TB arthritis of the knee is rare and difficult to diagnose, particularly in cases with a low index of suspicion. In young and healthy patients not recovering from knee injuries as expected, further diagnostic testing is warranted to exclude rare forms of arthritis, such as TB, despite low incidence rates in developed countries. Early diagnosis and treatment of TB in the knee joint are linked to favorable outcomes, whereas delays can incur significant and irreversible joint damage.
Dr. Nicolaas Kotze, Department of Orthopaedics, Connolly Hospital Blanchardstown, Dublin, Ireland, D15X40D. E-mail: nicolaasleonkot24@rcsi.com
Introduction: Tuberculosis (TB) arthritis, particularly in the knee, is a rare condition with significant diagnostic challenges, especially in regions with low TB incidence. This case report presents the first documented instance of native knee TB arthritis in Ireland, highlighting the necessity for increased awareness and a multidisciplinary approach in diagnosing this uncommon disease.
Case Report: A 27-year-old healthy male, originally from India, and living in Ireland, presented with non-specific left knee pain for 3 weeks, initially diagnosed as a soft-tissue injury. After a subsequent traumatic left patellar fracture that required surgical fixation, his recovery was complicated by persistent knee swelling and limited range of motion. Following 12 months of delayed recovery, all implants were removed from his knee, and physiotherapy was initiated. When he was still symptomatic 10 months later, further investigations were required. Higher-order imaging revealed marked degenerative changes in the knee joint along with extensive synovitis. Following multidisciplinary team input, he underwent biopsies of his tibial plateau as well as synovial tissue and joint fluid. Histology of tissue demonstrated granulomata, and anti-tuberculous therapy was initiated before tissue culture from the index biopsy later confirmed Mycobacterium TB (MTB). Clinical response to treatment was marked, with improvement in symptoms and functionality. After completing the course of treatment, the patient had another setback when he sustained a comminuted left distal femur fracture following a low-trauma fall. During the open reduction and internal fixation for this fracture, tissue samples taken intraoperatively confirmed complete resolution of granulomatous inflammation. Intraoperative tissue was culture negative for MTB. This confirms successful microbiological and clinical cure of the infection.
Conclusion: This report underscores the critical importance of considering TB arthritis in patients with persistent knee pain, particularly in patients who have migrated from high-incidence countries. It provides insight into the diagnostic complexities and emphasizes the role of tissue biopsy for histological analysis and mycobacterial tests in confirming the diagnosis. The findings from this case contribute significantly to the orthopedic literature and foster awareness of TB arthritis, advocating for timely diagnosis and interdisciplinary cooperation in managing rare diseases.
Keywords: Tuberculosis, arthritis, knee, diagnosis.
Tuberculosis (TB) is an ancient infectious disease that has accompanied humanity since the Neolithic period. Archeological evidence shows human remains dating back over 8000 years that exhibit bony alterations consistent with TB infection. Genetic analyses indicate that Mycobacterium TB (MTB), the causative agent, has undergone minimal evolutionary changes since that time [1]. Historical references to TB are prevalent across multiple cultures, spanning from ancient civilizations through the Middle Ages into the Renaissance. Robert Koch’s isolation of the tubercle bacillus in 1882 marked a significant milestone in understanding and treating TB [2]. The World Health Organization estimates 10.8 million TB diagnoses worldwide in 2023, highlighting distinct geographical variation. Southeast Asia has a ten-fold higher incidence compared to Europe (200–300 vs. 20–30/100,000 annually) [3]. In Ireland, 289 cases were notified in 2024 (5.6/100,000), with 72% of those occurring in individuals born outside of Ireland [4]. According to the 2022 census, approximately 150,000 individuals in Ireland are citizens of Asia and Africa, regions with significantly higher TB incidence than Europe [5].
Musculoskeletal (MSK) TB is rare, usually resulting from reactivation of latent hematogenously disseminated infection. MSK TB accounts for approximately 2–3% of all TB cases in the United States. A regional study from Los Angeles County, USA, reported that TB arthritis of the knee constituted 13% of all MSK TB cases [6]. Magnetic resonance imaging (MRI) is important for identifying areas of abnormality to be targeted for diagnostic biopsy. Bone edema, joint effusion, and synovial thickening are commonly seen. It can demonstrate hypointense areas indicative of necrotic tissue, alongside hyperintense fluid collections and “rice bodies,” which are small low-signal intensity nodules in the joint fluid [7]. A multi-faceted diagnostic approach, including MRI, biopsy, and aspiration for microscopy, histology, culture, and nucleic acid amplification testing in suspected MSK TB cases, is recommended [6].
