To describe a novel technique in acute patellar tendon repair.
Dr. Anzano Francesco, Department of Orthopaedics, IRCCS Ospedale S. Raffaele, Milan, Italy E-mail: anzano.francesco@hsr.it
Introduction: Patellar tendon rupture is a serious injury affecting the knee extensors and often requires surgical repair with graft augmentation, which lengthen return to sports not sooner than 6 months.
Case Report: We, hereby, describe a case of an active male presenting with sudden knee pain and inability to flex the knee during a soccer match. Clinical examination and imaging were positive for complete patellar tendon rupture. Surgical treatment consisted of tendon repair and side-to-side augmentation with Gore-Tex membrane. Weight-bearing was allowed from day 1, knee flexion after 1 month, and weightlifting and running after 2 months. In 3 months, return to sport was achieved, a time shorter with respect to conventional techniques.
Conclusions: This case report highlights the possibility of shorter return to sport with this new technique.
Keywords: Patellar tendon rupture, augmentation, Gore-Tex membrane.
Patellar tendon rupture is a rare but serious injury affecting the knee extensor mechanisms [1]. It is most commonly found in active men in their 30–50s, and 6 months are expected before return to play [2]. The mechanism of tendon rupture often involves forced contraction of the knee in a flexed position, but it may also arise from systemic conditions, such as diabetes, chronic tendinopathies, and use of antibiotics, in which cases of bilateral tendon rupture have been reported [3]. Diagnosis is clinical, with inability to flex the knee, and imaging may help in defining the extent of the lesion or the presence of associated soft-tissue injuries [4]. Several techniques have been described for the treatment of patellar tendon rupture, often using non-absorbable sutures to reapproximate the tendon sides as well as augmentation with semitendinosus and gracilis through bone tunnels. This technique is effective in chronic tendon repair [5,6] but involves the use of bone tunnels and autologous grafts, which are detached from their original sites and may require prolonged time to heal and limit prompt return to play. The following case involves a patient with acute patellar tendon rupture treated with augmentation with Gore-Tex membrane. Gore-Tex membranes are made of polyglycolic acid, and their mechanics have been studied in in vivo models for tendon rupture with properties similar to the native tendon [7]. We, therefore, decided to adopt this membrane for tendon repair. To the best of our knowledge, no previous cases of tenorrhaphy with Gore-Tex membrane have been reported.
We present the case of an active male in his early 30s admitted to the emergency department for acute pain with an inability to flex his left knee after performing a jump in a soccer match. His medical history was negative presented no comorbidities, no corticosteroid injections nor recent antibiotic use. His weight was 78 kg and his height was 185 cm (Body mass index 22.8). He practices soccer 3 times a week in a local team as an amateur. He was referred for orthopedic consult. He presented with a painful, swollen knee, inability to knee flexion, and a palpable gap at the level of patellar tendon (Fig. 1).

Figure 1: Palpable patellar tendon gap at presentation.
Patellar tendon rupture was diagnosed and confirmed by an abnormally high patella on X-rays and by echography, which showed a complete tendon rupture with a 32 mm gap between the two tendon sides. Patient consent for surgical treatment was obtained, and surgery was performed 7 days after the trauma.
Under subarachnoid anesthesia, surgery was performed in the supine position. A tourniquet was applied for the whole procedure. Bone marrow aspiration was taken from the iliac crest and put in the bone marrow aspirate concentrate (BMAC) centrifuge. A parapatellar incision was performed, and total patellar tendon rupture was reported (Fig. 2).

Figure 2: Intraoperative finding of complete patellar tendon tear.
Notably, also the medial and lateral capsule was teared. First, the tendon sides were attached using non-absorbable sutures, and the anteromedial and anterolateral capsules were reconstructed using the same sutures (Fig. 3).
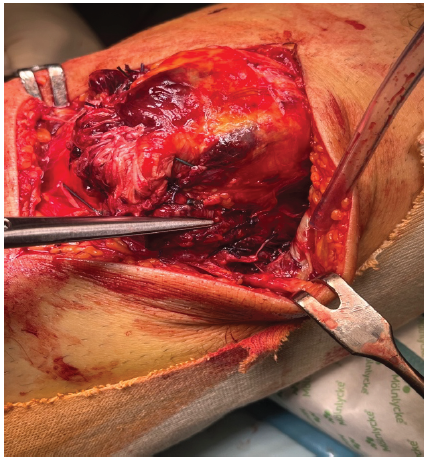
Figure 3: Tenorrhaphy and reconstruction of anteromedial and anterolateral capsule.
Subsequently, with the knee flexed at 30°, a tubular GORE® stretch Vascular Graft (Newark, New Jersey, US) was prepared. First, it was passed from medial to lateral into the quadriceps tendon and secondly attached with non-absorbable sutures at paratendinous sides (Fig. 4).
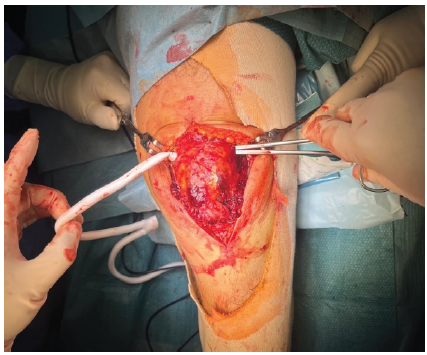
Figure 4: Insertion of the Gore-Tex membrane into quadriceps tendon.
The membrane was then tightened and attached at the level of the tibial tuberosity with intraosseous stitches, without the need of anchors or bone tunnels (Fig. 5).
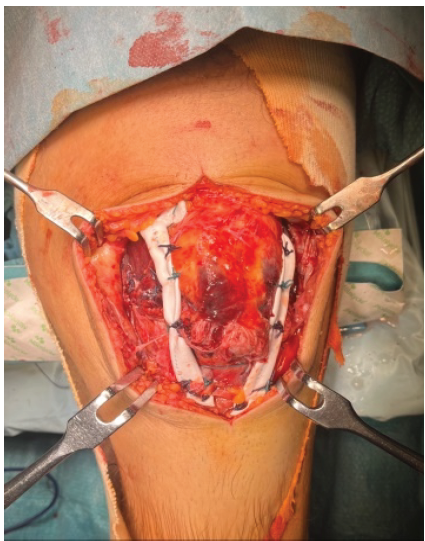
Figure 5: Gore-Tex membrane fixation and tendon augmentation.
The construct was tested at different degrees of flexion, with no instability reported, and finally, BMAC was injected into the knee (Fig. 6).

