Intraneural ganglion cysts of the suprascapular nerve may enlarge and cause dual-site compression if the underlying labral tear is not treated, potentially resulting in asymmetric neural branch recovery.
Dr. Margaux Keppens, Faculty of Medicine, University of Leuven, Herestraat 49/bus 400, 3001, Leuven, Belgium. Email: margaux.keppens@gmail.com
Introduction: Intraneural ganglion cysts of the suprascapular nerve (SSN) are rare cystic lesions that can lead to shoulder pain, weakness, and muscle atrophy due to nerve compression. They frequently arise secondary to a capsulolabral tear, which allows joint fluid to track into the nerve through the articular branch. Although relatively uncommon, appropriate management is crucial to prevent cyst enlargement and progressive nerve damage.
Case Report: We report the case of a 63-year-old woman who presented with a 6-month history of posterior shoulder pain, weakness, and limitation in overhead activities. Magnetic resonance imaging and ultrasound identified an intraneural ganglion cyst at the spinoglenoid and the suprascapular notch in association with a superior labrum anterior to posterior lesion, while electromyography (EMG) confirmed a SSN lesion proximal to the branch to the supraspinatus muscle. Conservative management with physiotherapy, cyst aspiration, and corticosteroid injection provided partial pain relief but resulted in cyst enlargement. Follow-up EMG demonstrated partial recovery of the supraspinatus branch but no recovery of the infraspinatus branch. Arthroscopic decompression and labral debridement were performed, preserving the articular branch. Postoperatively, EMG confirmed symmetrical recovery of both the supraspinatus and infraspinatus muscles.
Conclusion: This case demonstrates that conservative treatment without addressing the underlying labral tear may allow cyst progression and cause dual-site nerve compression with asymmetric branch recovery. Early recognition, serial imaging, and EMG are essential to guide timely surgical intervention and prevent irreversible denervation. This report also supports Spinner’s unifying articular theory.
Keywords: Intraneural cyst, suprascapular nerve, suprascapular neuropathy, dual-site compression, spinoglenoid notch, superior labrum anterior to posterior lesion, articular theory.
The suprascapular nerve (SSN) is a mixed sensorimotor branch of the brachial plexus, typically from C5 to C6 and occasionally C4. It innervates the supraspinatus and infraspinatus muscles and supplies sensory input to the acromioclavicular and glenohumeral joints through superior and inferior articular branches [1,2]. Passing through the suprascapular and spinoglenoid notches, the SSN is vulnerable to compression [1,3]. Cystic lesions are a recognized cause of SSN compression. Paralabral cysts, usually secondary to labral tears or capsular defects, contain synovial fluid and form adjacent to the joint. They are very common [3]. Intraneural ganglion cysts share similar fluid content but develop within the epineurium, with fluid tracking along the articular branch into the nerve [3,4]. On magnetic resonance imaging (MRI), they appear as elongated tubular intraneural structures [3,4]. Most occur in the common peroneal nerve, but other sites include the ulnar, median, radial, superficial radial, posterior interosseous, digital nerves, and the brachial plexus [5,6,7]. Suprascapular involvement is rare but can cause neuropathy leading to shoulder pain and dysfunction [3,4]. We report a rare intraneural ganglion cyst of the SSN with documented progression under conservative management, resulting in simultaneous compression at the suprascapular and spinoglenoid notches. This case also showed differing recovery between the supraspinatus and infraspinatus branches. The findings support Spinner’s articular theory [4,6,8] and highlight the need for early recognition and targeted surgical intervention.
