulder showing no arthritic change in 61-year-old woman. (c) The latissimus dorsi tendon (asterisk) is harvested and prepared with Krackow suture. (d) The latissimus dorsi tendon (sterisk) is transferred to the lesser tuberosity.
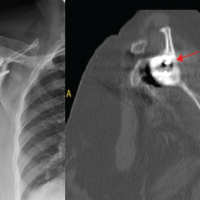
Over time, she experienced worsening pain and functional limitations, particularly during daily tasks such as food preparation, toileting, and personal hygiene, which significantly reduced her quality of life. Clinical evaluation demonstrated FE of 130°, abduction of 130°, external rotation (ER) of 40°, and IR to the L3 vertebral level. Strength testing showed values of 20.1 N for FE, 24.3 N for abduction, 22.7 N for ER, and 27.9 N for IR. Patient-reported outcomes indicated moderate disability, with a visual analogue scale (VAS) score of 6/10, a constant score of 56/100, and the American Shoulder and Elbow Surgeons (ASES) score of 59/100. Radiographs revealed advanced glenohumeral osteoarthritis with joint space narrowing and superior migration of the humeral head. Magnetic resonance imaging demonstrated humeral head cartilage loss, glenoid wear, and an intact, well-preserved latissimus dorsi transfer (Fig. 2). Considering the severity of osteoarthritis and persistent symptoms, rTSA was performed with preservation of the prior LDT.
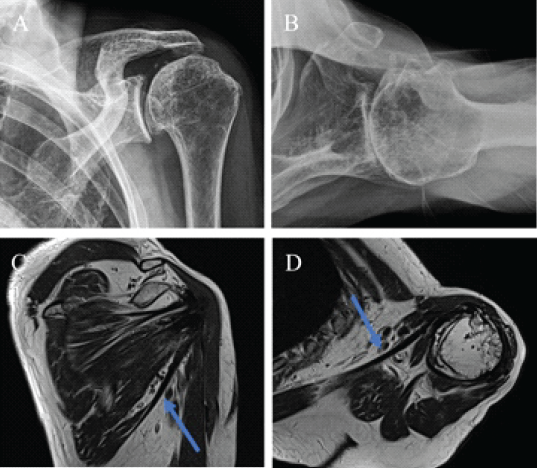
Figure 2: Radiographs and magnetic resonance imaging 10 years after anterior latissimus dorsi tendon transfer. (a) Anteroposterior and (b) axil radiograph of left shoulder demonstrating advanced glenohumeral osteoarthritis with joint space narrowing and superior migration of the humeral head. (c) Coronal and (d) axial T2-weighted magnetic resonance image showing well-preserved transferred latissimus dorsi tendon attached to the lesser tuberosity.
Surgical procedure
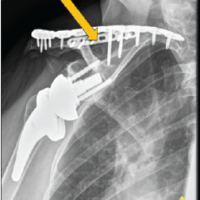
The patient was positioned in the beach-chair position under general anesthesia combined with an interscalene block for post-operative pain control. A standard deltopectoral approach was used. Careful dissection was performed to expose the shoulder joint while preserving the integrity of the previously transferred latissimus dorsi tendon. The latissimus dorsi transfer was visualized at its insertion on the lesser tuberosity and confirmed to be firmly and securely attached. Preserving latissimus dorsi transfer was considered critical to maintaining IR strength and maximizing post-operative functional outcomes. rTSA was performed using the Equinoxe reverse shoulder system (Exactech Inc., Gainesville, FL, USA). The humeral head osteotomy was carried out just superior to the LDT insertion and the greater tuberosity, at an inclination of 132.5° and retroversion of 20°. Particular attention was paid to avoiding damage to the transferred tendon insertion during this step. After circumferential capsulectomy, the glenoid was exposed and prepared. The baseplate was implanted in the inferior portion of the glenoid with an intentional inferior tilt to minimize scapular notching and optimize stability. A glenosphere was then secured onto the baseplate. On the humeral side, both metaphyseal and epiphyseal bone were sequentially reamed using progressively larger reamers, with care taken to conserve cancellous bone for biological fixation. A press-fit humeral stem was then inserted with final impaction. The humeral component was reduced onto the glenosphere, and stability was confirmed. Intraoperative testing demonstrated smooth motion without impingement throughout internal and ER. Finally, the LDT was re-examined to ensure that its attachment to the lesser tuberosity remained intact and tension-free following reduction. This preservation was expected to enhance IR function, which is often compromised after rTSA (Fig. 3). The wound was irrigated thoroughly and closed in layers.
