Intra-articular corrective osteotomy is an effective surgical option to restore joint congruency and function in symptomatic malunited Bennett’s fractures when degenerative changes have not yet developed.
Dr. V S Kiran Raju, Institute of Orthopaedics, AIG Hospitals, Hyderabad, Telangana, India. E-mail: vatsavaisatyakiran@gmail.com
Introduction: Bennett’s fracture is an intra-articular fracture-dislocation at the base of the first metacarpal. If inadequately treated, it may lead to malunion and subluxation of the carpometacarpal joint, resulting in pain, stiffness, and functional impairment.
Case Report: We report the case of a 28-year-old male software professional who presented 7 months after sustaining a left thumb injury with persistent pain, stiffness, and difficulty in thumb use. Radiographs revealed a malunited intra-articular fracture of the first metacarpal base with joint subluxation. The patient underwent intra-articular corrective osteotomy with fixation using screws and a trans-articular K-wire to restore joint congruity. At 12 weeks, he achieved full, pain-free thumb movements, and at 10 months, radiographs confirmed fracture union with a Kapandji score of 10/10.
Conclusion: Intra-articular corrective osteotomy is a viable and effective treatment for symptomatic Bennett’s fracture malunion, particularly when performed before the onset of degenerative changes, leading to excellent pain relief and restoration of thumb function.
Keywords: Bennett’s fracture, malunion, intra-articular osteotomy, thumb carpometacarpal joint, corrective surgery.
Bennett’s fracture is an intra-articular fracture-dislocation of the base of the first metacarpal, involving the carpometacarpal (CMC) joint of the thumb. It is a relatively common injury, accounting for 10–20% of all thumb fractures [1]. The mechanism of injury typically involves an axial force applied to a partially flexed thumb, such as during a fall or direct trauma, leading to subluxation or dislocation of the first metacarpal base over the trapezium. Closed reduction and percutaneous pinning are widely accepted treatment options for this fracture [2]. If not treated properly, there is a significant risk of malunion and instability of the basal joint, which can result in decreased range of motion in the thumb, reduced grip, pinch strength, and chronic pain leading to arthritis [3].
We report a case of 28-year-old male who presented to the outpatient department with complaints of left thumb pain for the past 7 months. He had a history of a road traffic accident 7 months ago. He went to an orthopedic surgeon and got treated with a removable Thumb Spica splint for 2 months. He was not on any physiotherapy after the splint removal. Due to prolonged immobilization patient developed stiffness and pain on attempted thumb movements, but no rest pain. Clinically, there was tenderness over the base of the first metacarpal and along the basal joint line. The joint appears to be subluxed. He was unable to perform active thumb movements, passive movements were painful secondary to stiffness, and the joint was subluxated on palpation. He was not able to perform activities such as typing, holding a bottle of water, difficulty in picking up things with a pinch grip, and significantly impaired activities of daily living involving thumb function.
Investigations
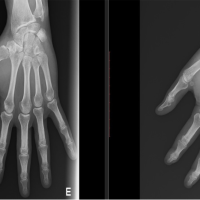
Radiographs revealed a healed fracture at the base of the first metacarpal, which was malunited, and the metacarpal was hinging over the underlying trapezium (Fig. 1a and b). Stress views were not obtained.
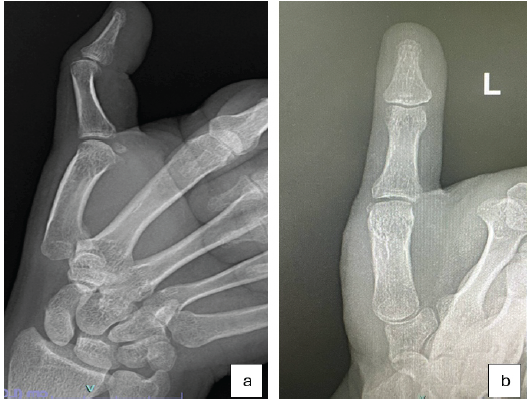
Figure 1: (a and b) showing the plain radiographs of base of first metacarpal anteroposterior and lateral views.