Initial presentation
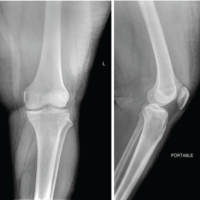
A man in his 20s who immigrated to Ireland from India reported non-specific knee pain. He had no significant medical history, and the episode was diagnosed as a soft-tissue injury, for treatment with non-steroidal anti-inflammatory medication. He presented to the Emergency Department 1 year later after a fall and hyperextension injury to his left knee. A displaced transverse fracture of the patella was confirmed on X-ray imaging. The initial laboratory investigations were normal, including an erythrocyte sedimentation rate (ESR) of 10 mm/h, a white blood cell count of 10.9 × 109/L, and a C-reactive protein (CRP) of 3 mg/L. The patient underwent open reduction and internal fixation using tension band wiring 4 days after the injury, and the surgery was uncomplicated. However, outpatient recovery was slower than anticipated, with persistent knee swelling. Range of motion remained limited to an arc of 10–90° despite adequate physiotherapy and rehabilitation. Given these issues, a decision was made to remove the implants 12 months after the initial surgery. All implants were removed without complications, and there were no abnormal findings intraoperatively. Upon re-evaluation in the outpatient department, the patient exhibited persistent knee swelling but no tenderness. Knee flexion to 110° was possible, and although quadriceps muscle wasting was noted, he managed to perform a straight leg raise (SLR). X-rays showed a healing patellar fracture without articular surface involvement, as shown in Fig. 1. He was discharged for ongoing community physiotherapy.
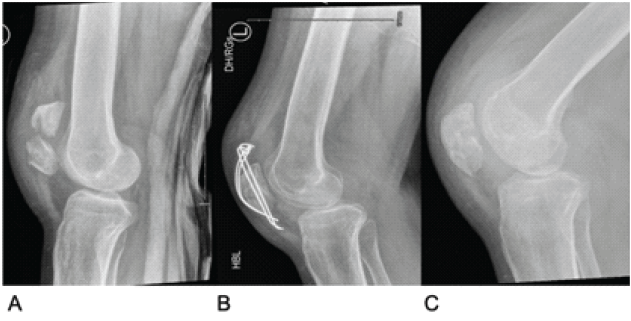
Figure 1: Lateral X-ray images of the left knee. (a) Initial fracture. (b) Tension band wiring. (c) After the removal of metal.
Re-presentation
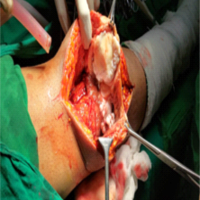
After experiencing persistent knee pain, swelling, and reliance on a crutch for mobility, he was referred back to the orthopedic outpatient clinic. Eight months after the removal of implants, examination demonstrated minimal tenderness but substantial joint effusion and an inability to sustain SLR. This raised the possibility of a partial quadriceps muscle rupture. Inflammatory markers were normal (white cell count 5.3 × 109/L, CRP 6 mg/L). An MRI performed at that time excluded a quadriceps rupture, noting joint effusion, synovitis, and degenerative changes in the tibial plateaus and femoral condyles. Unfortunately, the absence of pain, normal inflammatory markers, and lack of systemic features of infection were falsely reassuring, and MRI changes were attributed to post-traumatic degenerative changes. He was referred for quadriceps strengthening physiotherapy with an emphasis on gradual progression. The patient returned with knee pain, joint effusion, and ongoing limited knee extension 3 months later. Repeat blood work again showed no acute inflammatory changes (ESR 18 mm/h, white cell count 5.6 × 109/L, CRP 7 mg/L). A subsequent MRI (Fig. 2) revealed extensive tricompartmental knee arthritis with joint space narrowing, chondral loss, subarticular geodes, and significant subchondral bone marrow edema, along with a collection in the gastrocnemius.
