Combination of lateralized reverse total shoulder arthroplasty and pectoralis major transfer may enhance pain relief, function, and strength in patients with cuff tear arthropathy and irreparable subscapularis tears.
Chang Hee Baek, Department of Orthopaedic Surgery, Yeosu Baek Hospital, Jeollanam-do, Republic of Korea. E-mail: yeosubaek@gmail.com
Introduction: Reverse total shoulder arthroplasty (RTSA) has shown promise as a solution for individuals with rotator cuff tear arthropathy (CTA). However, RTSA has demonstrated limited improvement in internal rotation (IR) range of motion (ROM) and strength, potentially affecting patients’ ability to perform essential daily tasks such as toileting, a crucial factor that significantly influences overall patient satisfaction
Case Report: A 69-year-old female patient presented with a complaint of chronic pain and weakness in her right shoulder. The patient exhibited rotator CTA with irreparable subscapularis. As the owner of a fish restaurant, the patient underwent lateralized RTSA combined with pectoralis tendon transfer. By the post-operative 1 year 6 months, the patient’s strengths of forward elevation (FE) and IR had improved from 14.2N to 20.2N and from 15.4 to 26.2N, respectively. The ROM increased from 80° to 150° for FE, from 70° to 150° for abduction, from 25° to 35° for external rotation, and from L5 to L1 for IR at the back. With no significant complications, the patient was able to return to her workplace.
Conclusion: Primary RTSA combined with pectoralis major tendon transfer could be a viable option for restoring both ROM and strength in FE and IR, particularly in cases of rotator CTA with irreparable subscapularis tears.
Keywords: Pectoralis Major transfer, reverse total shoulder arthroplasty, irreparable subscapularis tear, rotator cuff arthropathy.
Reverse total shoulder arthroplasty (RTSA) has shown promise as a solution for individuals with rotator cuff tear arthropathy (CTA) [1]. RTSA has demonstrated satisfactory clinical results in terms of alleviating pain and improving shoulder’s range of motion (ROM) [2,3]. However, the extent to which it effectively addresses issues related to internal rotation (IR) and external rotation (ER) remains a subject of ongoing discussion [1,4,5]. Gerber et al. [4] and Boileau et al. [6] introduced the concept of combining RSA with the modified L’Episcopo procedure to address the often observed ER deficit in patients who have undergone RTSA, particularly in those with massive posterior superior rotator cuff tears. This surgical technique yielded significant improvements in pain, ROM, and functional scores [7]. Similarly, Baek et al. [8] demonstrated the effectiveness of RTSA combined with anterior latissimus dorsi and teres major (LDTM) transfer in patients afflicted with CTA and irreparable subscapularis tears. The findings presented promising short-term outcomes, leading to an improvement in both forward elevation (FE) and IR. Considering the critical role of IR in post-operative satisfaction and overall clinical prognosis, the restoring IR becomes especially pertinent in cases involving CTA with irreparable subscapularis tears [9,10]. Historically, the transfer of the pectoralis major (PM) tendon has been the preferred approach for addressing irreparable subscapularis tears [11]. Recent biomechanical studies [12,13] have shown that the PM tendon transfer combined with RTSA carries strong IR moment arm. Hence, the combination of RTSA with PM tendon transfer holds the potential to enhance shoulder function and strength in patients with CTA and IR deficit. This report’s primary aim is to provide the technique and outcomes of a single patient who underwent RTSA combined with PM tendon transfer.
Case description
A 69-year-old right hand dominant female patient presented to our clinic for the right shoulder pain and weakness in her right shoulder for the past 3 years, without any trauma history (Fig. 1).
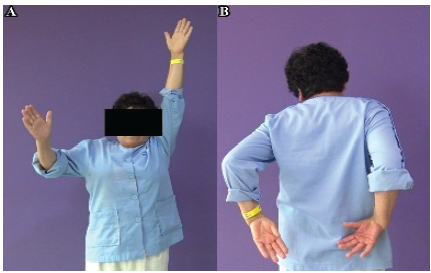
Figure 1: Pre-operative clinical photographs. (a) The pre-operative clinical photos of the patient showing limited active forward elevation and (b) internal rotation at side of the right shoulder.
