Suprapatellar intramedullary nailing with condylar screw augmentation is a minimally invasive technique that offers stable fixation and enables early mobilization in complex proximal tibia fractures.
Dr. R S Boobathi Raja, Department of Trauma Surgery, Soundarapandian Bone and Joint Hospital and Research Institute, Chennai, Tamil Nadu, India. E-mail: boobathirajars@gmail.com
Introduction: Complex intra-articular proximal tibia fractures (Schatzker types V and VI) are difficult to manage due to articular involvement, malalignment, and soft-tissue compromise. Conventional plating techniques carry risks of infection and soft-tissue morbidity. Suprapatellar intramedullary nailing (IMN), combined with condylar screws, offers a minimally invasive option with potential biomechanical and clinical advantages.
Materials and Methods: A prospective case series was conducted at a tertiary trauma center in Chennai, India, including 10 consecutive adults with Schatzker type V (n = 6) and VI (n = 4) fractures. All patients underwent Suprapatellar IMN in the semi-extended position, reinforced with two lateral-to-medial condylar screws. Patients were followed for 12 months. Radiological union, fracture alignment, and complications were documented. Functional recovery was assessed using the lower extremity functional scale (LEFS) and knee range of motion (ROM). Results: The mean patient age was 46.9 years (range 29–73), with 8 males and 2 females. The mean operative time was 104.3 ± 14.2 min. All fractures united radiologically at a mean of 14.3 ± 1.8 weeks. At 12 months, the mean LEFS score was 66.6 ± 7.5; 70% of patients achieved minimal limitation (LEFS ≥64). The mean knee ROM was 125° ± 7.8°. No cases of infection, non-union, implant failure, or neurovascular injury were recorded.
Conclusion: Suprapatellar IMN supplemented with condylar screws appears to be a reliable minimally invasive technique for complex proximal tibia fractures, allowing stable fixation, early mobilization, and good functional outcomes. Larger studies are warranted to validate these findings.
Keywords: Proximal tibia fracture, tibial plateau fracture, Schatzker V–VI, suprapatellar intramedullary nailing, condylar screws, minimally invasive fixation.
Complex intra-articular proximal tibia fractures (Schatzker types V and VI) involve both tibial condyles and are among the most difficult fractures to treat [1,2]. Conventional strategies such as plating – either open reduction or minimally invasive – or external fixation have all been used, yet clinical outcomes are often unpredictable [3,4]. Open plating facilitates direct visualization and anatomical reduction, but carries risks of instability, infection, and delayed union [5]. Angled plate constructs may improve stability but are more invasive and may compromise soft tissues [6]. Minimally invasive plate fixation reduces dissection but may complicate accurate alignment [7]. Intramedullary nailing (IMN) has emerged as a viable alternative, particularly for lowering infection rates and soft-tissue problems, though malalignment remains a concern [8]. To address these issues, newer implant designs and surgical techniques have been developed [9]. One such approach is suprapatellar IMN augmented with condylar screws, combining the mechanical stability of nailing with articular surface support [10]. This report describes the clinical and radiological results of this method in a series of complex tibial fractures.
Study design and setting
This prospective case series was conducted in the department of orthopedics at a tertiary care bone and joint hospital in Chennai. A total of 10 patients were enrolled sequentially between October 2023 and July 2024. Each patient was followed for 12 months from the date of enrolment, with the 12-month follow-up for the last patient completed in July 2025.
Patient selection
Consecutive skeletally mature patients (>18 years) with radiologically confirmed Schatzker types V or VI proximal tibia fractures presenting within 24 h of injury were included.
Inclusion criteria
Closed fractures, fit for surgery, and a willingness to participate in follow-up.
Exclusion criteria
Open or pathological fractures, polytrauma requiring staged fixation, impending compartment syndrome, and delayed presentation (>24 h).
Surgical technique
All procedures were performed by the senior trauma team using a standardized protocol.
- Position: Supine with knee in 20° flexion (semi-extended)
- Approach: Suprapatellar portal established using a trocar through the quadriceps tendon
- Reduction: Fracture alignment and articular elevation achieved under fluoroscopic guidance
- Fixation: Two lateral-to-medial condylar screws inserted 0.5–1 cm below the joint surface, followed by intramedullary nail insertion with proximal and distal locking screws
- Post-operative care: Immediate active knee mobilization as tolerated; non-weight-bearing for 6 weeks, followed by partial and then full weight-bearing by 2–3 months.
