High-energy clavicular fractures with suspected posterior acromioclavicular dislocation require prompt confirmatory imaging and surgical management to stabilize both the acromioclavicular joint and the clavicle.
Dr. Braghis Vlad, Department of Orthopaedic Surgery and Traumatology, eHnv, Yverdon-les-Bains Hospital, Yverdon-les-Bains, Switzerland. E-mail: vlad.braghis@ehnv.ch
Introduction: Acromioclavicular joint (ACJ) dislocation combined with an ipsilateral medial clavicle fracture is extremely rare and results from high-energy shoulder trauma. This case report describes a medial clavicle fracture associated with ipsilateral ACJ dislocation, classified as type IV according to the Rockwood classification.
Case Report: A 23-year-old male presented for an orthopedic consultation 1 week after a skiing accident in which he sustained direct trauma to his left shoulder upon impact with the ground. Radiographs and computed tomography (CT) scans of the left shoulder revealed a medial clavicle fracture with ipsilateral ACJ dislocation, classified as type IV according to the Rockwood classification. The patient was treated with an anterior 3.5 clavicle plate combined with an ACJ cerclage wire in a figure-eight configuration and a coracoclavicular endobutton placed arthroscopically. After a 6-month follow-up, the patient demonstrated excellent results in shoulder range of motion and function. The patient’s Constant-Murley score was 92.
Conclusion: A medial clavicle fracture resulting from high-energy trauma should raise suspicion for a concomitant ACJ dislocation. To confirm this association, additional imaging studies, such as a shoulder CT scan, are essential.
Keywords: Clavicle fractures, acromioclavicular dislocation, Rockwood grade IV, trauma.
Medial third clavicle fractures are relatively rare, accounting for approximately 2–5% of all clavicle fractures [1]. Their incidence is lower than midshaft clavicle fractures, which comprise about 75-80% of cases. Acromioclavicular dislocations, on the other hand, are more common, representing up to 12% [2] of traumatic shoulder injuries, predominantly affecting young adults and athletes. However, posterior dislocations classified as Rockwood grade IV are rare [3], constituting only a small percentage of total acromioclavicular dislocations. The combination of a medial third clavicle fracture and a posterior acromioclavicular dislocation is an extremely rare event, with very few cases described in the literature. This association may result from high-energy trauma, such as motor vehicle accidents or sports injuries (e.g., skiing, cycling, or contact sports) [4].
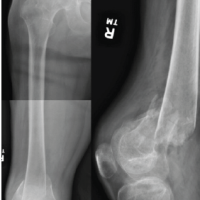
A 23-year-old right-handed male, working in automation and a non-smoker, sustained a skiing accident with direct impact on the left shoulder. Following the trauma, he experienced acute pain and functional impairment of the left upper limb. On the day of the injury, initial clinical and radiological evaluation revealed a slightly displaced closed fracture of the medial third of the left clavicle (Fig. 1).
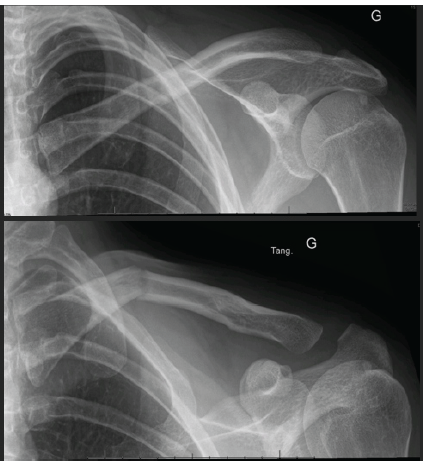
Figure 1: Radiograph taken at the first consultation, 1 week after the accident.
The patient was treated with orthopedic vest immobilization and analgesic therapy. At the 7-day follow-up, during the clinical and radiological control visit, the patient was no longer wearing the orthopedic vest due to discomfort with immobilization. His condition was as follows: pain was controlled, and physical examination showed swelling at the medial clavicle without signs of skin compromise, tenderness on palpation of the acromioclavicular joint (ACJ) and fracture site, and no signs of horizontal or vertical instability of the distal clavicle. Radiological evaluation showed a slightly displaced fracture of the medial third of the left clavicle with increased angulation compared to the initial radiograph, along with an acromioclavicular distortion and suspected posterior dislocation of the distal clavicle (Rockwood stage IV) on the tangential projection (Fig. 2).
