Concomitant septic arthritis should be considered while treating patients with femoral head osteonecrosis having synovitis if they are on steroids or immunosuppressants.
Dr. James C George, Department of Orthopaedics, Aster DM Healthcare, Dubai, United Arab Emirates. Email: drjamescgeorge@gmail.com
Introduction: Concomitant femoral head osteonecrosis and hip joint septic arthritis is rare. Membranous nephropathy is an immune-mediated glomerular disease producing nephrotic syndrome in adults. Patients take glucocorticoids or immunosuppressants during treatment of this condition. We report the first case of a patient with nephrotic syndrome during treatment developing concomitant hip septic arthritis and femoral head osteonecrosis with an opportunistic pathogen seen in gastrointestinal tract.
Case Report: A 37-year-old gentleman on treatment with high-dose prednisolone and mycophenolate for nephrotic syndrome developed bilateral hip pain and was diagnosed as osteonecrosis of femoral head. He underwent core decompression of both hips. Suspected concomitant septic arthritis noted in the magnetic resonance imaging was considered as synovitis. After core decompressio Citrobacter species was aspirated from the left hip. This was then managed by debridement and antibiotics. Five years later, he developed secondary osteoarthritis with protrusio-acetabuli subsequent to septic sequelae and underwent total hip replacement without any reactivation till last follow-up.
Conclusion: Concomitant septic arthritis with femoral head osteonecrosis should be considered when treating patients on steroids or immunosuppressants. An elevated erythrocyte sedimentation rate and C-reactive protein in a patient with osteonecrosis warrants additional investigations, including ultrasound-guided aspiration and culture, before core decompression or any surgical intervention even in immunocompetent patients.
Keywords: Osteonecrosis, septic arthritis, citrobacter, glucocorticoids, membranous nephropathy, immunosuppression.
Membranous nephropathy is an immune-mediated glomerular disease producing nephrotic syndrome in adults. Steroids and immunosuppressants are the main line of treatment for this condition. These, patients are susceptible for developing complications secondary to both steroids and immunosuppression. Gram-negative bacilli account for to 20% of septic arthritis globally. Common pathogens include Escherichia coli, Proteus, Klebsiella, and Enterobacter. It most often affects neonates, intravenous drug abusers, and elderly immunocompromised people with diabetes. These organisms pose serious therapeutic problems because of the increasing incidence of multidrug resistance [1]. Citrobacter is a Gram-negative bacillus found commonly in the soil and also in the gastrointestinal tract of humans. It is a rare opportunistic pathogen infecting immunocompromised patients. There are no reported cases of septic arthritis of the hip caused by Citrobacter in the literature except for one case report on prosthetic hip joint infection in a diabetic, morbidly obese patient [2]. We report the first case of a patient with nephrotic syndrome during treatment with steroids and immunosuppressants developing concomitant hip septic arthritis and femoral head osteonecrosis with an opportunistic pathogen.
A 37-year-old gentleman diagnosed with primary membranous glomerulonephritis by renal biopsy developed bilateral hip pain in 2019. He was on treatment with 60 mg prednisolone per day along with 1 g mycophenolate twice a day for more than a year. He was afebrile, and his total white blood cell (WBC) count was also normal. He had elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) (Table 1).
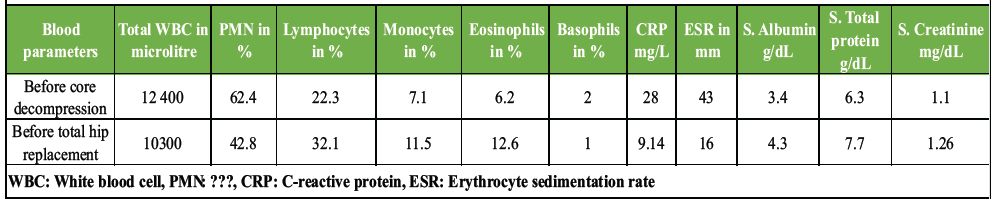
Table 1: Preoperative blood investigations before core decompression when the patient had septic arthritis and osteonecrosis, and 5 years later, before total hip replacement
His magnetic resonance imaging of the hip showed Ficat Stage 2b osteonecrosis on both sides, along with synovitis and suspected septic arthritis of the left hip (Fig. 1).