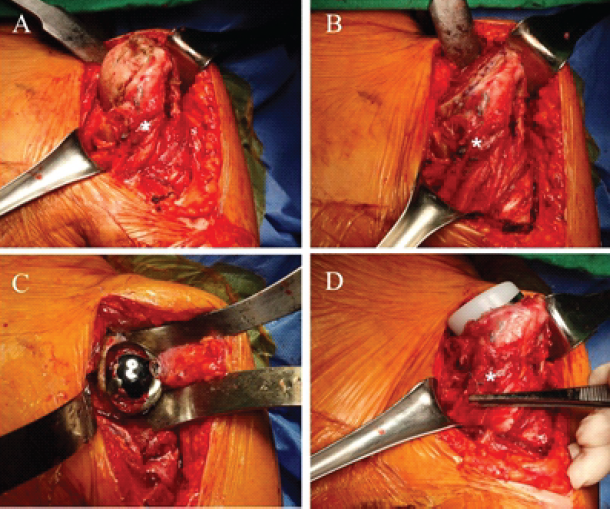
Figure 3: Conversion to reverse total shoulder arthroplasty with preservation of the anterior latissimus dorsi transfer (LDT). (a) Intraoperative photograph showing the preserved LDT at its insertion on the lesser tuberosity, where it is visualized and confirmed to be firmly and securely attached. (b) The humeral head osteotomy is performed just superior to the latissimus dorsi tendon insertion and the greater tuberosity. (c) The baseplate is implanted in the inferior portion of the glenoid with an intentional inferior tilt to minimize scapular notching and optimize stability. (d) The humeral stem is inserted with preservation of the LDT.
Post-operative rehabilitation
Postoperatively, the patient was immobilized in an abduction brace for 4 weeks, although intermittent elbow, wrist, and finger motion was permitted to maintain distal joint mobility. While wearing the brace, the patient was able to perform basic daily activities such as eating and writing. After 4 weeks, the brace was discontinued, and active-assisted ROM exercises were initiated to gradually restore mobility. At 3 months, a strengthening program was introduced in all planes of motion. Heavy labor and sports activities were strictly restricted until 6 months postoperatively.
Post-operative outcome
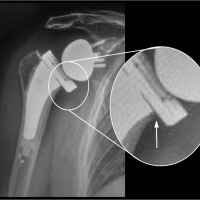
At the 2-year follow-up, the patient demonstrated substantial improvement in pain, strength, and function, reporting high satisfaction with the surgical outcome. VAS decreased to 1/10, the Constant score increased to 87/100, and the ASES score improved to 87/100. ROM was maintained or enhanced, with FE of 165°, abduction of 165°, ER of 50°, and IR to the T12 vertebral level. Strength also improved across all planes: FE 27.2 N, abduction 29.1 N, ER 23.6 N, and IR 27.1 N. Post-operative radiographs confirmed stable fixation of both humeral and glenoid components, without loosening, subsidence, or implant-related complications (Fig. 4). Ultrasonographic assessment demonstrated an intact latissimus dorsi transfer without detachment. Functionally, the patient returned to pain-free performance of daily household activities, including cooking and dishwashing, and maintained consistent satisfaction with the surgical result.