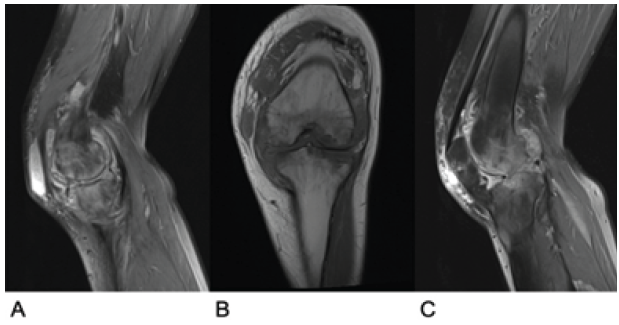
Figure 2: Magnetic resonance imaging scan of the left knee (a) Sagittal view of the medial tibial joint space. (b) Coronal view of the centre of the knee joint. (c) Sagittal view of the lateral tibial plateau
These findings, along with accompanying effusion and synovitis, raised the possibility of infective arthropathy.
He underwent arthroscopy, joint aspiration, and synovial biopsy. The procedure confirmed significant degenerative changes and thickened synovium and was ultimately abandoned due to poor visibility. Standard bacterial cultures from the aspirated fluid did not grow any organisms, but histological examination indicated a florid histiocytic reaction. Infectious diseases review was requested, and a multidisciplinary discussion prompted repeat synovial as well as bone marrow biopsies, via interventional radiology, for histopathological examination and mycobacterial investigations. Histological analysis of tibial bone marrow biopsies revealed granulomas, whereas synovial tissue showed lymphoplasmacytic infiltrate and necrotic debris. Ziehl–Neelsen (ZN) staining was negative for all samples. Anti-tuberculous therapy (ATT) was commenced in the infectious diseases clinic on the basis of the histological findings, while awaiting culture results. Intensive phase ATT comprised rifampicin, isoniazid, and pyrazinamide with pyridoxine in addition. Levofloxacin was substituted for ethambutol before culture confirmation of MTB, in case a potential bacterial low-grade infection related to previous hardware might be at play. Synovial fluid cultured MTB after 26 days in a mycobacterial growth indicator tube system. At this point, the patient had been taking ATT for 2 weeks. Tests for human immunodeficiency virus, hepatitis B, and hepatitis C were negative, and a chest X-ray revealed no signs of pulmonary TB. The patient experienced significant symptom relief within the first 2 weeks of treatment, which accelerated after the addition of a steroid. After drug susceptibility testing confirmed pan-susceptible MTB, ATT was rationalized to the consolidation phase with rifampicin + isoniazid, and he completed 6 months of therapy without complication. Systemic steroids were re-initiated midway through ATT after improvement plateaued, each time with a significant clinical response. By completion of ATT, he had marked improvement in pain and mobility, allowing him to walk unassisted and ride his bicycle for the 1st time in nearly 2 years.
Subsequent setback
Three months after completing TB treatment, he sustained a comminuted fracture of the left distal femur following a fall resulting in excessive valgus force on the knee, as shown in the X-ray images in Fig. 3. A computed tomography scan (Fig. 4) raised concern over marrow sella tissue density and calcifications at the fracture site, suggesting an underlying lesion. Blood work during this period returned normal results (white cell count 8.7 × 109/L, CRP 3 mg/L).
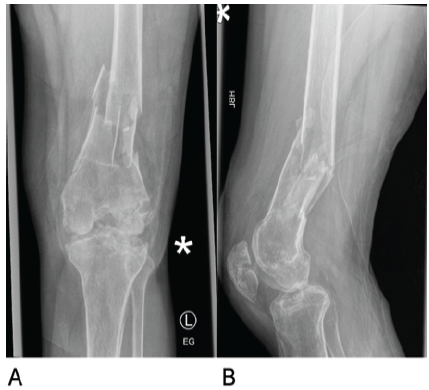
Figure 3: X-ray images of the left knee following repeat injury demonstrating a comminuted left distal femur fracture. (a) Anterior-posterior view. (b) Lateral view.