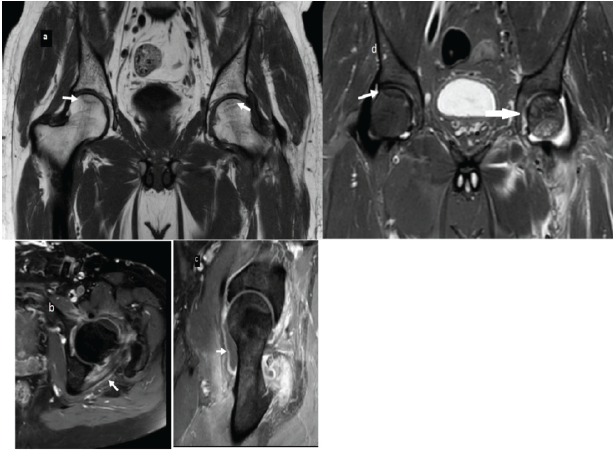
Figure 1: (a) T1WI coronal image showing bilateral femoral head osteonecrosis with arrows indicating bilateral subchondral fracture lines. (b) Axial post contrast T1WI showing left hip septic arthritis (c) Septic arthritis left hip joint (d) Coronal short tau inversion recovery image showing right femoral head Double line sign (bright and dark lines) in osteonecrosis and concomitant septic arthritis left side.
He underwent bilateral core decompression of hip joints, ignoring the possibility of concomitant septic arthritis. Postoperatively, he developed an increase in pain of the left hip. Ultrasound-guided aspiration was done and pus from the hip joint grew Citrobacter species sensitive to piperacillin, tazobactum, meropenem, quinolones, and cefixime. He underwent debridement, and intraoperative culture also grew the same organism (Table 2). He was treated with Meropenem 1.5 g thrice daily for 7 days, and his infection settled with normalization of CRP.
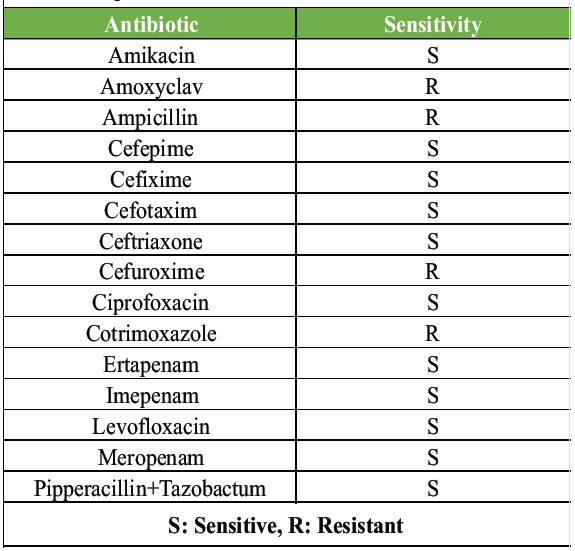
Table 2: Culture and sensitivity report of Citrobacter species isolated intraoperatively during debridement and ultrasound-guided aspiration of the left hip after bilateral core decompression
He continued to have mild pain in the left hip, which gradually progressed over the next 5 years. He did not have any reactivation of infection for 5 years. He was on tacrolimus for his nephropathy, the dose being adjusted as per his disease activity until he attained remission. By 2025, he was unable to bear weight and walk and also noticed progressive shortening of the left lower limb. He had a flexion deformity of 20°. All other movements were limited to 20° range but were intact. His X-ray showed destruction of the femoral head with Grade 2 Protrusio acetabulii (Fig. 2).
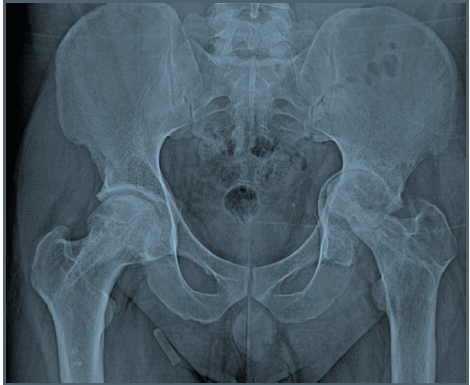
Figure 2: Left hip protrusio acetabuli Grade 2 with joint space narrowing, femoral head destruction, and arthritis.