Follow-up and outcome measures
Patients were reviewed at 1, 3, 6, 9, and 12 months.
Radiological outcomes
Union (bridging callus across 3 cortices) and alignment on AP, lateral, and long-leg standing radiographs.
Functional outcomes
Lower Extremity Functional Scale (LEFS) at 12 months, and knee range of motion (ROM).
Complications
Infection, implant failure, malunion, non-union, and neurovascular injury.
Data analysis
Descriptive statistics (mean, standard deviation, and range) were used to summarize patient demographics and outcomes. Given the small sample size, inferential analysis was not performed. Data were analyzed using Statistical Package for the Social Sciences version 26.0 (IBM, USA).
A total of 10 patients were included in this prospective case series, of whom 80% were male, and 20% were female, with an average age of 46.9 years (range: 29, 73). The right lower limb was involved in 60% cases on the right side, while 40% patients had fractures on the left side. Based on the Schatzker classification, Type V fractures were observed in 6 patients (60%), while Type VI fractures were present in 4 patients (40%). The mean operative time was 104.3 ± 14.27 min (range: 85–118 min). No intraoperative complications were noted, and there were no cases of non-union, neurovascular injury, revision surgery, or need for plating. All fractures achieved both clinical and radiographic union at a mean of 14.3 ± 1.81 weeks (range: 10–18 weeks) postoperatively. Restoration of the articular surface and tibial alignment was assessed using post-operative anteroposterior and lateral knee radiographs, along with full-length standing views. At the latest follow-up, the mean knee range of motion was 125° ± 7.81° (115, 145) The mean LEFS score was 66.6 ± 7.5, with scores ranging from 53 to 75. The median score was 68, indicating overall good lower limb functional recovery. Most patients (7 out of 10) achieved LEFS scores of ≥64, which corresponds to mild or minimal functional limitation. Only two patients scored below 60, suggesting moderate difficulty in some activities of daily living. All the above results are explained in Table 1. Representative pre-operative, intra-operative, and post-operative images are shown in Fig. 1-5.
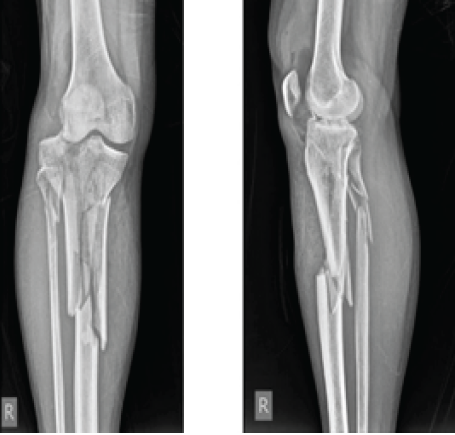
Figure 1: Anteroposterior and lateral view of X-ray showing Type 6 tibial plateau fracture with metaphyseal diaphyseal disassociation.
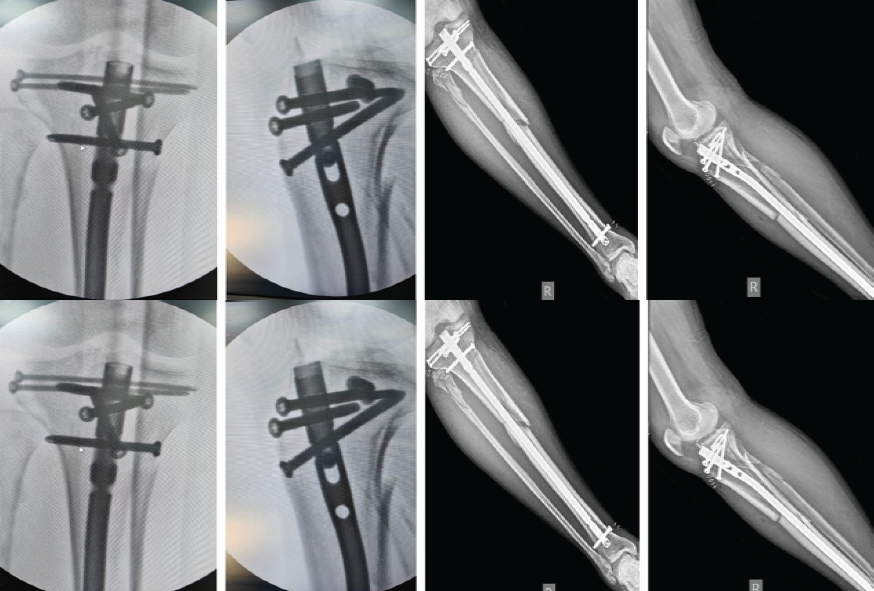
Figure 2: Image showing staple 5 locking screw fixation for proximal fragments. Immediate Postoperative X-ray.