A 63-year-old right-handed woman with no relevant medical history presented with a 6-month history of continuous dull right shoulder pain, aggravated by lying on the affected side and associated with nocturnal pain. She reported functional limitations in overhead activities. Analgesics included paracetamol, ibuprofen, and topical diclofenac. Her regular physical activities included walking and cycling. Examination showed normal biceps and triceps reflexes, intact sensation, negative Spurling’s test, and preserved cervical and cervicodorsal mobility with negative facet joint and foraminal compression tests. Increased tone was noted in the postural muscles, mainly in the upper trapezius. Shoulder assessment revealed painless passive external rotation and abduction-external rotation, but active external rotation strength was reduced to 4/5 on the Medical Research Council scale. Impingement signs and Jobe’s test were negative. Palpation over the suprascapular notch elicited tenderness. Ultrasound revealed a cystic lesion posterior to the glenoid. Arthro-MRI confirmed a cyst from the spinoglenoid to the suprascapular notch along the course of the SSN. No teres minor atrophy was observed. Additional findings included insertional tendinopathy of the supraspinatus and a superoposterior labral tear. The imaging appearance was consistent with an intraneural ganglion cyst. Electromyography (EMG) showed a right SSN lesion at or proximal to the supraspinatus muscle branch, consistent with a partial axonotmesis and associated with moderate-to-severe muscular involvement. The patient initially opted for a conservative approach with physiotherapy, ultrasound-guided aspiration, and intralesional glucocorticoid injection for symptomatic relief (Depo-Medrol 80 mg). Aspiration of the cyst was attempted. However, only 1 mL of the thick mucinous fluid could be retrieved. At 4 weeks, pain improved but there was persistent fatigue with overhead activity and weakness in both the supraspinatus and infraspinatus. Ultrasound showed a persistent anechoic, lobulated cyst (9.4 × 7.6 mm) in the suprascapular notch, with extension to the spinoglenoid (4.1 × 7.4 mm) notch, without hyperemia. Physiotherapy was continued, with follow-up planned in 2 months. Two months later, ultrasound showed an enlargement at the suprascapular notch (11.4 × 9.3 mm) and stable size at the spinoglenoid notch (4.0 × 7.3 mm). EMG revealed improved compound muscle action potential (CMAP) amplitude and recruitment in the supraspinatus, but decreased recruitment and denervation in the infraspinatus. A surgical indication was made for arthroscopic decompression of the cyst at both the suprascapular and spinoglenoid notches and treatment of the labral tear. Arthroscopy revealed a degenerative type IIB superior labrum anterior to posterior (SLAP) lesion, treated with biceps tenotomy and labral debridement, as repair was deemed infeasible. Cyst decompression exposed a well-defined synovial cyst wall surrounding the nerve. Incision released a wine-red mucinous fluid, and the wall was carefully debrided to achieve complete decompression (Fig. 1)
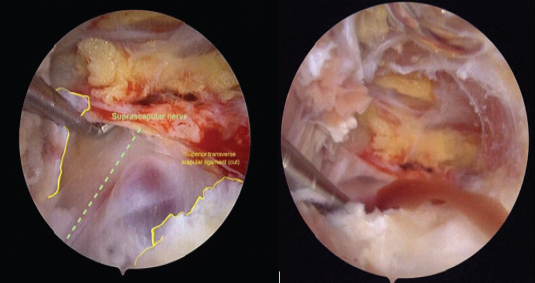
Figure 1 Arthroscopic view before and after incision.
(Additional file 1: Arthroscopic_Decompression_Suprascapular_Cyst.mp4). Additional acromioplasty addressed the insertional supraspinatus tendinopathy. Postoperatively, an adduction sling was applied for comfort for 2 weeks with immediate passive and active assisted mobilization after 3 weeks, followed by progressive strengthening from week 5. At 5 weeks postoperatively, the patient regained full range of motion and early external rotation strength improvement. Physiotherapy continued. At 3 months postoperatively, improvement was evident on anamnestic, clinical, and electromyographic assessment. External rotation strength had further increased, and the patient now reported only exertion-related discomfort. The EMG demonstrated recovery of the partial axonotmesis. The CMAP amplitude increased from 3.9 to 5.2 mV, and a significant increase in recruitment was observed in the infraspinatus muscle. Continued improvement is anticipated. Physiotherapy will be maintained, and a follow-up evaluation is scheduled for 6 months postoperatively.
An intraneural ganglion cyst is a mucin-filled lesion within the epineurium, enclosed by a fibrous wall, that causes neuropathy through fascicular compression [9]. Several pathogenetic mechanisms have been proposed. The intraneural theory attributes cyst formation to repetitive microtrauma and subsequent mucoid degeneration of fibrous tissue [7]. However, the most widely accepted explanation is Spinner’s articular theory, in which a capsulolabral tear permits joint fluid to track along the articular branch into the nerve, with dynamic joint pressures influencing cyst size and extension [3,4,6,8]. Cross-over into adjacent nerves may occur through a shared epineural sheath [4,6]. Our case supports this mechanism: the cyst arose from a capsulolabral tear. Arthro-MRI confirmed a SLAP lesion, with joint fluid tracking along the articular branch to the suprascapular notch, causing suprascapular neuropathy. Both supraspinatus and infraspinatus were affected, the latter more severely. Supraspinatus dysfunction likely limited overhead activity, while infraspinatus weakness reduced external rotation strength. Sensation was intact bilaterally, consistent with the SSN’s lack of a cutaneous branch [1]. Imaging showed no atrophy, but EMG demonstrated active denervation; follow-up EMG revealed improved supraspinatus recruitment and CMAP amplitude, with severe decreased recruitment and denervation in infraspinatus muscle. Three potential propagation patterns can be considered: (1) two independent primary cysts originating from the superior and inferior branches, (2) a primary cyst arising from the superior branch with distal cross-over into the infraspinatus branch, or (3) a primary cyst from the inferior branch with proximal ascent and cross-over to the supraspinatus branch (Fig. 2).