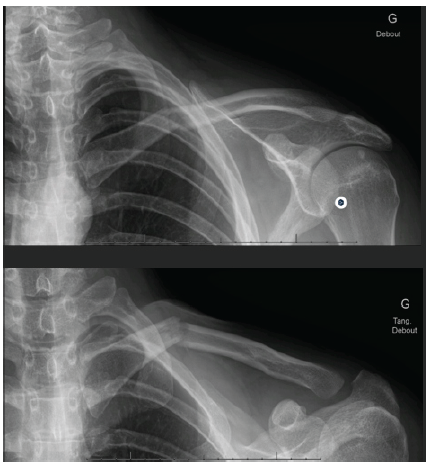
Figure 2: Radiograph taken at the second consultation showing a secondary displacement.
Given the complexity of the injury, a computed tomography (CT) scan with 3D reconstruction was indicated to precisely assess the extent of the clavicle fracture and confirm the posterior dislocation of the distal clavicle. After radiological confirmation of the posterior dislocation (Fig. 3) associated with the medial clavicle fracture, surgical treatment was chosen due to progressive clavicular shortening with altered scapulothoracic biomechanics, risk of chronic clavicular instability, and potential persistent pain caused by clavicular impingement with surrounding muscles and structures, leading to mobility difficulties, particularly in abduction and flexion.
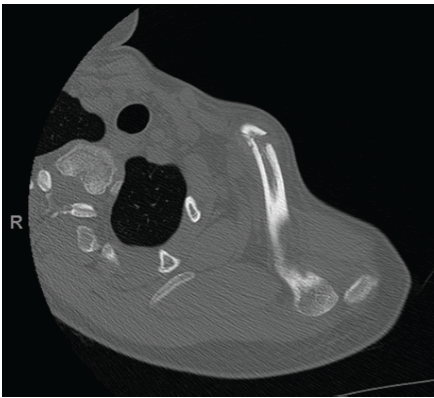
Figure 3: Computed tomography scan with 3D reconstruction, with confirmation of the posterior dislocation of the acromioclavicular joint associated with the medial clavicle fracture.
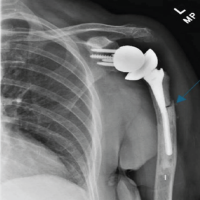
The planned surgical intervention included the reduction and fixation of the ACJ. We used a wire cerclage in a figure-eight pattern for the ACJ and performed medial clavicle fixation using a 3.5 reconstruction plate anteriorly. X-rays showed good reduction, and clinically, there was no “piano key” sign. However, we still placed an endobutton to ensure stability under arthroscopy (Fig. 4).

Figure 4: Pre-operative marking. Medial clavicle fixation using an anteriorly placed 3.5 mm reconstruction plate. Acromioclavicular joint wire cerclage in a figure-eight pattern and an endobutton placed arthroscopically.
Medial third clavicle fractures associated with posterior dislocation of the distal clavicle present a diagnostic and therapeutic challenge. Initial clinical evaluation with standard radiographs can be misleading, making advanced imaging (3D CT) essential for confirming the diagnosis [5]. Conservative treatment may be appropriate for stable fractures; however, in our case, the progression of deformity and confirmation of posterior dislocation necessitated surgical intervention to ensure optimal functional recovery and prevent long-term complications [6]. This case highlights the importance of thorough clinical and radiological evaluation, with advanced imaging in cases of suspected complex dislocations. Close radiological follow-up is crucial to monitor fracture evolution and clavicular stability. Timely surgical intervention is recommended in cases of progressive deformity and joint instability, which can be performed through open surgery or arthroscopically using simple wires and/or endobuttons [7,8,9]. The patient underwent surgery with a favorable post-operative outcome and a rehabilitation protocol aimed at complete functional recovery [10] (Fig. 5). After a 6-month follow-up, the patient had excellent results for shoulder range of motion and function. The patient’s Constant-Murley score is 92.
