Intratendinous ganglion cysts of the patellar tendon should be recognized as a potential cause of anterior knee pain.
Dr. Ezequiel Ortiz, Galvan 4102 CABA, Buenos Aires Argentina, E-mail: eortiz@cemic.edu.ar
Introduction: Ganglion cysts are benign soft-tissue lesions most commonly encountered around the wrist and hand, while their occurrence in the knee joint is relatively uncommon. An intratendinous location within the patellar tendon is exceptionally rare. This report describes a unique case of an intratendinous ganglion cyst of the patellar tendon, outlining its clinical presentation, imaging characteristics, surgical management, and histopathological confirmation.
Case Report: A 39-year-old male with a history of Osgood–Schlatter disease presented with progressive anterior knee pain. Magnetic resonance imaging (MRI) demonstrated a well-circumscribed, multilobulated cystic lesion within the patellar tendon, consistent with a ganglion cyst. The patient underwent complete surgical excision of the lesion, and histopathological examination confirmed the diagnosis. At follow-up, the patient exhibited full clinical recovery, return to sporting activities, and no evidence of recurrence on control MRI.
Conclusion: Intratendinous ganglion cysts of the patellar tendon are extremely rare and can mimic other etiologies of anterior knee pain. MRI remains the gold standard for diagnosis, whereas surgical excision provides definitive management. Recognition of this entity is essential for accurate differential diagnosis and appropriate treatment planning.
Keywords: Patellar tendon ganglion cyst, Intratendinous ganglion cyst, Anterior knee pain patellar tendon, Knee ganglion cyst.
Ganglion cysts are benign, mucin-filled cystic lesions most commonly observed in the wrist and hand, accounting for approximately 50–70% of all ganglion cysts [1]. Their occurrence around the knee joint is relatively uncommon, with most arising from the cruciate ligaments, joint capsule, or adjacent soft tissues [2,3,4]. Intra-articular ganglion cysts of the cruciate ligaments – particularly those involving the anterior cruciate ligament – have been increasingly reported in recent years [5,6]. In contrast, ganglion cysts originating within the patellar tendon are exceedingly rare, with only a few cases documented in the literature [7,8,9,10,11]. Their etiology remains uncertain; proposed mechanisms include mucoid degeneration, repetitive microtrauma, synovial herniation, or embryologic remnants [3,9]. Because of their rarity, these lesions are often overlooked in the differential diagnosis of anterior knee pain, which is more frequently attributed to conditions, such as patellar tendinopathy, Osgood–Schlatter disease, or infrapatellar bursitis. Magnetic resonance imaging (MRI) plays a pivotal role in the accurate characterization of these lesions and in guiding appropriate management [8,11]. We report a rare case of an intratendinous ganglion cyst of the patellar tendon in an adult patient with a prior history of Osgood–Schlatter disease, along with a review of the relevant literature.
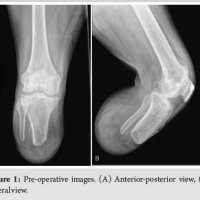
A 39-year-old male presented with a 6-month history of progressive anterior knee pain, aggravated by physical activity and kneeling. He denied any recent trauma but reported a history of Osgood–Schlatter disease during adolescence. Physical examination revealed tenderness over the anterior aspect of the knee and a palpable fusiform swelling along the course of the patellar tendon. Range of motion was preserved, and ligamentous stability tests were negative. No signs of meniscal pathology were detected. Plain radiographs demonstrated residual ossicles at the tibial tuberosity, consistent with sequelae of Osgood–Schlatter disease (Fig. 1).
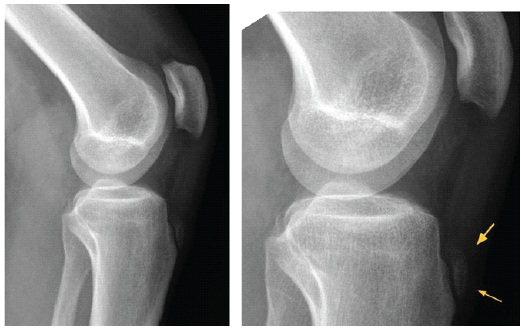
Figure 1: Lateral knee radiographs demonstrate residual ossicles at the tibial tuberosity, consistent with sequelae of Osgood–Schlatter disease.