Figure 6: Intra-articular bone marrow aspirate concentrate injection at the end of the procedure.
The remaining layers were then sutured, and a brace fixed in extension was put on for the subsequent month. The patient was allowed for weight-bearing from post-operative day 1. 30 days after surgery, the brace was removed, and passive and active flexion was initiated. At the 2-month follow-up, the patient showed an almost complete of movement, good patellar tendon function, and no complaints from the surgical procedure (Fig. 7). At this point, weight-bearing exercises and running was encouraged. Return to play was allowed from day 90 with no impairment.

Figure 7: Knee flexion at 2-month follow-up, weight lifting, and running were encouraged at this point.
Patellar tendon ruptures are rare but serious injuries that impair patient activity for a prolonged time. Several effective techniques have been described, but almost all involve autografts and bone tunnels, which allow for return to sports not sooner than 6 months. In the presented case, we used the GORE® stretch Vascular Graft since it is biocompatible, as well as strong, conformable, and easy-to-handle, to avoid the need for autografts. This method provided good overall results and prompt return to sport with respect to standard techniques. Augmentation using allografts including bioinductive collagen patch [8] or synthetic ligament [9] has been described. To the best of our knowledge, there are no described cases in the literature of the use of vascular membranes for repairing patellar tendons. In this case, anteromedial and anterolateral capsule were rupture and need reconstruction to avoid potential complications including patellar dislocation. During the procedure, BMAC was also injected, as it has been proven to ameliorate symptoms and provide immunomodulatory effects [10] decelerating knee osteoarthritis. This type of treatment may also have some limitations, including the high cost of the graft and the potential risk of host versus graft reactions. In addition, the patient was treated acutely with tenorrhaphy and augmentation, a treatment that is often reserved for chronic tendon rupture, while tenorrhaphy alone is often the method of choice for acute tendon rupture. The use of BMAC may, however, have contributed to hastening the good results of this report. The good results at three follow-ups encouraged us to reproduce this technique also in future case, possibly without the need of knee bracing after surgery. We, hence, deem that further studies and applications of Gore-Tex membranes for acute and chronic patellar tendon augmentation may help in evaluating this technique as an effective method for young, active patients to provide prompt return to sport.
In the presented case, we highlighted the possibility of using a novel technique for the surgical repair of patellar tendon. The promising initial results and the prompt return to sport provided interest in utilizing this technique for further cases.
Treating acute patellar tendon rupture with a new technique.
References
- 1. Arras C, Ksrause M, Frosch KH. Die Quadrizepssehnen- and Patellarsehnenruptur [Quadriceps Tendon and Patellar Tendon Rupture]. Z Orthop Unfall 2025;163:181-94. [Google Scholar] [PubMed]
- 2. Brinkman JC, Reeson E, Chhabra A. Acute patellar tendon ruptures: An update on management. J Am Acad Orthop Surg Glob Res Rev 2024;8:e24.00060. [Google Scholar] [PubMed]
- 3. Fernandes A, Rufino M, Hamal D, Mousa A, Fossett E, Cheema KS. Simultaneous bilateral patellar tendon rupture: A systematic review. Cureus 2023;15:e41512. [Google Scholar] [PubMed]
- 4. Enad JG. Patellar tendon ruptures. South Med J 1999;92:563-6. [Google Scholar] [PubMed]
- 5. Valianatos P, Papadakou E, Erginoussakis D, Kampras D, Schizas N, Kouzoupis A. Treatment of chronic patellar tendon rupture with hamstrings tendon autograft. J Knee Surg 2020;33:792-7. [Google Scholar] [PubMed]
- 6. Kovacev N, Antić J, Gvozdenović N, Obradović M, Vranješ M, Milankov M. Patellar tendon rupture–treatment results. Med Pregl 2015;68:22-8. [Google Scholar] [PubMed]
- 7. Yokoya S, Mochizuki Y, Nagata Y, Deie M, Ochi M. Tendon-bone insertion repair and regeneration using polyglycolic acid sheet in the rabbit rotator cuff injury model. Am J Sports Med 2008;36:1298-309. [Google Scholar] [PubMed]
- 8. Daniel AV, Rechter GR, Reed LA, Williams WA, Carbone AD, Kannan AS. Patellar Tendon Repair With Bioinductive Implant Augmentation. Arthrosc Tech 2025;14:103639. [Google Scholar] [PubMed]
- 9. Core M, Anract P, Raffin J, Biau DJ. Traumatic patellar tendon rupture repair using synthetic ligament augmentation. J Knee Surg 2020;33:804-9. [Google Scholar] [PubMed]
- 10. Vitali M, Ometti M, Pironti P, Salvato D, Sandrucci A, Leone O, et al. Clinical and functional evaluation of bone marrow aspirate concentrate vs autologous conditioned serum in the treatment of knee osteoarthritis. Acta Biomed 2022;93:e2022222. [Google Scholar] [PubMed]