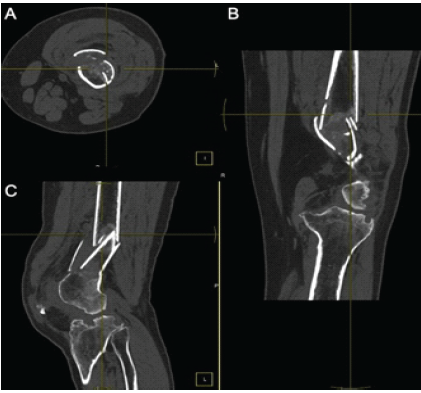
Figure 4: Computed tomography scan of the left knee following repeat injury. (a) Axial view. (b) Coronal view. (c) Lateral view.
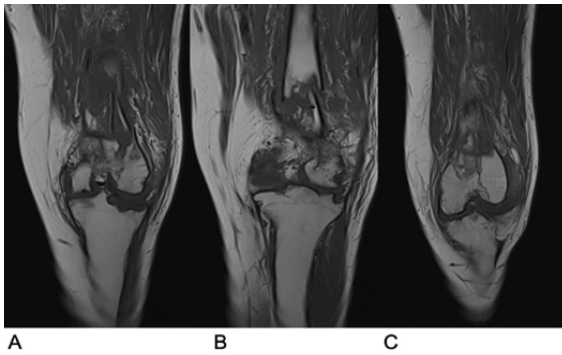
Figure 5: Magnetic resonance imaging scan of the left knee following repeat injury. (a) Coronal view of the anterior section of the joint. (b) Coronal view of the middle section of the joint. (c) Coronal view of the posterior section of the joint.
An MRI (Fig. 5) displayed normal marrow tissue and significant improvement in bony architecture compared to the initial MRI, with no suspicion of underlying lesions. A second open reduction and internal fixation was performed, with extensive samples taken for histological and microbiological analysis. Histological evaluations indicated acute inflammatory changes consistent with an acute fracture, and granulomas were absent. ZN staining and mycobacterial tissue culture were negative, confirming no recurrence of TB infection. The patient had a normal recovery following this surgical intervention, with tissue samples confirming successful treatment of TB. X-rays showed satisfactory alignment and implant placement (Fig. 6). The patient was pain-free while weight-bearing with one crutch at 12 weeks after the final surgery.
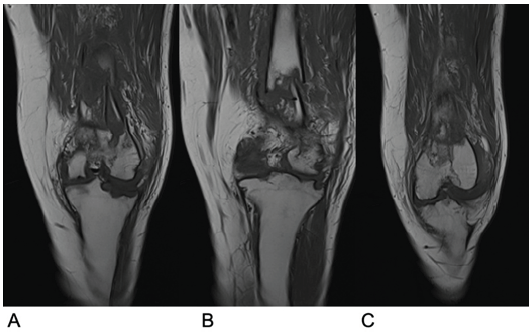
Figure 6: X-ray of the left knee at 12 weeks post-repeat surgery (a) Anterior-posterior view. (b) Lateral view.
This case underscores the diagnostic challenges associated with TB arthritis, particularly in European contexts where such cases are rare. In the absence of a high index of suspicion, non-specific symptoms can lead to treatment delays and significant joint destruction. Just under half of TB cases are extrapulmonary, and recent UK data found osteoarticular disease accounted for 6% of annual TB caseload (4.4% spinal, 1.8% non-spinal) [8]. Extrapolating from this, and from an American study on MSK TB and knee joint TB arthritis [6], there is roughly one TB arthritis case of the knee in Ireland annually. Utilizing search terms (“Tuberculosis” OR “TB”) AND (“Arthritis” OR “Arthritis, Tuberculous”) AND (“Knee” OR “Knee Joint”) on PubMed, we identified 19 reported cases of TB arthritis in native joints among immunocompetent adults over the past 25 years, of which 17 cases were available for review. To our knowledge, this case represents the first documented instance of knee TB arthritis in Ireland. Most cases over the past quarter-century were reported in low- and middle-income countries (LMIC), including five from India [9,10,11,12,13], two from Morocco [14,15], and one each from Turkey [16], the UK [17], South Korea [18], Italy [19], Iran [20], Vietnam [21], the Philippines [22], the US [23], Hong Kong [24], and Portugal [25]. Notably, all cases reported from high-income countries occurred in migrants from high-incidence LMICs. Most reported cases emphasize significant diagnostic delays in identifying TB arthritis of the knee, with a median time from symptom onset to definitive diagnosis across the 17 cases noted at around 12 months. Most of these delays resulted from failure to promptly obtain tissue for histological and appropriate mycobacterial investigation. One particular case involved a patient with symptoms spanning 7 years; her diagnosis was confirmed following total knee arthroplasty (TKA), during which biopsies were obtained. Histopathology revealed necrotizing granulomas, and cultures confirmed MTB. The