Recurrent acromioclavicular joint ganglion cysts in elderly patients can be effectively managed using a minimally invasive double-loop suture (threading) technique, offering a safe, low-cost outpatient alternative to surgery with minimal morbidity and reduced risk of recurrence.
Dr. Prannoy Paul, Department of Orthopaedics, M.O.S.C Medical College Hospital, Kolenchery, Ernakulam, Kerala, India. E-mail: prannoypaul@gmail.com
Introduction: Acromioclavicular (AC) joint cysts are rare cysts often linked to degenerative shoulder issues. Although recurrence can limit treatment success, aspiration and corticosteroid injections are commonly used. Surgical removal is effective but may not be suitable for older patients or those with financial constraints. A minimally invasive double-loop suture technique offers a promising alternative.
Case Report: An 80-year-old woman experienced painless swelling in her right AC joint measuring 8 × 5 cm for 4 months, as well as restricted shoulder movement and a 15-year history of falling. After a triamcinolone injection and aspiration, the cyst returned within a month. A clinical exam revealed a soft, movable, non-tender ganglion cyst. The outpatient procedure used a minimally invasive double-loop suture technique, placing two non-absorbable silk sutures perpendicularly through the cyst for drainage. Post-procedure care involved only a compression dressing, with no medications needed. Results: The procedure lasted 10 min and was completed without complications. The patient experienced no immediate complications. The cyst resolved completely at 6 months and we are tracking long-term results and recurrence potential.
Conclusion: The double loop suturing technique is a simple and affordable outpatient treatment for recurrent AC joint cysts, especially for older patients or when surgery is not an option. It may lead to lower recurrence rates and is less invasive and less expensive than the surgical excision.
Keywords: Ganglion cyst, acromioclavicular, elderly.
Acromioclavicular (AC) joint ganglion cysts are rare benign swellings that typically arise secondary to degenerative changes within the AC joint or chronic rotator cuff pathology. These cysts often occur when synovial fluid from the glenohumeral joint tracks superiorly through a degenerative capsular defect, producing a unidirectional “check-valve” mechanism and subsequent cyst formation. Although many AC joint cysts are asymptomatic, they may present with pain, cosmetic concerns, and functional limitations, particularly in elderly individuals who are more prone to rotator cuff degeneration and AC joint arthropathy [1]. Management remains challenging, as currently available treatment options demonstrate varying success and recurrence rates. Simple aspiration is frequently attempted due to its minimally invasive nature; however, recurrence rates remain alarmingly high – reported between 70 and 90% – because the underlying cyst wall and joint communication are not addressed [2]. Corticosteroid injections may offer temporary symptomatic relief but carry risks, such as skin atrophy and hypopigmentation, especially in older adults, and their overall efficacy remains limited in communicating cysts [3,4]. Surgical excision, though effective, involves hospitalization, anesthesia risks, and extended recovery, which may not be ideal for elderly or medically fragile patients [5]. Arthroscopy allows simultaneous treatment of intra-articular pathology but requires specialized resources that may not be readily available in all settings [5,6]. Alternative minimally invasive techniques, such as threading – traditionally used for wrist ganglion cysts – have recently gained attention for their simplicity, cost-effectiveness, and promising recurrence outcomes [7,8,9].
An 80-year-old female, came to our outpatient clinic with a painless swelling near her right AC joint that had been gradually increasing in size over the past 4 months. Although she experienced shoulder pain for the past 10–15 years, there were no signs of infection, redness, or any systemic problems. She also gave no history of any evening rise of temperature or weight loss. She denied any history of high blood pressure, or diabetes. She had a history of a fall at home 15 years back, sustained a fracture to the shoulder bone and took treatment from a local bonesetter for the same. She was treated with a massage and bandage, but had on-and-off pain following that injury. Her day-to-day activities, such as wearing clothes and combing hair, were limited, but she has no complaints regarding this; she was living on with it. Previously, she had undergone aspiration and received an intralesional injection of triamcinolone (Kenacort) from outside the hospital, but the cyst returned within a month.