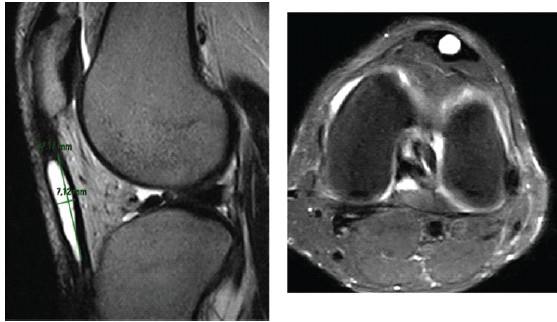
MRI revealed a well-circumscribed, multilobulated cystic lesion – hypointense on T1-weighted and hyperintense on T2-weighted sequences – located within the substance of the patellar tendon, measuring 2.5 × 1.5 × 1.2 cm. The lesion showed no communication with the knee joint cavity. Surrounding tendon fibers appeared intact, with no evidence of rupture or inflammatory changes (Fig. 2).
 Given the symptomatic nature of the lesion, surgical excision was indicated. Across an anterior longitudinal approach, the patellar tendon was exposed, and the cystic lesion was identified within its substance. Careful dissection enabled en bloc removal of the cyst while preserving the surrounding tendon fibers. The resulting defect was repaired using side-to-side sutures. Histopathological examination revealed a cystic cavity lined by dense fibrous connective tissue without a synovial lining, consistent with a ganglion cyst (Fig. 3).
Given the symptomatic nature of the lesion, surgical excision was indicated. Across an anterior longitudinal approach, the patellar tendon was exposed, and the cystic lesion was identified within its substance. Careful dissection enabled en bloc removal of the cyst while preserving the surrounding tendon fibers. The resulting defect was repaired using side-to-side sutures. Histopathological examination revealed a cystic cavity lined by dense fibrous connective tissue without a synovial lining, consistent with a ganglion cyst (Fig. 3).
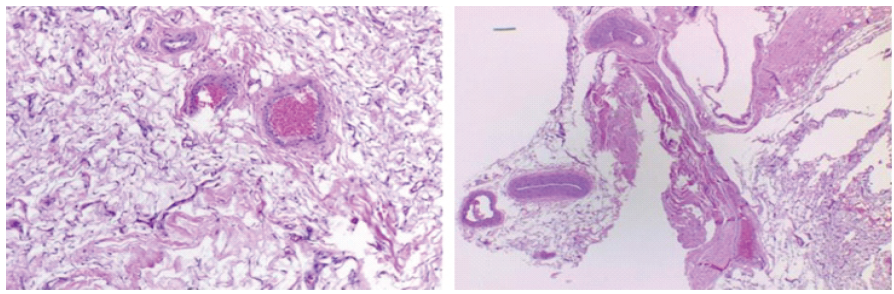
Figure 3: Hematoxylin–eosin–stained histological sections reveal a cystic cavity bordered by dense fibrous connective tissue and lacking a synovial lining, consistent with a ganglion cyst.
Rehabilitation protocol
Post-operatively, the patient was allowed full weight-bearing as tolerated with the assistance of crutches and a knee brace for the first 48 hours. Analgesics, including non-steroidal anti-inflammatory drugs, were prescribed on an as-needed basis for pain control. During the initial 2-week period, knee flexion was restricted to 0–30°, and only passive range-of-motion exercises were permitted to minimize mechanical stress on the patellar tendon. The sutures were removed at 14 days. From weeks 2 to 4, knee flexion was gradually increased to 30–60°, with continued use of crutches and the knee brace during ambulation. Between weeks 4 and 6, controlled progression of knee motion was allowed, aiming to achieve a full range of motion by the 6th post-operative week. Quadriceps strengthening – focused on closed-chain, low-load exercises – was initiated once full motion had been restored and tendon healing appeared clinically stable. After 6 weeks, the patient progressed to advanced strengthening and functional rehabilitation, including proprioceptive training and a gradual return to daily activities. Return to unrestricted physical activity and sports participation was recommended at approximately 6 months, based on symptom resolution, functional performance, and tendon integrity. MR confirmed satisfactory tendon healing with no evidence of ganglion cyst recurrence at 12-month follow-up (Fig. 4).