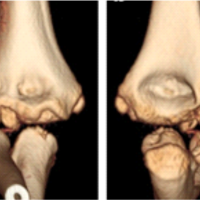
Computed tomography with 3D reconstruction showed a displaced intra-articular fracture at base of the first metacarpal involving volar, ulnar aspects of the bone, consistent with Bennett’s fracture attached to the beak ligament, with proximally and laterally migrated distal metacarpal fragment (Fig. 2a and b).
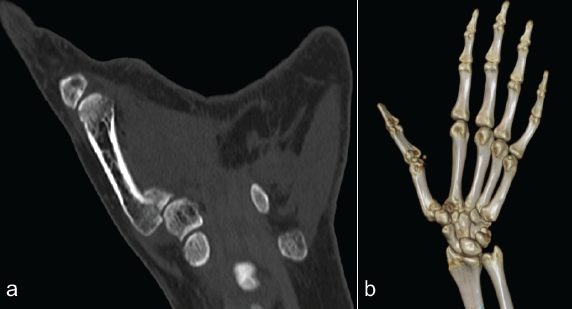
Figure 2: (a and b) showing the pre-operative computed tomography images of the malunited base of first metacarpal.
We had planned to correct the intra-articular step deformity of the malunion and correct subluxation to achieve a congruent joint.
Technique
Surgery was performed under regional anesthesia with the patient in a supine position, with the left upper limb placed on an arm table. Intravenous antibiotic (injection cefuroxime 1.5 gm) was administered half an hour before tourniquet inflation. Standard preparation and draping were done. A Wagner’s incision centered over the CMC joint of the left thumb was made, and a plane was developed between the abductor pollicis longus and abductor pollicis brevis (APB). The APB and thenar muscles were raised from the joint capsule and metacarpal base. A T-shaped capsular incision was made to expose the base of the first metacarpal. Intra-articular malunion site was identified, revealing a step deformity. Osteotomy was performed at the malunion site under C-arm guidance using fine osteotomies, and the fracture was recreated. Subluxation of the metacarpal block was corrected, and the fragment was reduced anatomically (Fig. 3a, b, c).
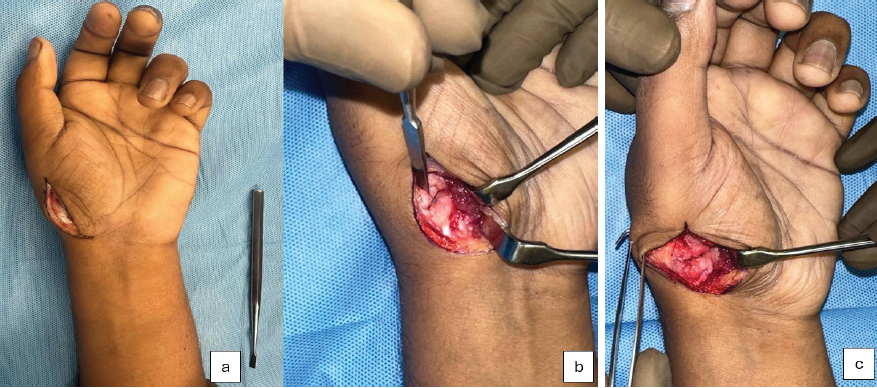
Figure 3: (a, b and c) showing intra-operative images of the incision, osteotomy.
