Timely closed reduction of multiple metatarsophalangeal joint dislocations, even when associated with an intra-articular fracture, can yield excellent outcomes with conservative treatment.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Introduction: Metatarsophalangeal (MTP) joint dislocations are uncommon due to the joint’s inherent stability. Simultaneous dislocations of multiple lesser MTP joints with an associated fracture are extremely rare and typically result from high-energy trauma.
Case Report: A 36-year-old female sustained dorsolateral dislocation of the 2nd, 3rd, and 4th MTP joints and an intra-articular fracture of the 5th metatarsal base following a tractor run-over injury. Closed reduction under regional anesthesia was successfully performed. The joints were found to be stable post-reduction and immobilized with a below-knee slab. The patient opted against surgical intervention for the 5th metatarsal fracture. At the 3-month follow-up, she showed complete recovery with excellent functional scores.
Conclusion: Multiple MTP dislocations can be successfully managed with closed reduction and conservative treatment when joint stability is achieved. Patient compliance and close follow-up are critical.
Keywords: Metatarsophalangeal joint, dislocation, metatarsal fracture, below-knee slab.
The metatarsophalangeal (MTP) joints are synovial condyloid joints that play a critical role in forefoot biomechanics, particularly during the toe-off phase of gait. During this phase, the MTP joints dorsiflex significantly, contributing to forward propulsion. Their stability and motion are governed by an intricate network of supporting structures, including the joint capsule, plantar plate, collateral ligaments, and extensor tendons [1]. Due to these stabilizing elements, dislocations of the MTP joints are relatively uncommon, especially in the lesser toes. When such injuries occur, they most frequently involve the first MTP joint because of its weight-bearing and propulsive function [2]. Traumatic dislocations of the lesser MTP joints (2nd–5th) are far less common and are typically associated with high-energy mechanisms such as motor vehicle accidents, crush injuries, or falls from height [3]. Simultaneous dislocation of multiple lesser MTP joints in a closed manner is exceptionally rare. In these cases, closed reduction can be challenging or impossible due to anatomical obstacles such as the interposed plantar plate or buttonholing of the joint capsule [4]. As a result, open reduction may be required, especially in irreducible cases. Moreover, concomitant metatarsal fractures – such as intra-articular injuries – add to the complexity of treatment planning and often influence whether surgical fixation is indicated [5]. We report a unique case of closed dorsolateral dislocation of the 2nd–4th MTP joints along with an intra-articular fracture of the 5th metatarsal base, successfully managed by closed reduction and conservative care, highlighting the importance of early recognition and individualized treatment planning.
A 36-year-old female presented to the emergency department after a tractor ran over her right foot. She was unable to stand without support due to pain and deformity. Clinical examination revealed swelling, deformity, and tenderness over the dorsum of the right foot (Fig. 1). Active toe movements were present but painful. There were no open wounds, and distal neurovascular examination was normal.
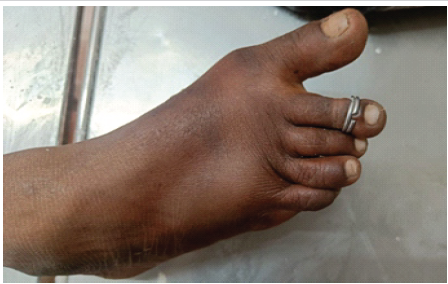
Figure 1: Clinical image of right foot at presentation showing swelling and deformity at 2nd, 3rd, and 4th metatarsophalangeal joints.
Plain radiographs of the right foot showed dorsolateral dislocation of the 2nd, 3rd, and 4th MTP joints and an oblique intra-articular fracture of the 5th metatarsal base (Fig. 2).

Figure 2: X-ray of right foot showing dorsolateral dislocation of 2nd, 3rd, and 4th metatarsophalangeal joints.