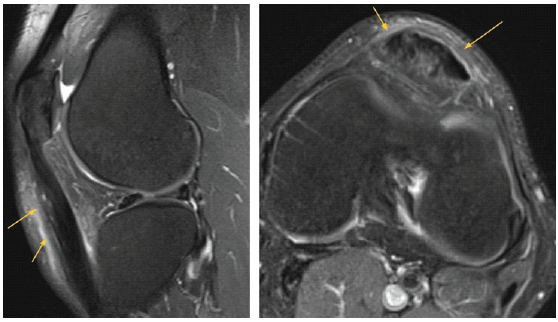
Figure 4: Post-operative knee magnetic resonance imaging reveals complete excision of the ganglion cyst and reparative tendinous scar tissue.
Ganglion cysts of the knee are uncommon lesions, most of which are located intra-articularly, typically arising in association with the cruciate ligaments [1,2,3,4,5,6]. Intratendinous ganglion cysts of the patellar tendon are exceedingly rare, with only sporadic cases reported in the literature [7,8,9,10,11] (Table 1).
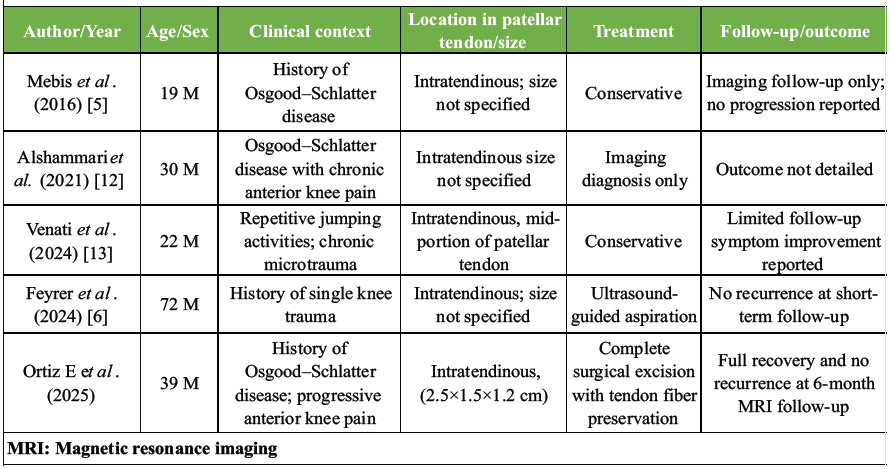
Table 1: Case report of Intratendinous ganglion cysts of the patellar tendon.
The pathogenesis of these cysts remains controversial. Several mechanisms have been proposed, including mucoid degeneration of connective tissue, synovial herniation, embryonic remnants, and repetitive microtrauma [3,9]. In the present case, a prior history of Osgood–Schlatter disease may have predisposed the patient to chronic microtrauma and subsequent cyst formation. Clinically, these cysts may manifest as anterior knee pain, swelling, or a palpable mass, often mimicking more common conditions, such as patellar tendinopathy or infrapatellar bursitis. Therefore, they should be considered in the differential diagnosis of anterior knee pain, particularly in young and physically active individuals. MRI is the diagnostic modality of choice, as it provides superior soft-tissue contrast and enables accurate delineation of the lesion, its extent, and its relationship with surrounding structures [8,11]. In our case, MRI allowed precise localization of the cyst within the patellar tendon and confirmed the absence of communication with the joint cavity. Surgical excision remains the most widely reported and reliable treatment, offering both definitive diagnosis and durable symptom resolution [7,8,9,10,11]. Although excision remains the standard approach, less invasive alternatives have been described. Ultrasound-guided aspiration may be considered in selected cases – particularly for superficial or extra-articular cysts – as it offers both diagnostic confirmation and temporary symptom relief [3]. However, recurrence rates following aspiration are considerably higher compared with open excision, and its applicability to intratendinous lesions is limited. Histopathological examination is essential to differentiate ganglion cysts from other cystic lesions, such as synovial cysts or degenerative myxoid changes. In our case, the absence of a synovial lining confirmed the diagnosis of a ganglion cyst. The post-operative prognosis following surgical excision is generally excellent, with low recurrence rates reported in the literature [7,8,9,10,11]. Our patient remained asymptomatic and recurrence-free at 6-month follow-up.