initiation of ATT led to favorable outcomes 12 months after surgical intervention [25]. Misdiagnosis was prevalent among the reviewed cases. One notable instance involved a 27-year-old male who underwent radiation synovectomy for knee pain identified as non-specific synovitis; this intervention failed to relieve his symptoms. Following surgical synovectomy and biopsy, histological examination revealed epithelioid granulomas, and tissue polymerase chain reaction for TB was positive. The commencement of ATT led to symptom resolution [11]. If left untreated, TB arthritis of the knee can result in significant joint degradation. In our review, nine individuals underwent arthroscopic or open synovectomy for symptomatic treatment [9,10,11,12,18,19,20,21,22], with a case involving a 22-year-old Turkish male requiring knee arthrodesis due to extensive destruction [16]. Three patients underwent TKA of the affected joint, either before or following the initiation of ATT due to substantial joint damage [17,23,24]. Three patients only received medical treatment with ATT [13,14,15]. All 17 cases included in our review commenced some form of ATT as soon as TB was diagnosed. Favorable outcomes were recorded in 12 of these cases, with timelines indicating a median pain-free follow-up duration of 12 months after starting ATT. This case is of particular value for countries with low TB incidence, such as Ireland. Multidisciplinary review and diagnostic sampling should be encouraged.
This case and the accompanying literature review underscore the clinical significance of diagnosing TB large joint appendicular arthritis, particularly in patients migrating from high-incidence countries. It showcases the importance of multidisciplinary care and emphasizes the critical role of tissue for histological and mycobacterial evaluations of joint specimens when confronted with diagnostic uncertainty.
In young and healthy patients not recovering from knee injuries as expected, further diagnostic testing is warranted to exclude rare forms of arthritis, such as TB, despite low incidence rates in developed countries. Early diagnosis and treatment of TB in the knee joint are linked to favorable outcomes, whereas delays can incur significant and irreversible joint damage.
References
- 1. Hershkovitz I, Donoghue HD, Minnikin DE, May H, Lee OY, Feldman M, et al. Tuberculosis origin: The neolithic scenario. Tuberculosis (Edinb) 2015;95 Suppl 1:S122-6. [Google Scholar] [PubMed]
- 2. Barberis I, Bragazzi NL, Galluzzo L, Martini M. The history of tuberculosis: From the first historical records to the isolation of Koch’s bacillus. J Prev Med Hyg 2017;58:E9-12. [Google Scholar] [PubMed]
- 3. World Health Organisation. Global Tuberculosis Report. Geneva: World Health Organisation; 2024. [Google Scholar] [PubMed]
- 4. Health Protection Surveillance Centre. Tuberculosis in Ireland: Trends in Surveillance Data 2025. Ireland: Health Protection Surveillance Centre; 2025. [Google Scholar] [PubMed]
- 5. Central Statistics Office. Census of Population 2022 Profile 5 – Diversity, Migration, Ethnicity, Irish Travellers and Religion; 2022. Available from: https://www.cso.ie/en/releasesandpublications/ep/pcpp5/censusofpopulation2022profile5-diversitymigrationethnicityirishtravellersreligion/keyfindings. Accessed 18 Jan 2026 [Google Scholar] [PubMed]
- 6. Leonard MK, Blumberg HM. Musculoskeletal tuberculosis. Microbiol Spectr 2017;5(2)in Print. [Google Scholar] [PubMed]