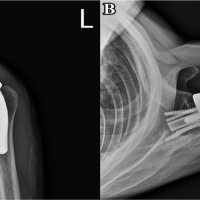
Patient did not have any history of shoulder surgery. FE was measured at 80°, abduction (ABD) at 70°, ER at 25°, and IR reached at L5 level. Functional assessment scores were unsatisfactory: Pain visual analog scale (VAS) of 4, Constant score of 51/100, and American Shoulder and Elbow Surgeons (ASES) score of 51/100. Strengths of FF, ABD, ER, and IR were 14.2N, 15.1N, 18.2N, and 15.4N, respectively. Radiographic evaluation revealed glenohumeral arthritis and superior translation of the humeral head (Hamada [14] grade 3) (Fig. 2a and b). Magnetic resonance imaging scan showed irreparable tears of the subscapularis, supraspinatus, and infraspinatus tendon, exhibiting retraction toward the glenoid surface and poor muscle quality (Goutallier [15] grade III fatty infiltration and atrophy) (Fig. 2c and d). The patient was the owner of a sushi restaurant for a living. She complained that she could not fillet fish at the restaurant and wash dishes due to weakness in her shoulder. The patient underwent RTSA combined with PM tendon transfer.
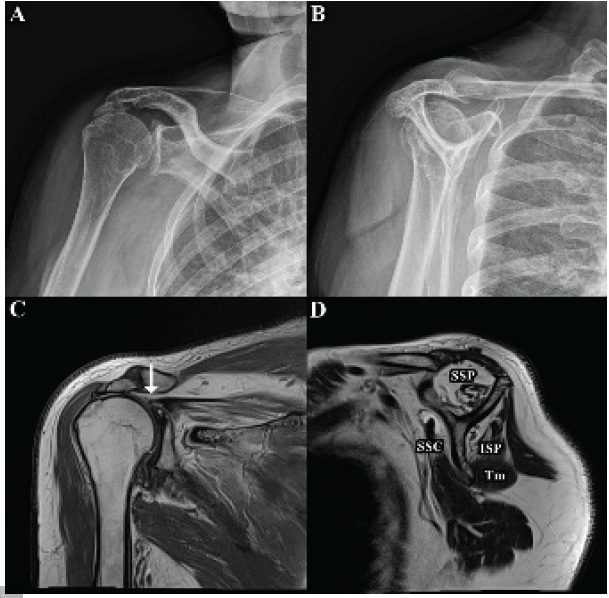
Figure 2: Pre-operative radiograph and magnetic resonance imaging (MRIs) of right shoulder. (a) Pre-operative radiograph of the right shoulder demonstrates rotator cuff arthropathy in the True AP view, and (b) in the supraspinatus outlet view. (c) Pre-operative MRI of the right shoulder shows the supraspinatus tendon (white arrow) retracted to the level of the glenoid in a T2-weighted coronal-view MRI, and (d) shows severe fatty infiltration and atrophy of the SSC, SSP, and ISP in a T2-weighted oblique sagittal-view MRI. AP: Anterior-posterior, SSC: Subscapularis, SSP: Supraspinatus, ISP: Infraspinatus, TM: Teres minor.
Surgical procedure
Patient was placed in the beach-chair position under general anesthesia with an interscalene block. A standard deltopectoral approach was performed with the incision extended to the inferior border of the PM tendon. Tenotomy of the long head of the biceps was performed. Both upper and lower border of PM muscle was meticulously released from surround soft tissue. PM tendon was detached from the humerus, and two long forceps were used to hold both edges of the detached PM tendon, followed by placement of non-absorbable sutures in Krackow fashion (Fig. 3). While applying traction to sutures, PM muscle was bluntly released from surrounding adhesions to acquire further excursion.