Intratendinous ganglion cysts of the patellar tendon are exceedingly rare entities that should be included in the differential diagnosis of anterior knee pain. MRI is indispensable for accurate diagnosis, while surgical excision remains the gold standard treatment, ensuring symptom resolution and a low likelihood of recurrence.
Even though exceedingly rare, intratendinous ganglion cysts of the patellar tendon should be recognized as a potential cause of anterior knee pain. MRI is essential for diagnosis, and surgical excision offers curative treatment with a low risk of recurrence.
References
- 1. Mao Y, Dong Q, Wang Y. Ganglion cysts of the cruciate ligaments: A series of 31 cases and review of the literature. BMC Musculoskelet Disord 2012;13:137. [Google Scholar] [PubMed]
- 2. Kim MG, Kim BH, Choi JA, Lee NJ, Chung KB, Choi YS, et al. Intra-articular ganglion cysts of the knee: Clinical and MR imaging features. Eur Radiol 2001;11:834-40. [Google Scholar] [PubMed]
- 3. Krudwig WK, Schulte KK, Heinemann C. Intra-articular ganglion cysts of the knee joint: A report of 85 cases and review of the literature. Knee Surg Sports Traumatol Arthrosc 2004;12:123-9. [Google Scholar] [PubMed]
- 4. Jose J, O’Donnell K, Lesniak BP. Symptomatic intratendinous ganglion cyst of the patellar tendon. Orthopedics 2011;34:135. [Google Scholar] [PubMed]
- 5. Mebis W, Jager T, Van Hedent E. Intratendinous patellar ganglion cyst with coexistant osgood schlatter disease. J Belg Soc Radiol 2016;100:86. [Google Scholar] [PubMed]
- 6. Feyrer M, Sesselmann S, Koehl P, Schuh A. An intratendinous ganglion cyst of the patellar tendon: A rare cause of anterior knee pain. Georgian Med News 2023;343:204-5. [Google Scholar] [PubMed]
- 7. Deutsch A, Veltri DM, Altchek DW, Potter HG, Warren RF, Wickiewicz TL. Symptomatic intraarticular ganglia of the cruciate ligaments of the knee. Arthroscopy 1994;10:219-23. [Google Scholar] [PubMed]
- 8. Bui-Mansfield LT, Youngberg RA. Intraarticular ganglia of the knee: Prevalence, presentation, etiology, and management. AJR Am J Roentgenol 1997;168:123-7. [Google Scholar] [PubMed]
- 9. Tachibana Y, Sugimoto K, Moriya H. Intra-articular ganglia arising from the posterior joint capsule of the knee. Arthroscopy 2004;20:54-9. [Google Scholar] [PubMed]
- 10. Touraine S, Lagadec M, Petrover D, Genah I, Parlier-Cuau C, Bousson V, et al. A ganglion of the patellar tendon in patellar tendon-lateral femoral condyle friction syndrome. Skeletal Radiol 2013;42:1323-7. [Google Scholar] [PubMed]
- 11. Jain M, Sahu NK, Behera S, Rana R, Patra SK. Intra-tendinous patellar ganglion cyst maybe the unusual cause of knee pain: A case report. Cureus 2019;11:e5467. [Google Scholar] [PubMed]
- 12. Alshammari A, Alajmi S, AlHajri A. Intratendinous ganglion cyst of the patellar tendon associated with Osgood-Schlatter disease: A case report. Kuwait Med J 2021;53:252-5. [Google Scholar] [PubMed]
- 13. Venati U, Rahul BN, Damayanthi Y, Botchu R. Unusual etiology of anterior knee pain in a young athlete engaged in chronic jumping exercises: The intratendinous ganglionic cyst of the patellar tendon. Indian J Musculoskelet Radiol. 2024;6:65-9. doi: 10.25259/IJMSR_53_2023. [Google Scholar] [PubMed] [CrossRef]