Reduction of the articular surface and joint surfaces was confirmed under an image intensifier (II). Provisional fixation was achieved with a 1.2 mm K wire, and reduction was confirmed under II. Definitive fixation was achieved using mini fragment screws (Synthes 1.3 mm screws: 15 mm–01, 16 mm – 01). CMC joint reduction was stabilized with a transarticular K-wire. The joint capsule was closed. We cauterized the injured palmar cutaneous nerve branch supplying the joint capsule of the basal joint lying at the thenar origin (not a planned procedure). We did not perform a complete selective neurectomy of the basal joint. Thenar origin was resutured. Incision was closed in layers, followed by an antiseptic dressing. A thumb spica plaster slab was applied with a compression dressing. Tourniquet deflated at 72 min.
Rehabilitation
The thumb spica plaster slab was maintained for three weeks, followed by a removable thumb spica splint for an additional 3 weeks. After 6 weeks, K wire was removed, and the patient was encouraged to perform active movements of the thumb at the metacarpophalangeal and interphalangeal joints to restore mobility and function.
Outcome
At 12 weeks postoperatively, the patient achieved a full, pain-free range of motion in the thumb (Fig. 4). The functional Kapandji score was 7/10 at the 3-month follow-up, and 10/10 at the end of 10 months reflecting excellent thumb mobility, dexterity, and functional recovery (Fig. 5). The patient achieved good union at fracture site and a congruent joint on radiographs (Fig. 6).

Figure 4: Result at 3 months.
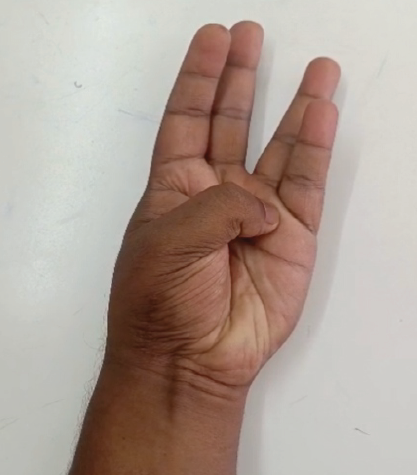
Figure 5: Result at 10 months.
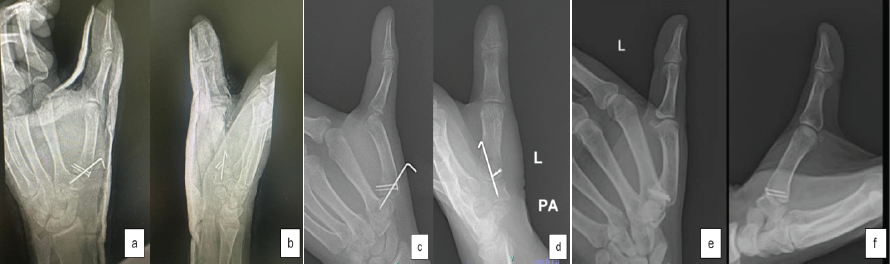
Figure 6: Post-operative radiographs. (a and b) immediate post operative radiographs. (c and d) radiographs at 6 weeks post operative. (e and f) radiographs at 10 months after the surgery.