His CRP was 9.1 g/L, and his WBC count was normal (Table 1). His creatinine was 1.26 mg/dL, albumin was 4.3 g/dL, and there was no proteinuria. Ultrasound of the hip did not show any fluid. After withholding tacrolimus for a week, he underwent uncemented total hip replacement (Fig. 3) under the cover of piperacillin and tazobactum 4.5 g thrice daily.
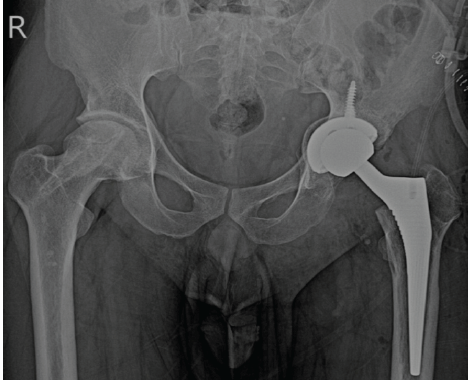
Figure 3: Left uncemented total hip replacement status.
The femoral head was found to be partially destroyed (Fig. 4), and the acetabulum was devoid of any cartilage.
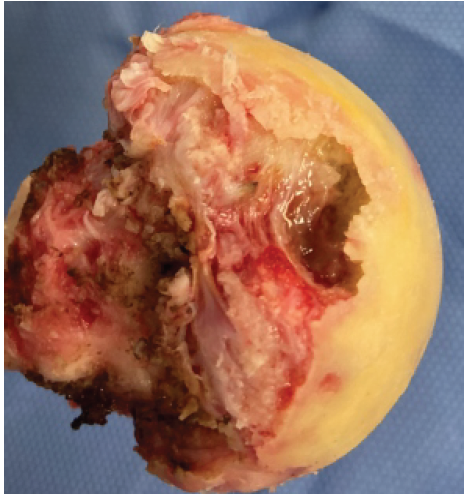
Figure 4: Destruction of the femoral head by infection and osteonecrosis with associated synovitis.
Significant synovitis and granulation tissue noted during surgery were meticulously debrided. Tissues were sent for aerobic and anaerobic culture, mycobacterium, fungus, and histopathology (Table 3).
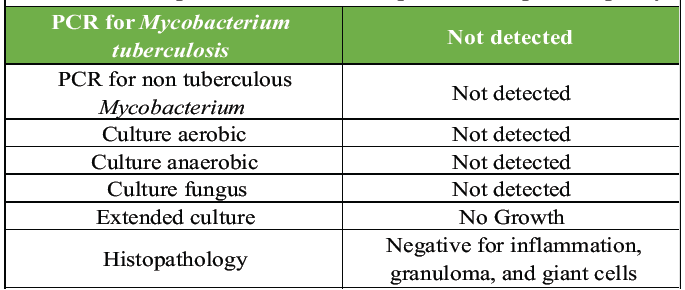
Table 3: Investigations carried out from the tissues from acetabulum and proximal femur during left total hip arthroplasty
Antibiotics were continued for 72 h intravenously until culture reports were ready. Oral dual antibiotics were given (cefixime 400 mg daily and levofloxacin 750 mg daily) for 2 weeks until the extended cultures were negative for any organism. Postoperatively, there was no reactivation of infection. Harris hip score improved from 29 preoperatively to 81 at 6 months post-surgery.