- 7. Abid W, Ladeb MF, Chidambaranathan N, Peh WC, Vanhoenacker FM. Imaging of musculoskeletal tuberculosis. Skeletal Radiol 2024;53:2081-97. [Google Scholar] [PubMed]
- 8. UK Health Security Agency. Tuberculosis Incidence and Epidemiology, England, 2023. London: UK Health Security Agency; 2025. [Google Scholar] [PubMed]
- 9. Agarwal S, Akhtar N. Tri-compartmental tubercular arthritis of knee masquerading as popliteal fossa tumor: A case report. Orthop Surg 2010;2:313-5. [Google Scholar] [PubMed]
- 10. Meena S, Gangary SK. Knee tuberculosis masquerading as pigmented villonodular synovitis. J Res Med Sci 2014;19:1193-5. [Google Scholar] [PubMed]
- 11. Sood A, Sharma A, Chouhan D, Gupta K, Parghane R, Shukla J, et al. Failed radiation synovectomy in diseased knee joint with missed tuberculous synovitis. World J Nucl Med 2016;15:206-8. [Google Scholar] [PubMed]
- 12. Shakya A, Patil N, Kakadiya G, Soni Y. The great imitator – disseminated tuberculosis presenting as baker’s cyst: A case report. Malays Orthop J 2022;16:126-9. [Google Scholar] [PubMed]
- 13. Sureshkumar M, Rajamani S, Ravindran V, ArvindhKrishnan E. A rare case of smear positive tuberculous arthritis. Indian J Pathol Microbiol 2023;66:350-1. [Google Scholar] [PubMed]
- 14. Benchanna R, Benjelloune A, Abdelafatah Z, Arsalane A, Janah H, Oujaber J, et al. Report of a case of isolated tuberculous arthritis of the knee: A difficult diagnosis in adolescents. Pan Afr Med J 2020;37:225. [Google Scholar] [PubMed]
- 15. Miry A, Tbouda M, Bouhajeb YY, Abbaoui S. Tuberculosis of the tibial plateau mimicking a giant cell tumor: A case report. Cureus 2023;15:e43785. [Google Scholar] [PubMed]
- 16. Akgün U, Erol B, Cimşit C, Karahan M. Tuberculosis of the knee joint: A case report. Acta Orthop Traumatol Turc 2008;42:214-8. [Google Scholar] [PubMed]
- 17. Lidder S, Lang K, Haroon M, Shahidi M, El-Guindi M. Tuberculosis of the knee. Orthop Rev (Pavia) 2009;1:e24. [Google Scholar] [PubMed]
- 18. Lee DH, Lee DK, Lee SH, Park JH, Kim CH, Han SB. Tuberculous arthritis of the knee joint mimicking pigmented villonodular synovitis. Knee Surg Sports Traumatol Arthrosc 2012;20:937-40. [Google Scholar] [PubMed]
- 19. Uboldi FM, Limonta S, Ferrua P, Manunta A, Pellegrini A. Tuberculosis of the knee: A case report and literature review. Joints 2017;5:180-3. [Google Scholar] [PubMed]
- 20. Zamani B, Shayestehpour M. A case of knee monoarthritis caused by mycobacterium tuberculosis. Am J Case Rep 2019;20:522-4. [Google Scholar] [PubMed]
- 21. Hung TN, Duong TB, Binh TP, Tu DT, Hau HP, Tin TT, et al. Tuberculous arthritis of the knee with rice body formation: A report of a rare case. Case Rep Orthop 2020;2020:6369781. [Google Scholar] [PubMed]
- 22. Remalante-Rayco PP, Dumlao PI, Santiago AT. Great imitator: An unusual presentation of osteoarticular tuberculosis of the knee with gram-negative bacterial arthritis. BMJ Case Rep 2021;14:e245583. [Google Scholar] [PubMed]
- 23. Samade R, Voskuil RT, Scharschmidt TJ. Two-stage TKA for tuberculosis septic arthritis of the knee masquerading as pigmented villonodular synovitis: A case report. Knee 2022;38:30-5. [Google Scholar] [PubMed]
- 24. Chan HM, Fu H, Chiu KY. Tuberculosis of the knee as a great mimicker of inflammatory arthritis: A case report. Hong Kong Med J 2023;29:548-50. [Google Scholar] [PubMed]
- 25. Pinto I, Marques V, Dias L. Tuberculosis presenting as chronic monoarthritis: A case study. Cureus 2023;15:e39430. [Google Scholar] [PubMed]