Clinical examination
On examination, a soft and mobile lump was noted around the right AC joint, measuring approximately 8 × 5 cm, suggesting the potential presence of a ganglion cyst (Fig. 1a and b). The skin in that area looked normal, and there were no indications of neurovascular problems in the right arm. The active range of motion for the right shoulder was significantly restricted.
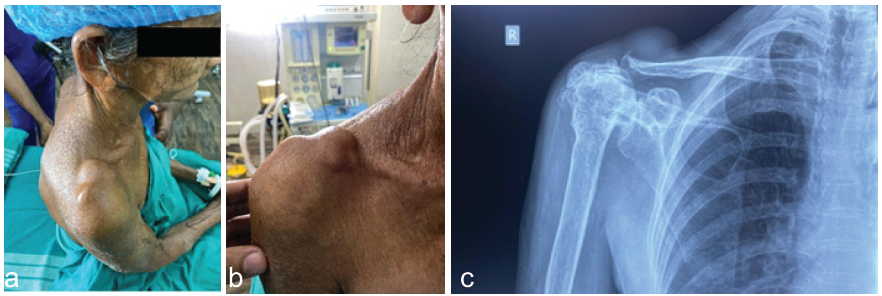
Figure 1: (a, b, c) Pre-operative.
- Abduction: 30–50°
- Flexion: 40–60°
- Extension: 20–30°
- Internal rotation: 20–40°
- External rotation: 10–30°
Investigations
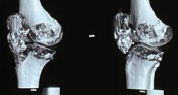
X-ray showed degenerative changes in the AC and glenohumeral joint. Deformed and decreased Humer acromial interval (Fig. 1c).
All routine blood investigations, including infection-related parameters (complete blood count, erythrocyte sedimentation rate, C-reactive protein), were within normal limits.
Management and procedure
A day care outpatient procedure was planned and performed, lasting around 10 min. The patient was seated with their elbow flexed at 90° and turned inward. Adhering to strict aseptic techniques, the right shoulder area was cleaned, disinfected, and draped. The cyst’s outline was marked with a sterile marker. A No. 1 silk suture was threaded through a cutting needle and inserted into one side of the cyst, emerging from the opposite side. The thick, yellowish, jelly-like fluid observed upon entry indicated that access to the ganglion was successful. The same suture was then re-threaded back through the cyst in the reverse direction, creating a loop within the cyst. Subsequently, a second suture was introduced perpendicularly in a similar manner, again forming a loop inside the cyst in orthogonal directions, forming a cross-stitch pattern to guarantee complete decompression. Once the cystic fluid was drained, a sterile gauze was positioned over the site, and the sutures were secured (Fig. 2a and b).
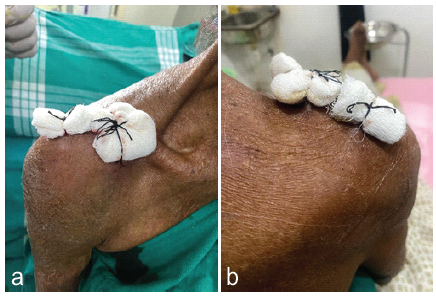
Figure 2: (a and b) Intraoperative.
Subsequently, a compression bandage was applied. The patient did not receive any antibiotics or anti-inflammatory drugs and was instructed to come back on the 10th day of suture removal and later if experienced considerable pain or if the cyst returned. Day 10 follow-up showed no signs of infection (Fig. 3a and b). The 6-month follow-up revealed no recurrence, an excellent outcome, and wound healing (Fig. 4a and b).
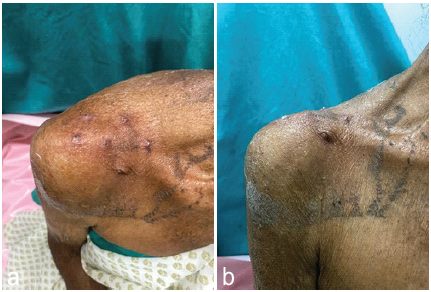
Figure 3: (a and b) Days of follow-up.

Figure 4: (a and b) 6 month Follow-up.