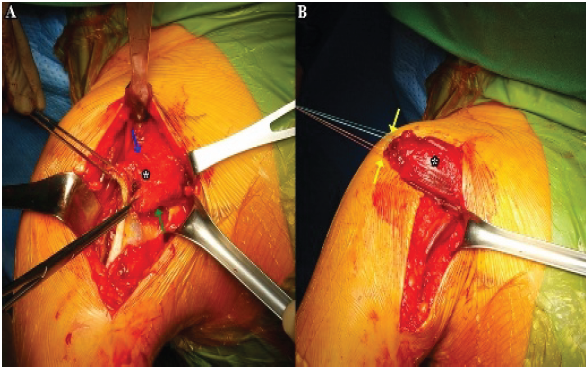
Figure 3: Pectoralis major (PM) tendon preparation. (a) Intraoperative image of the right shoulder shows that both the upper (blue arrow) and lower borders (green arrow) of the PM muscle (white asterisk) are meticulously released from surrounding soft tissue, and the PM tendon is detached from the insertion site on the humerus. (b) Non-absorbable suture (yellow arrow) is placed on both edges of the PM tendon in a Krackow fashion.
After preparation of the PM tendon, the RTSA procedure proceeded using Equinoxe reverse total shoulder system (Exactech Inc, Gainesville, FL, USA). Humeral head bone cutting was started 5 mm above the junction of the cephalic cartilage and the greater tuberosity with an inclination of 132.5° and retroversion of 20° (Fig. 4a and b). The metaphysis and epiphysis were prepared with increasingly larger reamers to conserve as much cancellous bone as possible to allow press-fit fixation of the humeral stem. The glenoid was prepared after circumferential capsulectomy (Fig. 4c). The baseplate was located at the inferior glenoid, with an inferior tilt to avoid scapular notching (Fig. 4d).
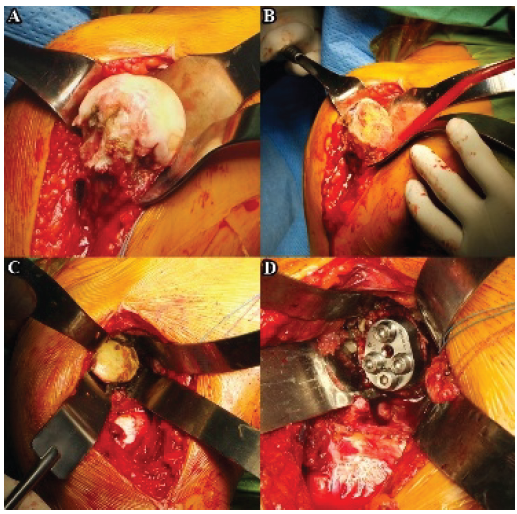
Figure 4: Reverse total shoulder arthroplasty procedure. (a) Intraoperative image of right shoulder showing advanced arthritis in humeral head, (b) humeral head bone cutting, (c) glenoid after circumferential capsulectomy, and (d) placement of glenoid component.
Following the glenoid procedure, six drill holes were made distally to the lateral edge of the greater tuberosity and laterally to the biceps groove (Fig. 5a). Sutures of harvested PM tendon were passed through these holes (Fig. 5b). Furthermore, additional three sutures were passed through these holes, forming respective loops; then, the humeral stem was passed down through the preplaced loop sutures (Fig. 5c).
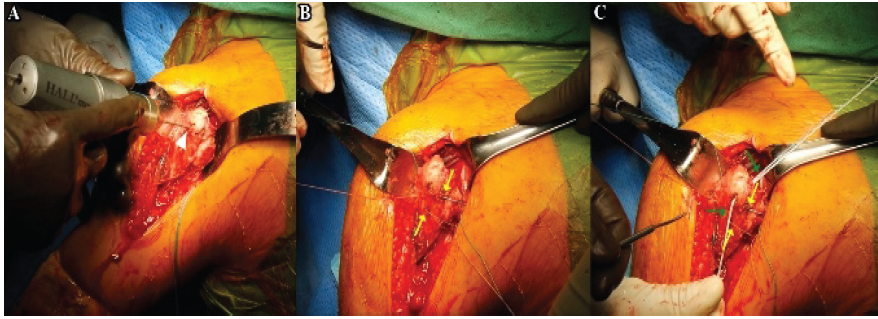
Figure 5: Drill holes before pectoralis major (PM) transfer. (a) Intraoperative image of the right shoulder shows the creating six drill holes (white arrow head) distal to the lateral edge of the greater tuberosity and lateral to the biceps groove. (b) Krackow sutures (yellow arrow) of the PM tendon are passed through the drill holes. (c) Three additional sutures (green arrow) are passed through the same drill holes, forming a loop.