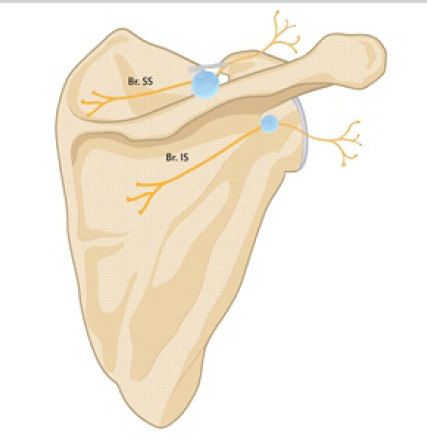
Figure 2: Dual-site compression of the suprascapular nerve. This figure illustrates the dual-site compression caused by a suprascapular intraneural ganglion cyst at the suprascapular and spinoglenoid notches. The most likely hypothesis is that a primary cyst was formed at the spinoglenoid notch due to mucinous fluid traveling along the inferior articular branch. Proximal ascent and cross-over to the supraspinatus branch subsequently led to the formation of a secondary cyst at the suprascapular notch. Br. SA: Superior articular branch, Br. IA: Inferior articular branch, Br. SS: Branch to the supraspinatus, Br. IS: Branch to the infraspinatus.
Based on previously described propagation models [4,6], the third hypothesis appears most consistent – representing a primary articular connection at the spinoglenoid notch with proximal intraneural extension and cross-over within the upper trunk. It is conceivable that following needle aspiration, transient pressure changes within the cyst may have facilitated further fluid migration along this inferior pathway. Moreover, the persistent lack of reinnervation in the infraspinatus branch could indicate that the inferior branch served as a principal site of fluid influx and pressure propagation, thereby sustaining localized fascicular injury and delayed recovery.
In this case, the intraneural ganglion cyst was confirmed by ultrasound (Fig. 3) and arthro-MRI (Fig. 4). It is important to distinguish such lesions from paralabral and extraneural ganglion cysts, cystic schwannomas, and nerve abscesses related to Hansen’s disease [9]. High-resolution MRI, ideally with intra-articular gadolinium, is recommended to detect a capsulolabral tear and MRI is the preferred method for detecting intraneural ganglion cysts [10,11]. On MRI, intraneural ganglion cysts typically appear as multilobulated, elongated, T2-hyperintense lesions along the nerve. Characteristic signs include the tail sign (extension along the articular branch), ascending limb (proximal spread), transverse limb (cross-over to an adjacent nerve), U sign (reverse propagation), and signet ring sign (fascicular compression) [9].
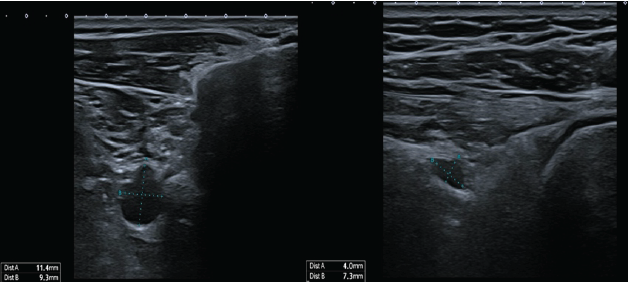
Figure 3: Ultrasound demonstrated a persistent anechoic, multilobulated cyst measuring 9.4 × 7.6 mm at the suprascapular notch, with a distal lobular extension measuring 4.1 × 7.4 mm towards the spinoglenoid notch.

Figure 4: Magnetic resonance imaging cystic formation in the suprascapular notch (left), spinoglenoid notch (middle), and tubular connection between both.
Sometimes, joint connections may be too small to visualize on imaging or obscured by surrounding anatomy, which can raise doubts about the articular theory. However, they are often identified on re-evaluation of pre-operative MRI or on post-operative imaging [8,10].
Historically, intraneural ganglion cysts were managed with open cyst decompression and articular branch resection [3]. However, this approach does not address the underlying capsulolabral tear and carries a significant risk of recurrence [3,8]. Moreover, decompression is not always necessary, as Prasad et al. reported that repair of the capsulolabral tear alone is often sufficient, with the cyst typically resolving spontaneously [3]. Early decompression, however, may provide rapid pain relief and prevent irreversible nerve damage, although recovery is limited once muscle atrophy has developed [7]. Arthroscopic management is now preferred, as it improves pain, strength, and function with low complication rates [12]. In summary, primary treatment should focus on arthroscopic repair of the capsulolabral tear, with optional articular branch resection to reduce recurrence and cyst decompression reserved for symptomatic relief [3]. Our patient initially chose conservative management, but the cyst enlarged due to persistent joint fluid leakage. EMG showed supraspinatus recovery with progressive infraspinatus denervation, prompting arthroscopic cyst decompression and labral debridement. The articular branch was preserved. Postoperatively, EMG demonstrated recovery of both the supraspinatus and infraspinatus muscles, indicating resolution of the previously asymmetric reinnervation pattern. This underscores the importance of EMG and imaging follow-up to guide timely intervention and thus prevent irreversible nerve damage. Our case is unique and worth reporting as it demonstrates cyst enlargement when the underlying cause is untreated, resulting in rare dual-site compression at the suprascapular and spinoglenoid notches. It also highlights asymmetric nerve recovery – partial in the supraspinatus branch with persistent infraspinatus denervation – and provides clinical, imaging, and surgical evidence supporting Spinner’s articular theory over the intraneural (mucoid degeneration) theory [4,6,7,8].