Under regional anesthesia using an ankle block, closed reduction of the dislocated MTP joints was performed. Reduction was confirmed both clinically by the restoration of normal foot contour (Fig. 3) and radiologically on post-reduction X-rays (Fig. 4). The joints were found to be stable post-reduction (Fig. 5).

Figure 3: Clinical image of the right foot showing normal alignment of all the metatarsophalangeal joints.

Figure 4: X-ray of right foot showing stable metatarsophalangeal joints post-closed reduction.

Figure 5: X-ray of right foot showing stable metatarsophalangeal joints with complete union of the base of the 5th metatarsal fracture.
Immobilization was achieved using a below-knee posterior slab with dorsal reinforcement and toe support, keeping the MTP joints in a neutral position. The patient declined surgical fixation of the 5th metatarsal base fracture, and conservative treatment was continued. At 6 weeks of follow-up, the slab was removed, and physiotherapy for mobilization was started. At 3 months follow-up, the patient reported no pain, had a normal gait, and showed no recurrence of deformity. Functional assessment using the American Orthopaedic Foot and Ankle Society (AOFAS) mid-foot scoring system revealed the following results, as mentioned in Table 1.
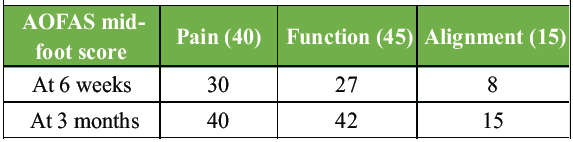
Table 1: Functional assessment using the American Orthopaedic Foot and Ankle Society (AOFAS) mid-foot scoring system
MTP joint dislocations, especially of the lesser toes, are infrequent due to the robust ligamentous and capsular structures that provide significant joint stability [6]. These joints are designed to withstand substantial mechanical load, particularly during the terminal stance and pre-swing phases of the gait cycle [7]. The anatomical features that confer this stability – namely the plantar plate, collateral ligaments, joint capsule, and deep transverse metatarsal ligament – also contribute to the complexity of managing dislocations when they occur [8]. Traumatic MTP dislocations most commonly affect the first MTP joint due to its exposure and greater load-bearing function. Lesser MTP joint dislocations (2nd–5th) are uncommon and usually result from high-energy trauma such as vehicular accidents, crush injuries, or sporting incidents. When multiple MTP joints are involved, it is often indicative of a severe mechanism of injury. The rarity of such injuries is highlighted in the literature, with only a handful of cases describing simultaneous dislocation of more than two lesser MTP joints [9,10,11]. The direction of dislocation is typically dorsal due to the biomechanics of forced hyperextension. This results in the metatarsal heads migrating plantarly while the proximal phalanges are displaced dorsally. In some cases, soft tissue structures – particularly the plantar plate and capsule – may become interposed between articulating surfaces, rendering closed reduction difficult or impossible [9,11]. Hey et al. emphasized that failed closed reductions are frequently attributed to such soft-tissue entrapment and may require open reduction for anatomical realignment [12]. Several surgical approaches for open reduction have been described. The dorsal approach is commonly preferred as it avoids injury to plantar neurovascular structures, although it limits access to the plantar plate for repair. In contrast, the plantar approach allows for direct visualization and repairs of the plantar plate and transverse metatarsal ligament but carries greater risks of scar sensitivity and delayed wound healing. The choice of approach is thus tailored based on surgeon preference, soft-tissue condition, and joint stability [4]. Despite these complexities, when closed reduction is achieved – as in our case – outcomes can be excellent with proper immobilization and rehabilitation. The successful reduction in our case indicates that the anatomical structures were likely stretched or displaced but not torn or interposed, allowing for effective non-operative management. The importance of prompt diagnosis cannot be overstated. Subtle clinical signs such as increased interdigital space, plantar bony prominence, or loss of toe cascade may suggest underlying MTP dislocations. Radiographic assessment with true lateral and oblique views is essential to avoid missed injuries, as delayed recognition may lead to persistent joint incongruity, stiffness, pain, or secondary deformities such as claw toe or transfer metatarsalgia [3]. Functional outcome measures such as the AOFAS mid-foot score serve as reliable tools for tracking recovery. Our patient showed progressive improvement in all domains – pain, function, and alignment – indicating the adequacy of conservative treatment despite the presence of an associated intra-articular fracture. This aligns with the findings of Arastu and Buckley, who supported conservative management in cases where the fracture is minimally displaced and the patient remains compliant [5].