Finally, the looped sutures were pulled taut around the humeral stem before final impaction (Fig. 6a and b). Following humeral stem placement, the humerus was reduced on the glenosphere. With the patient’s arm positioned in full IR and approximately 45° ABD, the sutures were threaded through the harvested PM tendon and tied together to attach PM to greater tuberosity (Fig. 6C). Finally, a firm attachment of the PM tendon to the humerus was ensured (Fig. 6D), and impingement was verified by internally and externally rotating the arm (Fig. 7). Wound was closed layer by layer.
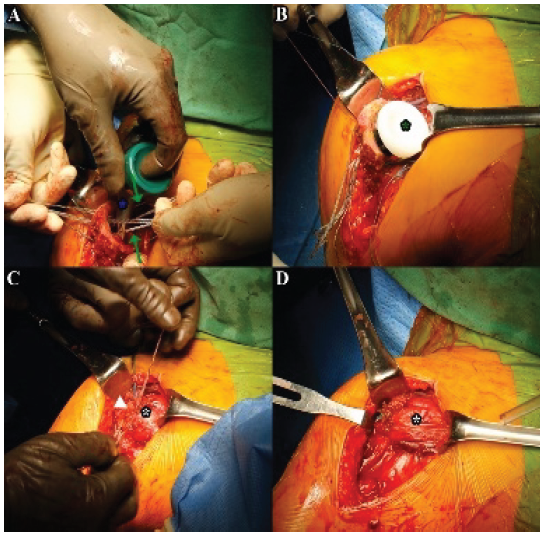
Figure 6: Insertion of humeral stem and securing pectoralis major (PM) tendon to humerus. (a) Intraoperative image of the right shoulder shows the humeral stem (blue asterisk) being passed down through the preplaced loop sutures (green arrow). (b) The humeral insert is placed (green asterisk). (c) With the patient’s arm positioned in full internal rotation and approximately 45° of abduction, the PM tendons (white asterisk) were tied (white arrow head). (d) The final appearance of the pectoralis major tendon (white asterisk) transfer.
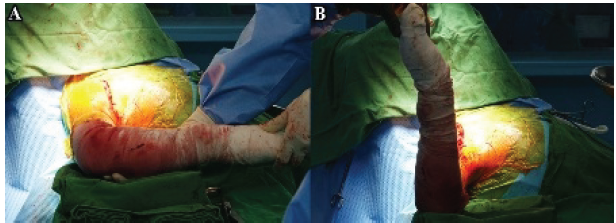
Figure 7: Intraoperative range of motion after the reverse total shoulder arthroplasty combined with pectoralis major tendon transfer. (a) Intraoperative image of right shoulder in full internal rotation and (b) external rotation at 90° abduction.
Post-operative rehabilitation
The standard tendon transfer rehabilitation protocol was performed as previously described in the literature [8,16]. During the initial 4 weeks, patients wore ABD brace and immobilized. Yet, intermittent movement of elbow, wrist, and fingers was allowed. While wearing the brace, the patient was able to engage in routine tasks such as eating and writing. After post-operative 4 weeks, brace was discontinued, and patients started active-assisted ROM exercises, allowing patients to actively participate in regaining ROM. After post-operative 3 months, patients were permitted to strengthening exercises in all directions. However, heavy labor work and sports were strictly prohibited until the post-operative 6 months.
Post-operative outcome
By post-operative 1-year and 6-month, the patient reported satisfaction with the procedure’s outcomes, achieving pain VAS of 1, Constant score of 76/100, and ASES score of 79/100. ROM increased to 150° for FE, 150° for ABD, and 35° for ER and IR to level of L1 (Fig. 8).