A very rare lesion, AC joint ganglion cysts can develop as a result of AC joint degeneration or chronic rotator cuff disease. They might enhance synovial fluid tracking by connecting to the glenohumeral joint through a degenerative pathway. Especially in elderly individuals, these cysts can lead to pain, esthetic concerns, and functional difficulties, while being benign and mostly asymptomatic [1]. A variety of treatment options have been utilized for AC joint ganglion cysts, resulting in differing outcomes and recurrence rates. The most common initial treatment is simple aspiration, favored for its non-invasive and straightforward nature. However, because aspiration does not tackle the cyst wall or the underlying joint problems, recurrence rates can soar to 70–90% [2]. Administering corticosteroids after aspiration aims to decrease inflammation and lower the chances of recurrence. Although this approach offers slight improvement over aspiration alone, the relationship between the cyst and the joint limits its overall effectiveness. Furthermore, repeated steroid injections can cause skin thinning and pigmentation loss, especially in older patients [3,4]. In our experience, combining aspiration with corticosteroid injection resulted in a recurrence within just 1 month. In cases where cysts are symptomatic or ongoing, or when there is rotator cuff tear arthropathy, surgical removal is recommended. This operation requires hospitalization and comes with anesthesia-related risks, particularly for elderly patients. Furthermore, it entails a longer recovery time and the risk of infection or harm to nearby tissues. If the communication within the glenohumeral joint is not effectively addressed, there is a chance of recurrence [5]. Arthroscopy improves the ability to visualize and treat intra-articular issues, particularly when rotator cuff injuries are also present. This technique demands specialized instruments and skills, and may not be necessary for straightforward, non-communicating ganglion cysts [5,6]. The minimally invasive threading method applied in this case involved the insertion of silk sutures into the cyst to facilitate controlled decompression and drainage. This approach is akin to traditional treatments for dorsal wrist ganglion cysts, particularly in rural or resource-constrained settings, and has shown encouraging outcomes [7]. It enables complete removal of cystic material, minimizes inflammation, and decreases the likelihood of fibrosis and recurrence. In addition, it eliminates the need for general anesthesia or extensive operating room time, avoids pharmacological interventions that could lead to side effects, and is cost-effective while ensuring high patient comfort, especially for elderly individuals. As an outpatient procedure, it promotes a swift return to everyday activities [8,9]. The patient underwent a minimally invasive, threading procedure due to specific clinical and individual factors. One month following aspiration and corticosteroid injection, the cyst reappeared. The integrity of the cyst wall and the communication with the joint may hinder long-term relief from conservative treatments. Although there are procedural risks, the 80-year-old patient did not have any significant comorbidities. Less invasive options are preferable for elderly patients compared to surgical excision or arthroscopic procedures, which would require hospitalization, anesthesia risks, longer recovery times, and other complications. While the swelling was not dangerous, it caused cosmetic concerns and mild pain that necessitated treatment. Threading provided a safe way to restore comfort and appearance without hospitalization or trauma. It effectively achieved complete and controlled cyst decompression. The crisscrossed double loop silk sutures help expel the cyst contents and induce low-grade inflammation in the cyst wall, leading to fibrosis and the collapse of the cyst cavity, thereby minimizing the chances of recurrence. This 10-min outpatient procedure is both cost-effective and resource-efficient, as it does not require specialized equipment, incisions, or postoperative medications. It is particularly beneficial in rural or low-resource healthcare environments where advanced surgical options are limited. Threading, which involves continuous drainage through suture insertion, facilitates the gradual decompression and epithelialization of the cyst tract, functioning as a controlled fistula. A study by Kim et al. demonstrated that using chromic catgut-guided ultrasonography for threading could eliminate 90% of cysts with minimal recurrence even after a year [10]. Similarly, Jiang et al. reported a case of a recurring AC joint ganglion that was effectively treated on an outpatient basis using nylon threading, with no signs of recurrence at the 6-month follow-up [11]. Based on these findings, our case utilized the threading technique (Silk No. 1) to ensure sustained drainage and the collapse of the cyst cavity, employing a non-absorbable silk suture. While this method has proven effective for managing fistulas and ganglion cysts around the wrist, its application for AC joint cysts is not widely documented, leaving us to speculate on its safety and efficacy in chronic fluid collections [12]. Our case adds to the limited but expanding research suggesting that the threading technique may offer advantages over surgical options for some patients. Further studies with larger sample sizes and long-term follow-ups are needed to standardize methods and compare outcomes across different suture materials and cyst causes. In our patient, the procedure was successfully tolerated, did not necessitate any post-surgery medication, and allowed for a quick discharge with just a compression bandage and simple guidelines. Focusing on patient-centered care enhances adherence, recovery, and overall satisfaction.