Intraneural ganglion cysts of the SSN may progress if the underlying joint pathology is untreated. This case shows that conservative management without addressing the causative labral tear can result in cyst enlargement, multi-site compression, and uneven recovery of the affected muscles. Early identification of the joint connection and timely surgery are essential to prevent irreversible nerve damage. Serial EMG and imaging help monitor progression, guide treatment, and assess recovery.
Intraneural ganglion cysts of the SSN should be recognized on imaging as a cause of neuropathy. Conservative management such as aspiration does not address the underlying labral tear and risks recurrence or progression with possible dual-site compression. Early arthroscopic labral repair, with or without articular branch resection, is essential to prevent progression/recurrence, while decompression may provide relief but carries risk of iatrogenic injury.
References
- 1. Basta M, Sanganeria T, Varacallo MA. Anatomy, Shoulder and Upper Limb, Suprascapular Nerve. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://pubmed.ncbi.nlm.nih.gov/32491803 [Last accessed on 2025 Jul 05]. [Google Scholar] [PubMed]
- 2. Terra BB, Gaspar EF, Siqueira KL, Filho NS, Monteiro GC, Andreoli CV, et al. Anatomical relationship of the suprascapular nerve to the coracoid process, acromioclavicular joint and acromion. Rev Bras Ortop 2015;45:269-72. [Google Scholar] [PubMed]
- 3. Prasad NK, Spinner RJ, Smith J, Howe BM, Amrami KK, Iannotti JP, et al. The successful arthroscopic treatment of suprascapular intraneural ganglion cysts. Neurosurg Focus 2015;39:E11. [Google Scholar] [PubMed]
- 4. Spinner RJ, Amrami KK, Wang H, Kliot M, Carmichael SW. Cross-over: A generalizable phenomenon necessary for secondary intraneural ganglion cyst formation. Clin Anat 2008;21:111-8. [Google Scholar] [PubMed]
- 5. Pemmari A, Mäkelä K, Niemi J, Kiekara T, Himanen SL. Large intraneural ganglion cyst in the peroneal nerve. Case Rep Neurol 2022;14:44-50. [Google Scholar] [PubMed]
- 6. Spinner RJ, Hébert-Blouin MN, Dahm DL, Amrami KK. Two different pathways for suprascapular intraneural ganglion cysts along two distinct articular branches from the glenohumeral joint. Clin Anat 2010;23:462-5. [Google Scholar] [PubMed]
- 7. Sanger J, Cortes W, Yan JG. Intraneural ganglion of the suprascapular nerve: Case report. J Hand Surg Am 2006;31:40-4. [Google Scholar] [PubMed]
- 8. Desy NM, Wang H, Elshiekh MA, Tanaka S, Choi TW, Howe BM, et al. Intraneural ganglion cysts: A systematic review and reinterpretation of the world’s literature. J Neurosurg 2016;125: 615-30. [Google Scholar] [PubMed]
- 9. Panwar J, Mathew A, Thomas BP. Cystic lesions of peripheral nerves: Are we missing the diagnosis of the intraneural ganglion cyst? World J Radiol 2017;9:230-44. [Google Scholar] [PubMed]
- 10. Spinner RJ, Amrami KK. Intraneural ganglion of the suprascapular nerve: Case report. J Hand Surg Am 2006;31:1698-9. [Google Scholar] [PubMed]
- 11. Lenartowicz KA, Wolf AS, Desy NM, Strakowski JA, Amrami KK, Spinner RJ. Preoperative imaging of intraneural ganglion cysts: A critical systematic analysis of the world literature. World Neurosurg 2022;166:e968-79. [Google Scholar] [PubMed]
- 12. Memon M, Kay J, Ginsberg L, Simunovic N, Bak K, Lapner P, et al. Arthroscopic management of suprascapular neuropathy of the shoulder improves pain and functional outcomes with minimal complication rates. Knee Surg Sports Traumatol Arthrosc 2018;26:240-66. [Google Scholar] [PubMed]