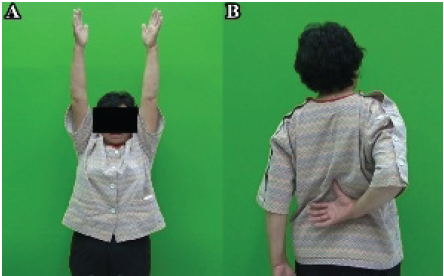
Figure 8: Post-operative clinical photographs. (a) Clinical photos of the patient at post-operative 1 year and 6 months show improved active forward elevation, and (b) internal rotation at the side of the right shoulder.
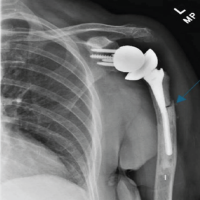
Shoulder strength was evaluated with a handheld dynamometer Hoggan Health Industries, UT, USA. Strengths of FF and IR had improved to 20.2N and 26.2N, respectively. However, ABD and ER did not improve as much with values of 15.4N and 19.1N, respectively. Radiographic image showed securely fixed implant without any signs of loosening (Fig. 9a), and sonographic panoramic scan image demonstrated the intact transferred PM tendon at the bone-to-tendon site (Fig. 9b). With no significant complications, the patient successfully returned to work at the post-operative 6 months and has continued to work thereafter without any significant complications.
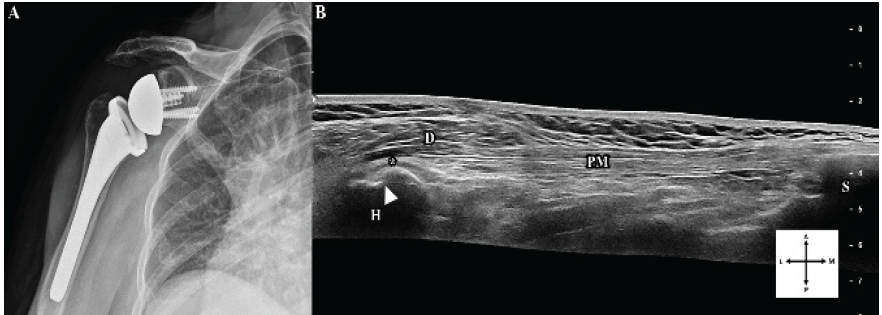
Figure 9: Post-operative radiograph and sonography of transferred PM tendon. (a) Post-operative radiograph of the right shoulder at post-operative 1 year and 6 months shows reverse total shoulder arthroplasty in the true AP view. (b) Sonographic panoramic scan image displays the intact transferred PM tendon at the bone-to-tendon site in the long-axis of the PM muscle. PM: Pectoralis major, H: Humerus, D: Deltoid, S: Sternum, white asterisk, bone-to-tendon site of transferred PM, white arrow head, bicipital groove of humerus, A: Anterior, P: Posterior, L: Lateral, M: Medial.
The current case report illustrates a clinical outcome of a single patient who underwent RTSA combined with PM transfer for CTA and irreparable subscapularis tear. By post-operative 1 year and 6 months, the patient reported pain relief and improved function. In addition, the patient demonstrated increased strength in FE and IR, along with an increase in ROM. The patient did not experience any significant complications from the application of PM transfer and has successfully returned to work. The necessity of repairing the subscapularis in setting of RTSA remains a subject of ongoing debate. Collin et al. [17] advocated for the repair of reparable subscapularis tendons during RTSA whenever feasible. However, in cases where the subscapularis is irreparable, alternative treatment options may be necessary to restore IR. Kany [18] has suggested the utilization of RTSA with anterior latissimus dorsi (LD) transfer for patients with combined loss of elevation and IR, and Baek et al. [8] proposed the use of RTSA with anterior LDTM transfer. Werthel et al. [13] conducted a biomechanical study comparing IR moment arm for various types of tendon transfers, including LD, teres minor, and PM transfers, with and without RTSA to restore IR. The study demonstrated that IR moment arm was greatest in PM tendon transfer. Furthermore, Chan et al. [12] reported on the biomechanical efficacy of PM tendon transfer in restoring IR in lateralized RTSA. Nonetheless, as there is a lack of clinical studies on RTSA combined with PM transfer, further clinical studies are still warranted. Despite the development of lateralized RTSA to address horizontal rotational insufficiency [8,16], RTSA has demonstrated limited improvement in IR, potentially affecting patients’ ability to perform essential daily tasks such as toileting, a crucial factor that significantly influences overall patient satisfaction [9,19]. Although there are several studies about increased IR with lateralized RTSA [20,21], clinical outcome often vary and can be unpredictable [22,23]. Kim et al. [24] reported that implant type and implant lateralization were not independent factors influencing post-operative IR. Gibian et al. [22] reported that higher pre-operative IR and 1-year post-operative FE were independent predictors of sufficient post-operative IR after RTSA. In the current case report, we used