In a study of 326 patients with gram-negative bacteremia, comorbid conditions were identified in 315 (97%) [3]. The conditions reported are hematopoietic stem cell transplant, liver failure, serum albumin <3 g/dL, solid organ transplant, diabetes, pulmonary disease, chronic hemodialysis, human immunodeficiency virus infection, and treatment with glucocorticoids and immunosuppression [4]. Conventionally, the majority of Gram-negative infections in the hospitals are caused by Klebsiella pneumoniae. However, over the past decade, extended-spectrum beta-lactamase-producing E. coli has emerged as an important cause of both hospital-onset and, in particular, community-onset bacteremia. Our patient was on immunosuppressive medications (mycophenolate) and high-dose glucocorticoids at the time of his initial presentation and calcineurin inhibitors thereafter. Therefore, he was vulnerable to develop Gram-negative bacteremia. However, an infection with Citrobacter was very unusual. Citrobacter is a Gram-negative bacillus belonging to the genus Enterobacteriaceae found mainly in the human intestine. A study on the evaluation of gut microbiota in patients with membranous nephropathy showed a significant increase in Enterobacteriaceae along with Escherichia-Shigella, Streptococcus, Peptostreptococcaceae, and Enterococcus [5]. Another study comparing the gut microbiota in normal healthy controls and patients with alcohol-induced femoral head osteonecrosis showed an increase in Klebsiella, Holdemanella, Citrobacter, and Lentilactobacillus [6]. Glucocorticoids can also influence the gut microbiota both therapeutically, as in inflammatory bowel disease-associated arthritis, or pathologically, as in osteoporosis and femoral head osteonecrosis [7]. Glucocorticoids also affect the immune system, making patients more prone to infections. Therefore, even in the absence of a specific focus of infection in the body producing bacteremia and subsequent septic arthritis, the change and increase in the spectrum of microbes in the gut can itself act as a potential source of infection in an immunocompromised state. This patient was on a heavy dose of glucocorticoids as well as mycophenolate (usually either one will be given for immune-mediated nephropathy) for more than a year, which is an unusually long duration for treatment of glomerulonephritis, making them susceptible to both osteonecrosis and Gram-negative bacteremia. The change in the gut microbiota seen in membranous nephropathy, Glucocorticoids therapy, immunosupression with mycophenolate, and femoral head osteonecrosis has created a perfect bed for our patient to develop an opportunistic infection with one of the gut microbiota (citrobacter) in the hip joint. Femoral head osteonecrosis and septic arthritis of the hip can coexist in immunocompromised patients and in patients on glucocorticoids [8]. Recent literature suggests that even immunocompetent patients with elevated ESR and WBC counts should also be evaluated for concomitant septic arthritis and osteonecrosis [9]. Salmonella, Serratia, Nocardia, and coagulase-negative Staphylococcus are the common organisms reported among those with comorbid conditions and immunocompromised status [10]. Our patient, in his initial presentation, had an elevated ESR and CRP. However, more significance was given to steroid-induced osteonecrosis, and elevated biochemical markers were attributed to his autoimmune status. Therefore, he underwent core decompression, which ended with septic arthritis sequelae. Concomitant femoral head osteonecrosis and protrusio acetabuli are also rare. This combination is mostly reported with sickle cell disease, irradiation, and rheumatoid arthritis, where the bone is inherently weak due to the underlying disease or by the treatment [11,12]. Advanced tuberculosis of the hip can also have a similar presentation [13]. Histopathological examination of the specimen is therefore very important while doing a total hip replacement. Acetabular bone deficiencies subsequent to infections and other pathologies can be challenging while performing hip replacements. Additive manufacturing technologies now aid in the planning and execution of such complex surgeries [14]. This patient had only a Grade 2 protrusio enabling us to perform surgery without any augmentation.
Concomitant septic arthritis with femoral head osteonecrosis should be considered while treating patients with femoral head osteonecrosis if they are on steroids or immunosuppressants. An elevated ESR and CRP in a patient with osteonecrosis warrants additional investigations, including ultrasound-guided aspiration – culture and blood culture before core decompression or any surgical intervention even in immunocompetent patients. Gram-negative antibiotic prophylaxis while treating patients on steroids, in an immunocompromised state, and with nephrotic syndrome can be an area of future research considering the recent advances related to gut microbiota and the immune system. Probiotic supplements in the diet of these patients, attempting to normalize the gut flora, are also an area of potential research. There are limitations in giving conclusions based on case reports, but further studies based on this can bring out more concrete evidence.