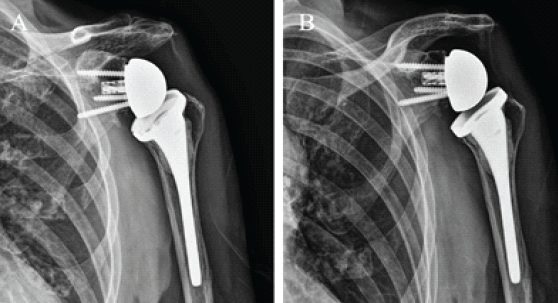
Figure 4: Anteroposterior radiographs obtained 2 years after conversion to reverse total shoulder arthroplasty. (a) Anteroposterior and (b) axil radiograph of left shoulder demonstrating stable fixation of the humeral and glenoid components without evidence of loosening, subsidence, or implant-related complications.
This case report demonstrates the durability of LDT in an irreparable SSC tear over 10 years and its compatibility with subsequent rTSA. Although the degenerative progression of the glenohumeral joint ultimately necessitated arthroplasty, preservation of the transferred tendon during rTSA contributed to maintain IR function and favorable clinical outcomes. Anterior LDT has been introduced as a joint-preserving procedure for irreparable SSC tears, with encouraging clinical outcomes in terms of pain relief, restoration of IR strength, and improvement in functional scores [1]. Previous mid- to long-term follow-up studies have demonstrated sustained functional gains for nearly a decade; however, radiographic progression of cuff tear arthropathy and narrowing of the AHD were also consistently reported, underscoring the potential for gradual degenerative changes despite preserved function [6,8]. The present case is unique in that the patient achieved a decade of functional shoulder use after anterior LDT before eventually requiring conversion to rTSA. To our knowledge, there are few reports describing such long-term survivorship of a tendon transfer before arthroplasty conversion. Most available series on conversion to rTSA after failed tendon transfers involve shorter intervals, typically within 2–5 years. This extended period of preserved function emphasizes the role of anterior LDT as a temporizing and joint-preserving strategy, capable of delaying prosthetic replacement in relatively young or active patients. Comparatively, most previously published reports describe conversion to rTSA within 2–5 years after tendon transfer due to persistent dysfunction or structural failure, rather than long-term durability before arthroplasty [6,7,8]. Moroder et al. reported progressive arthropathy after pectoralis major transfer, whereas Baek et al. demonstrated functional durability of anterior LDT up to 8.7 years but noted radiographic degeneration [6,8]. In contrast, the present case illustrates more than 10 years of preserved shoulder function, supporting the role of tendon transfer as a joint-preserving strategy capable of delaying arthroplasty in younger or active patients. Furthermore, this case demonstrates that preservation of the anterior LDT can contribute to maintenance of internal rotation and overall shoulder kinematics. From a surgical perspective, preservation of the previous LDT during rTSA was a critical aspect of this case. IR is frequently compromised after rTSA, and loss of SSC function further increases the risk of instability [9,10]. In this patient, maintaining the intact LDT provided an additional IR force vector, which likely contributed to her favorable functional outcome. This finding aligns with prior biomechanical studies suggesting that tendon transfers, particularly latissimus dorsi or pectoralis major, can augment internal rotation and enhance joint stability when combined with rTSA. Our case also highlights several technical considerations. First, careful exposure and osteotomy planning are required to avoid inadvertent damage to the transferred tendon, especially when it remains attached to the lesser tuberosity. Second, intraoperative tensioning should be confirmed following reduction to ensure that the transfer remains functional and is not impinged by the prosthetic components. Third, component positioning – such as inferior glenoid baseplate tilt and proper humeral stem retroversion – is essential to maximize stability and minimize complications. Although the clinical outcome in this case was favorable, potential complications associated with rTSA with preserving the anterior LDT, must be acknowledged. Previous studies have reported risks such as tendon rupture, post-operative stiffness, and instability following rTSA [4,5,6,7]. In addition, maintaining the integrity of the transferred tendon during osteotomy and implant positioning can be technically demanding. The absence of complications in this case may reflect the surgeon expertise and well-preserved tendon quality rather than generalized safety. Moreover, as a single case report, this study cannot evaluate complication rates or prognostic factors, emphasizing the need for larger multicenter studies to validate these findings. The main limitation of this report is its single-patient design, which precludes generalization. Nonetheless, it provides valuable insight into the natural history of a successful tendon transfer and its eventual progression to arthroplasty. Future studies should explore the long-term survivorship of tendon transfers as part of staged reconstructive strategies and assess whether preservation of these transfers during rTSA consistently enhances functional outcomes, particularly in internal rotation.