Figure 3: 6th month follow-up X-ray.
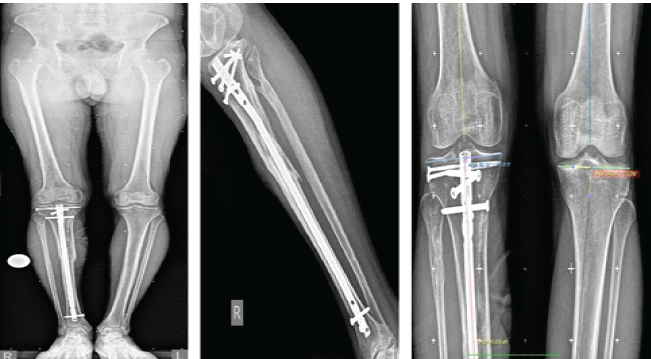
Figure 4: Long leg standing view at 12 months shows well-aligned fracture fixation with preserved medial joint space.
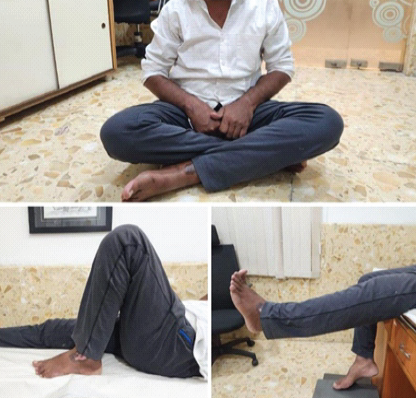
Figure 5: At 12-month follow-up, the patient demonstrates full range of motion.
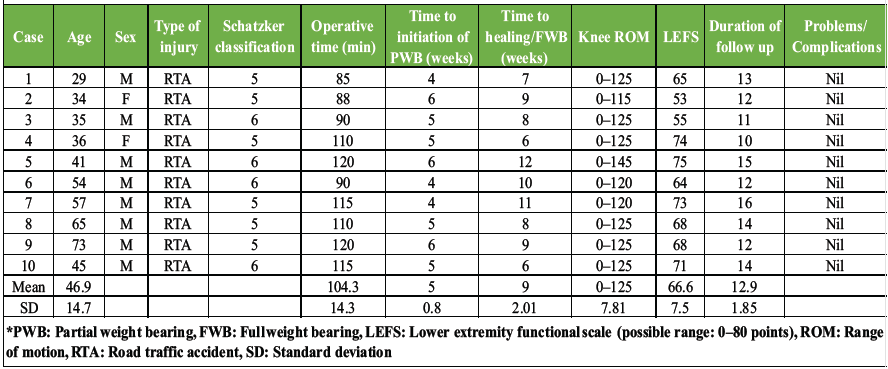
Table 1: Demographic data and results
Management of complex intra-articular proximal tibia fractures (Schatzker V and VI) remains a surgical challenge due to bicondylar involvement, articular depression, and risk of malalignment. Conventional strategies such as dual plating and minimally invasive plate osteosynthesis allow restoration of articular anatomy but are associated with soft-tissue complications, infection, and delayed rehabilitation [11,12]. External fixation, although less invasive, often fails to maintain reduction in osteoporotic bone and can interfere with mobilization, [13,14]. Intramedullary nailing has gained attention as a less invasive option with lower infection risk, but traditional infrapatellar entry is technically demanding in proximal fractures and carries a risk of malreduction. The Suprapatellar approach, performed in a semi-extended position, helps to neutralize the anterior pull of the quadriceps and facilitates accurate alignment under fluoroscopy [15]. Augmentation with condylar screws provides additional support to the articular surface, enhancing construct stability. In our series, Suprapatellar IMN supplemented with condylar screws achieved reliable union with good functional recovery and no major complications. The mean LEFS scores and knee range of motion at final follow-up were comparable to or better than reported outcomes with plating techniques. Early knee mobilization was possible in all patients, supporting the functional advantage of this minimally invasive approach. The strengths of this series include the prospective design, standardized surgical protocol, and consistent follow-up. However, limitations include the small sample size, absence of a control group, and reliance on radiographs for alignment assessment. These results should therefore be interpreted as preliminary evidence. Larger comparative studies are necessary to confirm the long-term benefits of this technique.