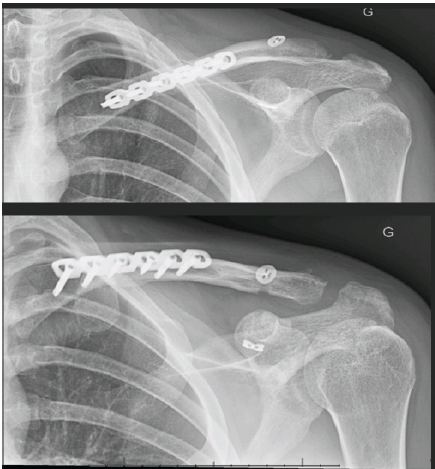
Figure 5: Post-operative radiographic control.
A medial clavicle fracture caused by high-energy trauma should always raise suspicion for a concomitant ACJ dislocation. Due to the rarity and complexity of this combined injury, a thorough clinical and radiological assessment is crucial for accurate diagnosis and appropriate treatment planning. Standard radiographs may not always reveal the full extent of the injury; therefore, advanced imaging modalities, such as a shoulder CT scan, are essential to confirm the diagnosis and guide surgical management. Early identification and appropriate intervention can significantly improve functional outcomes and reduce the risk of long-term complications.
In this type of high-energy trauma, early identification and appropriate intervention can significantly improve functional outcomes, reduce the risk of long-term complications, and prevent missed posterior acromioclavicular joint instability.
References
- 1. Gumina S, Carbone S, Polizzotti G, Paglialunga C, Preziosi Standoli J, Candela V. The rare medial-end clavicle fractures: Epidemiological study on inhabitants of a Suburban Area. Cureus 2021;13:e18008. [Google Scholar] [PubMed]
- 2. Pallis M, Cameron KL, Svoboda SJ, Owens BD. Epidemiology of acromioclavicular joint injury in young athletes. Am J Sports Med 2012;40:2072-7. [Google Scholar] [PubMed]
- 3. Nordin JS, Olsson O, Lunsjö K. Acromioclavicular joint dislocations: Incidence, injury profile, and patient characteristics from a prospective case series. JSES Int 2020;4:246-50. [Google Scholar] [PubMed]
- 4. Ottomeyer C, Taylor BC, Isaacson M, Martinez L, Ebaugh P, French BG. Midshaft clavicle fractures with associated ipsilateral acromioclavicular joint dislocations: Incidence and risk factors. Injury 2017;48:469-73. [Google Scholar] [PubMed]
- 5. Mantripragada S, Peh WC. Spectrum of lesions of the acromioclavicular joint: Imaging features. Singapore Med J 2022;63:130-9. [Google Scholar] [PubMed]
- 6. Putnam M, Vanderkarr M, Nandwani P, Holy CE, Chitnis AS. Surgical treatment, complications, and reimbursement among patients with clavicle fracture and acromioclavicular dislocations: A US retrospective claims database analysis. J Med Econ 2019;22:901-8. [Google Scholar] [PubMed]
- 7. Shih YJ, Chang HC, Wu CL. Optimizing treatment for combined midshaft clavicle fracture and acromioclavicular joint injury: A case study highlighting the efficacy of knowles pin fixation. Am J Case Rep 2023;24:e939325. [Google Scholar] [PubMed]
- 8. Cunningham G, Culebras Almeida LA, Gauthier M. All-suture technique for fixation of unstable displaced distal clavicle fracture. JSES Rev Rep Tech 2022;2:168-73. [Google Scholar] [PubMed]
- 9. Gao Z, Cai P, Yao K, Long N, Liu L, Xiao C. Mid-clavicle fracture with dislocation of the ipsilateral acromioclavicular joint treated with Endobutton system: A case report and review of the literature. Medicine (Baltimore) 2021;100:e27894. [Google Scholar] [PubMed]
- 10. Cote MP, Wojcik KE, Gomlinski G, Mazzocca AD. Rehabilitation of acromioclavicular joint separations: Operative and nonoperative considerations. Clin Sports Med 2010;29:213-28, vii. [Google Scholar] [PubMed]