Bennett’s fracture is a common injury, particularly in the dominant hand of males, often resulting from a direct blow with a clenched fist against a hard surface. Failure to recognize or achieve an anatomical reduction invariably results in chronic pain and stiffness, leading to the first CMC arthritis. The literature on malunited Bennett’s fractures remains sparse, with only a few case reports discussing the treatment options. Intra-articular osteotomy of malunited Bennett’s fracture was first described by Bunnell [2]. Vasko modified Bunnell’s technique using cotton suture for fixation of the osteotomized metacarpal fragment [4]. In 1950, Wagner proposed primary open arthrodesis of the first CMC joint for fractures that could not be anatomically reduced, prioritizing stability at the cost of mobility. However, this approach has been replaced by other reconstructive techniques [5]. Giachino reported a case in 1994 where intra-articular osteotomy and screw fixation of malunited Bennett’s fracture in a 30-year-old male yielded satisfactory outcomes over a 4-year follow-up [6]. Similarly, Jebson and Blair published a report on two cases of symptomatic malunited Bennet’s fractures, demonstrating good outcomes after 2 years with good pinch strength and weightlifting ability comparable to the opposite uninjured side [7]. Van Royen et al., also contributed a case report of intra-articular osteotomy for symptomatic Bennett’s fracture malunion, detailing the surgical technique for correction with good results [8]. The largest case series on malunited Bennett’s fracture was published in 2021 by Vergote and Mentzel in 24 patients (19 Bennett’s fractures, 3 Rolando fractures, and 2 Winterstein fractures). Corrective osteotomy and osteosynthesis were performed using screw or K-wires. Complete correction of articular step was achieved in 13 patients, while 6 patients had a residual intra-articular step of 0.5–2.2 mm, which was deemed acceptable. They concluded that posttraumatic malunion of the base of the first metacarpal can be treated effectively with corrective osteotomy, provided degenerative changes have not set in [9]. Alternative treatments, such as trapeziectomy (performed in two patients), remain viable options in selected chronic cases [10]. In our case, corrective osteotomy and internal fixation successfully restored joint congruency, leading to pain relief and improved thumb mobility and function.
Symptomatic malunion of Bennett’s fracture can significantly impact thumb function and quality of life. Cases of malunion may require surgical intervention to prevent long-term complications such as stiffness and arthritis. Our case adds to the growing body of literature supporting corrective osteotomy as a viable option for symptomatic malunited Bennett’s fractures, emphasizing the importance of early diagnosis and appropriate treatment to ensure optimal functional outcomes.
Symptomatic malunion of a Bennett’s fracture can severely impair thumb function due to pain, stiffness, and loss of motion. Early recognition and timely intra-articular corrective osteotomy can restore joint congruity, relieve pain, and regain optimal thumb mobility before degenerative changes occur. Careful preoperative planning and precise anatomical reduction are key to achieving excellent functional outcomes and preventing long-term arthritis.
References
- 1. Edmunds JO. Traumatic dislocations and instability of the trapeziometacarpal joint of the thumb. Hand Clin 2006;22:365-92. [Google Scholar] [PubMed]
- 2. Bunnell S. Surgery of the Hand. 3rd ed. United States: Mosby; 1972. [Google Scholar] [PubMed]
- 3. Goru P, Haque S, Verma GG, Mustafa A, Ebinesan A. Bennett’s fracture management: A systematic review of literature. Cureus 2022;14:e31340. [Google Scholar] [PubMed]
- 4. Vasco JR. An operation for old unreduced Bennett’s fracture. J Bone Joint Surg 1947;29:753-6. [Google Scholar] [PubMed]
- 5. Wagner CJ. Surgery of the first carpometacarpal joint: A study on arthrodesis for irreducible fractures. Am J Surg 1950;80:15-22. [Google Scholar] [PubMed]
- 6. Giachino AA. A surgical technique to treat a malunited symptomatic Bennett’s fracture. J Hand Surg Am 1996;21:149-51. [Google Scholar] [PubMed]
- 7. Jebson PJ, Blair WF. Correction of malunited Bennett’s fracture by intra-articular osteotomy: A report of two cases. J Hand Surg Am 1997;22:441-4. [Google Scholar] [PubMed]
- 8. Van Royen K, Vanmierlo B, Bonte F, Goorens CK, Berghs B, Goubau J. Intra-articular osteotomy for symptomatic Bennett fracture malunion. Tech Hand Up Extrem Surg 2019;23:138-142. [Google Scholar] [PubMed]
- 9. Vergote D, Mentzel M. Corrective Osteotomy of malunited fractures of the base of the first metacarpal bone. Handchir Mikrochir Plast Chir 2022;54:51-7. [Google Scholar] [PubMed]
- 10. Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011 Jan;36(1):157-69. doi: 10.1016/j.jhsa.2010.10.028. PMID: 21193136. [Google Scholar] [PubMed] [CrossRef]