Treating recurrent AC joint cysts can be challenging, especially for older patients who cannot undergo surgery. The Seton suturing technique offers a simple, minimally invasive, and cost-effective solution with minimal discomfort and no immediate complications. This outpatient method is a viable alternative to aspiration with corticosteroid injections, which have a high recurrence rate. In low-resource settings or for patients unfit for surgery, the Threading technique may be beneficial. More research is needed to confirm its long-term effectiveness and recurrence rates.
A minimally invasive double-loop (threading) suture technique offers a simple, cost-effective outpatient solution for recurrent acromioclavicular joint ganglion cysts, particularly in elderly patients unfit for surgery. It provides effective cyst decompression with low morbidity and may reduce recurrence compared to aspiration and steroid injection.
References
- 1. Schutz JF, Hamad CD, Russell MD, Abdeljaber M, Nelson SD, Eilber F. Acromioclavicular joint cyst presenting with findings concerning for a soft tissue tumor – a case report. Diagn Pathol 2024;19:156. [Google Scholar] [PubMed]
- 2. Tham SY, Ng PH, Phua SK, Ho SW. Aspiration of a large acromioclavicular joint cyst complicated by recurrence and enlargement: A case report. Cureus 2023;15:e34754. [Google Scholar] [PubMed]
- 3. Tiwari A, Soni R. Insights into acromioclavicular joint ganglionic cyst: Diagnosis and management. Int J Res Orthop 2024;10:1411-4. [Google Scholar] [PubMed]
- 4. Sinha MK, Mishra P, Mishra TS, Barman A. Aspiration and steroid injection in ganglion cysts: An ultrasound guided evaluation of the response. J Clin Orthop Trauma 2019;10:S252-7. [Google Scholar] [PubMed]
- 5. Kajita Y, Iwahori Y, Harada Y, Takahashi R, Deie M. Arthroscopic treatment of massive acromioclavicular joint ganglion cysts with color-aided visualization: A case series of 4 patients. JSES Rev Rep Tech 2022;2:526-34. [Google Scholar] [PubMed]
- 6. Chaudhari T, Gupta A. Acromioclavicular ganglion cyst: A rare case report. Cureus 2024;16:e54089. [Google Scholar] [PubMed]
- 7. Chaudhary S, Mandal S, Kumar V. Results of modified thread technique for the treatment of wrist ganglion. J Clin Orthop Trauma 2021;13:57-62. [Google Scholar] [PubMed]
- 8. Balke M, Wafaisade A, Hoeher J, Greshake O. Minimally invasive reconstruction of acute acromioclavicular joint injuries using the TwinBridge button system. Eur J Orthop Surg Traumatol 2023;33:1349-55. [Google Scholar] [PubMed]
- 9. Breuer R, Unterrainer A, Komjati M, Tiefenboeck TM, Trieb K, Pirkl C. Minimally invasive AC joint reconstruction system (MINAR(®)) in modified triple-button technique for the treatment of acute AC joint dislocation. J Clin Med 2019;8:1683. [Google Scholar] [PubMed]
- 10. Kim YJ, Lee SH, Bae JH. Minimally invasive threading for ganglion cysts: An alternative to surgery. J Shoulder Elbow Surg 2019;28:e98-103. [Google Scholar] [PubMed]
- 11. Jiang Y, Tan J, Zheng C. Successful treatment of recurrent AC joint ganglion cyst using suture threading: A case report. Case Rep Orthop 2020;2020:1-4. [Google Scholar] [PubMed]
- 12. Malik AI, Nelson RL. Surgical management of anal fistulae: A systematic review. Colorectal Dis 2008;10:420-30. [Google Scholar] [PubMed]