lateralized RTSA as our choice of implant. The observed increase in post-operative IR may or may not be attributed to the utilization of a lateralized-type prosthesis. Nevertheless, we noted an increase in strength and observed no decrease in horizontal ROM following the application of the PM transfer. To minimize intraoperative complications and improve the reproducibility of this technique, several technical considerations should be emphasized. Adequate exposure through an extended deltopectoral approach allows safe identification and complete release of the PM tendon while avoiding excessive traction or unintended soft-tissue injury. Conservative humeral bone preparation and inferior positioning of the glenoid baseplate with slight inferior tilt may reduce the risk of intraoperative fracture and post-operative impingement. In addition, precise placement of drill holes and secure, balanced suture fixation of the transferred tendon help prevent tendon tearing, mal-tensioning, or fixation failure. Finally, intraoperative dynamic assessment through a full ROM is recommended to confirm stable fixation and absence of impingement before wound closure. This case report has several strengths. First, it provides a detailed clinical and technical description of combining lateralized RTSA with PM tendon transfer in a patient with CTA and irreparable subscapularis deficiency, a clinical scenario for which limited evidence currently exists. Furthermore, the patient’s successful return to physically demanding occupational activities underscores the potential functional relevance of restoring IR strength in daily life. However, several limitations should be acknowledged. As a single case report, the findings are inherently limited in generalizability and do not allow comparison with alternative tendon transfer options or RTSA alone. In addition, the relatively short follow-up duration restricts conclusions regarding long-term durability of strength recovery, tendon integrity, and implant-related outcomes. Larger clinical studies with longer follow-up are necessary to validate the effectiveness and durability of this combined surgical approach.
In this case report, we showed that lateralized RTSA combined with PM transfer has improved pain and function, as well as increased ROM and strength in FE and IR. As a case report, it is important to acknowledge certain limitations. Further clinical studies are warranted, as the results are based on observations from a single patient. Nevertheless, this case report holds value in suggesting that the combination of PM transfer and lateralized RTSA may potentially enhance strength and ROM of FE and IR in patients with CTA and irreparable subscapularis tear.
The combination of lateralized RTSA and PM transfer could be a viable treatment option for patients with CTA and irreparable subscapularis tears.
References
- 1. Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: Design, rationale, and biomechanics. J Shoulder Elbow Surg 2005;14:147-61. [Google Scholar] [PubMed]
- 2. Burden EG, Batten TJ, Smith CD, Evans JP. Reverse total shoulder arthroplasty. Bone Joint J 2021;103-B:813-21. [Google Scholar] [PubMed]
- 3. Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer award 2005: The grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006;15:527-40. [Google Scholar] [PubMed]
- 4. Gerber C, Pennington SD, Lingenfelter EJ, Sukthankar A. Reverse delta-III total shoulder replacement combined with latissimus dorsi transfer. A preliminary report. J Bone Joint Surg Am 2007;89:940-7. [Google Scholar] [PubMed]
- 5. Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: A review of results according to etiology. J Bone Joint Surg Am 2007;89:1476-85. [Google Scholar] [PubMed]
- 6. Boileau P, Chuinard C, Roussanne Y, Neyton L, Trojani C. Modified latissimus dorsi and teres major transfer through a single delto-pectoral approach for external rotation deficit of the shoulder: As an isolated procedure or with a reverse arthroplasty. J Shoulder Elbow Surg 2007;16:671-82. [Google Scholar] [PubMed]