Suprapatellar intramedullary nailing with condylar screw augmentation is a reliable technique for complex proximal tibia fractures, offering stable fixation, minimal soft-tissue disruption, and encouraging early mobilization. While our findings suggest good functional outcomes, larger comparative studies are required to validate their wider applicability.
Suprapatellar intramedullary nailing supplemented with condylar screws provides a stable, minimally invasive option for managing complex proximal tibia fractures, enabling early mobilization and good functional recovery.
References
- 1. Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium – 2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 2007;21 10 Suppl:S1-133. [Google Scholar] [PubMed]
- 2. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The toronto experience 1968–1975. Clin Orthop Relat Res 1979;138:94-104. [Google Scholar] [PubMed]
- 3. Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury 2006;37:475-84. [Google Scholar] [PubMed]
- 4. Mahadeva D, Costa ML, Gaffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: A systematic review of the literature. Arch Orthop Trauma Surg 2008;128:1169-75. [Google Scholar] [PubMed]
- 5. Oh JK, Sahu D, Hwang JH, Cho JW, Oh CW. Technical pitfall while reducing the mismatch between LCP PLT and upper end tibia in proximal tibia fractures. Arch Orthop Trauma Surg 2010;130:759-63. [Google Scholar] [PubMed]
- 6. Ryan SP, Tornetta P 3rd, Dielwart C, Kaye-Krall E. Knee pain correlates with union after tibial nailing. J Orthop Trauma 2011;25:731-5. [Google Scholar] [PubMed]
- 7. Sanders RW, DiPasquale TG, Jordan CJ, Arrington JA, Sagi HC. Semiextended intramedullary nailing of the tibia using a Suprapatellar approach: Radiographic results and clinical outcomes at a minimum of 12 months follow-up. J Orthop Trauma 2014;28:245-55. [Google Scholar] [PubMed]
- 8. Ricci WM, O’Boyle M, Borrelli J, Bellabarba C, Sanders R. One-third of the tibial shaft treated with cantilever nails and locking screws. J Orthop Trauma 2019;15:264-70. [Google Scholar] [PubMed]
- 9. Garnavos C, Lasanianos NG. The management of complex fractures of the proximal tibia with minimal intra-articular impaction in fragility patients using intramedullary nailing and compression bolts. Injury 2011;42:1066-72. [Google Scholar] [PubMed]
- 10. Lasanianos NG, Garnavos C, Magnisalis E, Kourkoulis S, Babis GC. A comparative biomechanical study for complex tibial plateau fractures: Nailing and compression bolts versus modern and traditional plating. Injury 2013;44:1333-9. [Google Scholar] [PubMed]
- 11. Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev 1994;23:149-54. [Google Scholar] [PubMed]
- 12. Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma 2004;18:649-57. [Google Scholar] [PubMed]
- 13. Mallik AR, Covall DJ, Whitelaw GP. Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev 1992;21:1433-6. [Google Scholar] [PubMed]
- 14. Ali AM, Burton M, Hashmi M, Saleh M. Treatment of displaced bicondylar tibial plateau fractures (OTA-41C2&3) in patients older than 60 years of age. J Orthop Trauma 2003;17:346-52. [Google Scholar] [PubMed]
- 15. Bhandari M, Audige L, Ellis T, Hanson B, Evidence-Based Orthopaedic Trauma Working Group. Operative treatment of extra-articular proximal tibial fractures. J Orthop Trauma 2003;17:591-5. [Google Scholar] [PubMed]