Closed traumatic dislocations of multiple MTP joints are rare injuries that require a high index of suspicion and prompt management. When diagnosed early and reduced successfully, even complex injuries with associated fractures may be treated conservatively with favorable outcomes. Individualized treatment decisions, patient compliance, and close follow-up are key to achieving optimal results.
Even in rare, high-energy foot injuries involving multiple MTP dislocations and associated fractures, closed reduction and conservative treatment can be successful when performed promptly with appropriate immobilization and follow-up.
References
- 1. Hicks JH. The mechanics of the foot. II. The plantar aponeurosis and the arch. J Anat 1954;88:25-30. [Google Scholar] [PubMed]
- 2. Kinter CW, Hodgkins CW. Lesser metatarsophalangeal instability: Diagnosis and conservative management of a common cause of metatarsalgia. Sports Health 2020;12:390-4. [Google Scholar] [PubMed]
- 3. Bhide PP, Anantharaman C, Mohan G, Raju K. A case of simultaneous traumatic dorsal dislocation of all five metatarsophalangeal joints treated successfully with closed reduction. J Foot Ankle Surg 2016;55:423-6. [Google Scholar] [PubMed]
- 4. Leung WY, Wong SH, Lam JJ, Ip FK, Ko PS. Presentation of a missed injury of a metatarsophalangeal joint dislocation in the lesser toes. J Trauma 2001;50:1150-2. [Google Scholar] [PubMed]
- 5. Arastu MH, Buckley RE. Tarsometatarsal joint complex and midtarsal injuries. Acta Chir Orthop Traumatol Cech 2012;79:21-30. [Google Scholar] [PubMed]
- 6. Tablante AJ, Kurokawa H, Ueno Y, Wanezaki Y, Mei N, Li Y, et al. Second metatarsophalangeal joint dislocation in hallux valgus: A radiographic study using a two-dimensional coordinate system. BMC Musculoskelet Disord 2025;26:204. [Google Scholar] [PubMed]
- 7. Jeong B, Kim S, Son J, Kim Y. Kinetic analysis of the metatarsophalangeal joint in normal subjects and hallux valgus patients during walking using a four-segment foot model. J Foot Ankle Res 2014;7 Suppl 1:A125. [Google Scholar] [PubMed]
- 8. Wang B, Guss A, Chalayon O, Bachus KN, Barg A, Saltzman CL. Deep transverse metatarsal ligament and static stability of lesser metatarsophalangeal joints: A cadaveric study. Foot Ankle Int 2015;36:573-8. [Google Scholar] [PubMed]
- 9. Ito MM, Murase K, Tanaka S, Yamashita T. Dislocation of all metatarsophalangeal joints caused by horse injury. J Trauma 2007;63:938-9. [Google Scholar] [PubMed]
- 10. Neogi DS, Bandekar SM, Sadekar V, Patnaik S, Bhat T, D’Mello Z. Irreducible dislocation of all the lesser metatarsophalangeal joints of the foot: A case report. Foot Ankle Spec 2012;5:324-6. [Google Scholar] [PubMed]
- 11. Raj S, Subramani S, Babar SJ, Balaji MS Sr., Anand V. Rare case report of closed traumatic dislocation of second to fifth metatarsophalangeal joints. Cureus 2020;12:e11745. [Google Scholar] [PubMed]
- 12. Hey HW, Chang G, Hong CC, Kuan WS. Irreducible dislocation of the fourth metatarsophalangeal joint–a case report. Am J Emerg Med 2013;31:265.e1-3. [Google Scholar] [PubMed]