- 7. Hones KM, Rakauskas TR, Wright JO, King JJ, Wright TW, Werthel JD, et al. Outcomes of reverse total shoulder arthroplasty with latissimus dorsi tendon transfer for external rotation deficit: A systematic review and meta-analysis. JBJS Rev 2023;11:e23.00048. [Google Scholar] [PubMed]
- 8. Baek CH, Kim JG, Baek GR. Restoration of active internal rotation following reverse shoulder arthroplasty: Anterior latissimus dorsi and teres major combined transfer. J Shoulder Elbow Surg 2022;31:1154-65. [Google Scholar] [PubMed]
- 9. Kim MS, Jeong HY, Kim JD, Ro KH, Rhee SM, Rhee YG. Difficulty in performing activities of daily living associated with internal rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2020;29:86-94. [Google Scholar] [PubMed]
- 10. Murray IA, Johnson GR. A study of the external forces and moments at the shoulder and elbow while performing every day tasks. Clin Biomech (Bristol) 2004;19:586-94. [Google Scholar] [PubMed]
- 11. Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am 1996;78:1015-23. [Google Scholar] [PubMed]
- 12. Chan K, Langohr GD, Athwal GS, Johnson JA. The biomechanical effectiveness of tendon transfers to restore rotation after reverse shoulder arthroplasty: Latissimus versus lower trapezius. Shoulder Elbow 2022;14:48-54. [Google Scholar] [PubMed]
- 13. Werthel JD, Schoch BS, Hooke A, Sperling JW, An KN, Valenti P, et al. Biomechanical effectiveness of tendon transfers to restore active internal rotation in shoulder with deficient subscapularis with and without reverse shoulder arthroplasty. J Shoulder Elbow Surg 2021;30:1196-206. [Google Scholar] [PubMed]
- 14. Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res 1990;254:92-6. [Google Scholar] [PubMed]
- 15. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and post-operative evaluation by CT scan. Clin Orthop Relat Res 1994;304:78-83. [Google Scholar] [PubMed]
- 16. Baek GR, Kim JG, Baek CH, Baek G, Chung MS, Kao O, et al. Latissimus Dorsi and teres major tendon transfer increases internal rotation torque following lateralized reverse shoulder arthroplasty with subscapularis insufficiency. Arch Orthop Trauma Surg 2023;143:5759-66. [Google Scholar] [PubMed]
- 17. Collin P, Rol M, Muniandy M, Gain S, Lädermann A, Ode G. Relationship between postoperative integrity of subscapularis tendon and functional outcome in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2022;31:63-71. [Google Scholar] [PubMed]
- 18. Kany J. Tendon transfers in rotator-cuff surgery. Orthop Traumatol Surg Res 2020;106:S43-51. [Google Scholar] [PubMed]
- 19. Rojas J, Joseph J, Liu B, Srikumaran U, McFarland EG. Can patients manage toileting after reverse total shoulder arthroplasty? A systematic review. Int Orthop 2018;42:2423-8. [Google Scholar] [PubMed]
- 20. Collin P, Liu X, Denard PJ, Gain S, Nowak A, Lädermann A. Standard versus bony increased-offset reverse shoulder arthroplasty: A retrospective comparative cohort study. J Shoulder Elbow Surg 2018;27:59-64. [Google Scholar] [PubMed]
- 21. Mollon B, Mahure SA, Roche CP, Zuckerman JD. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: An analysis of 476 shoulders. J Shoulder Elbow Surg 2017;26:1253-61. [Google Scholar] [PubMed]
- 22. Gibian JT, Sokrab R, Hill JR, Keener JD, Zmistowski BM. Predictors of internal rotation after reverse shoulder arthroplasty. Arch Bone Jt Surg 2023;11:696-703. [Google Scholar] [PubMed]
- 23. Youn SM, Lee HS, Rhee SM, Rhee YG. Medialized vs. Lateralized humeral implant in reverse total shoulder arthroplasty: The comparison of outcomes in pseudoparalysis with massive rotator cuff tear. J Shoulder Elbow Surg 2022;31:736-46. [Google Scholar] [PubMed]
- 24. Kim SC, Lee JE, Lee SM, Yoo JC. Factors affecting internal rotation after reverse shoulder arthroplasty. J Orthop Sci 2022;27:131-8. [Google Scholar] [PubMed]