This case demonstrates that anterior LDT can provide durable pain relief and functional improvement for up to 10 years in patients with irreparable SSC tears. When glenohumeral osteoarthritis eventually progresses, conversion to rTSA while preserving the prior tendon transfer can yield excellent clinical outcomes. These findings support the concept of tendon transfer as a joint-preserving procedure that may delay arthroplasty and remain beneficial even at the time of conversion surgery.
Anterior LDT can provide durable functional improvement and pain relief for up to a decade in patients with irreparable SSC tears. Even when degenerative progression necessitates rTSA, preserving the transferred tendon during conversion surgery can maintain internal rotation function and yield excellent post-operative outcomes.
References
- 1. Collin P, Matsumura N, Lädermann A, Denard PJ, Walch G. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202. [Google Scholar] [PubMed]
- 2. Clark NJ, Elhassan BT. The role of tendon transfers for irreparable rotator cuff tears. Curr Rev Musculoskelet Med 2018;11:141-9. [Google Scholar] [PubMed]
- 3. Baek CH, Kim JG, Baek GR. Outcomes of combined anterior latissimus dorsi and teres major tendon transfer for irreparable anterosuperior rotator cuff tears. J Shoulder Elbow Surg 2022;31:2298-307. [Google Scholar] [PubMed]
- 4. Kany J, Grimberg J, Amaravathi RS, Sekaran P, Scorpie D, Werthel JD. Arthroscopically-assisted latissimus dorsi transfer for irreparable rotator cuff insufficiency: Modes of failure and clinical correlation. Arthroscopy 2018;34:1139-50. [Google Scholar] [PubMed]
- 5. Mun SW, Kim JY, Yi SH, Baek CH. Latissimus dorsi transfer for irreparable subscapularis tendon tears. J Shoulder Elbow Surg 2018;27:1057-64. [Google Scholar] [PubMed]
- 6. Moroder P, Schulz E, Mitterer M, Plachel F, Resch H, Lederer S. Long-term outcome after pectoralis major transfer for irreparable anterosuperior rotator cuff tears. J Bone Joint Surg Am 2017;99:239-45. [Google Scholar] [PubMed]
- 7. Baek CH, Kim JG, Kim BT, Kim SJ. Isolated latissimus dorsi transfer versus combined latissimus dorsi and teres major tendon transfer for irreparable anterosuperior rotator cuff tears. Clin Orthop Surg 2024;16:761-73. [Google Scholar] [PubMed]
- 8. Baek CH, Kim JG, Kim BT. Long-term outcomes of anterior latissimus dorsi tendon transfer for irreparable subscapularis tears. Bone Joint J 2024;106-B:957-63. [Google Scholar] [PubMed]
- 9. Baek CH, Kim JG, Kim BT, Kim SJ. Healed subscapularis and its clinical implications for internal rotation in humeral lateralized reverse shoulder arthroplasty. J Shoulder Elbow Surg 2025;34:1532-42. [Google Scholar] [PubMed]
- 10. Bigdon SF, Bolliger L, Albers CE, Collin P, Zumstein MA. Subscapularis in reverse total shoulder arthroplasty. J Shoulder Elb Arthroplast 2019;3:2471549219834192. [Google Scholar] [PubMed]