Early detection and management of concomitant septic arthritis in patients with femoral head osteonecrosis can reduce the progression to osteoarthritis as well as reduce the bone loss associated with infection while reconstructing these hips during arthroplasty.
References
- 1. Suárez CJ, Lolans K, Villegas MV, Quinn JP. Mechanisms of resistance to beta-lactams in some common gram-negative bacteria causing nosocomial infections. Expert Rev Anti Infect Ther 2005;3:915. [Google Scholar] [PubMed]
- 2. Kaufman AM, Watters TS, Henderson RA, Wellman SS, Bolognesi MP. Citrobacter koseri as a cause of early periprosthetic infection after primary total hip arthroplasty. J Arthroplasty 2011;26:978.e13-6. [Google Scholar] [PubMed]
- 3. Graff LR, Franklin KK, Witt L, Cohen N, Jacobs RA, Tompkins L, et al. Antimicrobial therapy of gram-negative bacteremia at two university-affiliated medical centers. Am J Med 2002;112:204-11. [Google Scholar] [PubMed]
- 4. Vidal F, Mensa J, Almela M, Olona M, Martínez JA, Marco F, et al. Bacteraemia in adults due to glucose non-fermentative gram-negative bacilli other than P. Aeruginosa. QJM 2003;96:227-34. [Google Scholar] [PubMed]
- 5. Dong R, Bai M, Zhao J, Wang D, Ning X, Sun S. A comparative study of the gut microbiota associated with immunoglobulin a nephropathy and membranous nephropathy. Front Cell Infect Microbiol 2020;10:557368. [Google Scholar] [PubMed]
- 6. Yue C, Ma M, Guo J, Li H, Yang Y, Liu Y, et al. Altered gut microbe metabolites in patients with alcohol -induced osteonecrosis of the femoral head: An integrated omics analysis. Exp Ther Med 2024;28:311. [Google Scholar] [PubMed]
- 7. Schepper JD, Collins F, Rios-Arce ND, Kang HJ, Schaefer L, Gardinier JD, et al. Involvement of the gut microbiota and barrier function in glucocorticoid-induced osteoporosis. J Bone Miner Res 2020;35:801-20. [Google Scholar] [PubMed]
- 8. Ardakani MV, Parviz S, Ghadimi E, Zamani Z, Salehi M, Firoozabadi MA, et al. Concomitant septic arthritis of the hip joint and femoral head avascular necrosis in patients with recent COVID-19 infection: A cautionary report. J Orthop Surg Res 2022;17:302. [Google Scholar] [PubMed]
- 9. Lee YK, Lee YJ, Ha YC, Kim KC, Koo KH. Septic arthritis of the hip in patients with femoral head osteonecrosis. Arch Orthop Trauma Surg 2011;131:1585-90. [Google Scholar] [PubMed]
- 10. Li M, Shao Z, Zhu H, Zhang Y. The diagnosis and treatment of septic hip with osteonecrosis of the femoral head. J Orthop Surg Res 2024;19:46. [Google Scholar] [PubMed]
- 11. Martinez S, Apple JS, Baber C, Putman CE, Rosse WF. Protrusio acetabuli in sickle-cell anemia. Radiology 1984;151:43-4. [Google Scholar] [PubMed]
- 12. Hall FM, Mauch PM, Levene MB, Goldstein MA. Protrusio acetabuli following pelvic irradiation. AJR Am J Roentgenol 1979;132:291-3. [Google Scholar] [PubMed]
- 13. Shanmugasundaram TK. A clinicoradiological classification of tuberculosis of the hip. In: Shanmugasundaram TK, editor. Current Concepts in Bone and Joint Tuberculosis. Madras, India: Proceedings of Combined Congress of International Bone and Joint Tuberculosis Club and the Indian Orthop Association; 1983. p. 60. [Google Scholar] [PubMed]
- 14. Agarval R, Gupta V, Singh J. Additive manufacturing based design approaches and challenges for orthopaedic bone screws: A state of the art review. J Brazil Soc Mech Sci Eng 2022;44:37. [Google Scholar] [PubMed]









