The present case report highlights the importance of meticulous planning and modified tunnel techniques for safe and effective ACL reconstruction in patients with Hereditary multiple exostoses.
Dr. Harshita Udiwal, Department of Orthopaedics, Bhagyoday medical college and Hospital, Kadi, India. E-mail: udiwalharshita@gmail.com
Introduction Hereditary multiple exostoses, also known as multiple osteochondromas, is a rare genetic disorder marked by the formation of osteocartilaginous outgrowths predominantly near the metaphysis of long bones. The knee is a commonly affected joint. Surgical reconstruction of the anterior cruciate ligament in patients with Hereditary multiple exostoses presents unique challenges due to distorted bony anatomy, posing risks to graft harvesting, tunnel positioning, and fixation.
Case report We present the case of a 17-year-old female football athlete with symptomatic Anterior cruciate ligament deficiency on a background of Hereditary multiple exostoses. Following persistent instability despite conservative management, she underwent arthroscopic Anterior cruciate ligament reconstruction using a tripled peroneus longus tendon autograft. Special precautions were taken intraoperatively to navigate anatomical distortions and ensure precise tunnel placement while avoiding conflict with osteochondromas. Fixation was achieved using a femoral Endobutton and tibial ‘T’ button.
Conclusion Anterior cruciate ligament reconstruction in patients with Hereditary multiple exostoses is feasible and can yield excellent functional outcomes when anatomical variations are meticulously accounted for in surgical planning. Peroneus longus graft is a viable option when conventional grafts are compromised or inaccessible due to exostoses.
Keywords: Anterior cruciate ligament reconstruction, Hereditary multiple exostoses, Osteochondromas, Peroneus longus graft, Tunnel placement, Knee instability, Adolescent athlete
Hereditary multiple exostoses (HME) is an autosomal dominant skeletal dysplasia with an estimated incidence of 1 in 50,000 individuals [1]. It is characterized by multiple osteocartilaginous exostoses, primarily in the metaphyseal regions of long bones, with the knee affected in up to 98% of cases [1]. Although many patients remain asymptomatic, complications such as deformity, neurovascular compression, and malignant transformation have been documented [1]. ACL injuries are common among athletes and typically managed with arthroscopic reconstruction but in a patient with MHE, ACL reconstruction is a challenge because of the presence of exostoses around the knee and the poor bone quality; such an anatomical anomaly can interfere with tendon harvesting, tunnel placement and implant fixation, and it can compromise the success of reconstruction. [2,3]. ACL reconstruction in adolescents presents additional considerations related to graft choice, fixation strength, and preservation of surrounding anatomy. Adolescent athletes have a higher risk of reinjury and graft failure, particularly in anatomically complex knees, necessitating individualized surgical strategies [4-9]. Furthermore, cortical suspensory fixation has gained popularity in such scenarios due to its reliable biomechanical strength and reduced dependence on metaphyseal bone quality [10]. We report a case of successful ACL reconstruction using peroneus longus tendon autograft in a female adolescent athlete with HME and discuss unique technical considerations.
A 17-year-old female national-level football athlete presented with right knee pain, instability, and giving-way episodes following a twisting injury four months prior. She had a known history of HME with multiple bony swellings around her knees since childhood. Clinical examination revealed swelling, tenderness, and multiple palpable exostoses. Lachman, anterior drawer, and pivot shift tests were positive. Conservative management with bracing and physiotherapy failed. Radiographs showed multiple osteochondromas around the distal femur and proximal tibia (Fig. 1), and MRI confirmed a complete ACL tear without meniscal injury (Fig. 2).
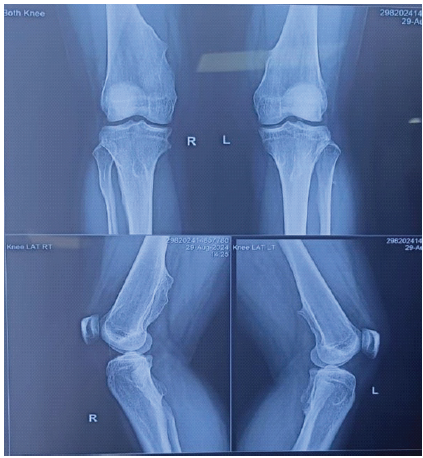
Figure 1. Preoperative radiographs showing multiple exostoses around distal femur and proximal tibia.
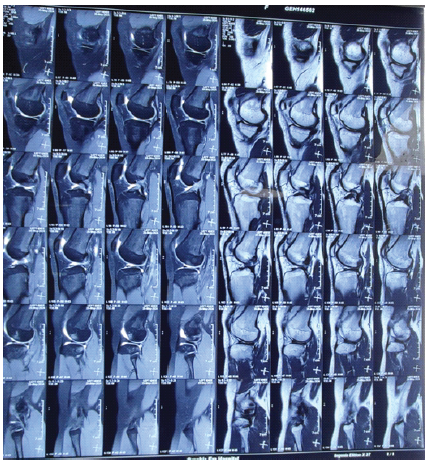
Figure 2. MRI of the knee demonstrating a complete ACL tear and multiple exostoses.
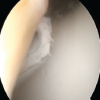
She underwent arthroscopic ACL reconstruction under spinal anesthesia. A 2-mm notchplasty improved visualization. Due to exostoses compromising hamstring tendons, peroneus longus autograft was harvested, tripled (7.5 mm diameter), and prepared (Fig. 3).
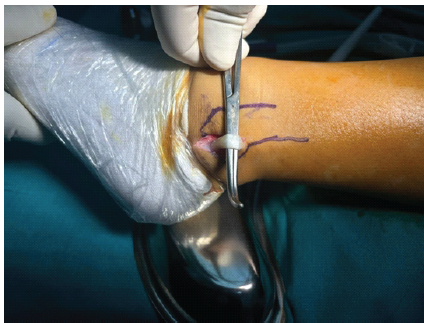
Figure 3. Intraoperative image showing peroneus longus tendon graft harvesting.
Tibial tunnel was created avoiding medial exostosis, and femoral tunnel was drilled via anteromedial portal to bypass femoral exostoses. Fixation was achieved using femoral Endobutton and tibial ‘T’ button. No intraoperative complications occurred, and arthroscopy confirmed good graft position (Fig. 4). Postoperative rehabilitation commenced on day one, and the patient progressed uneventfully (Fig. 5).
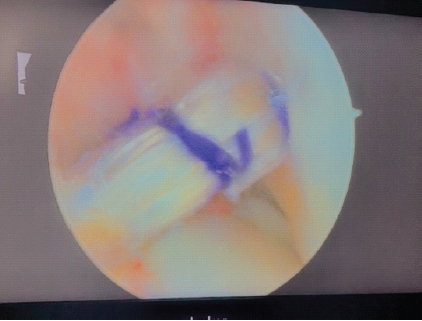
Figure 4. Arthroscopic image showing peroneus longus graft in situ after fixation.
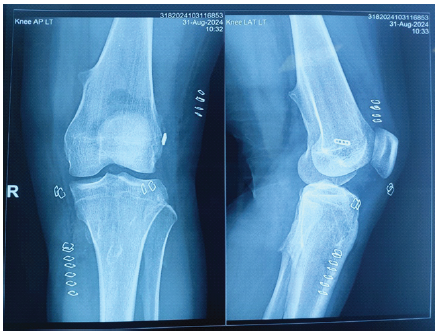
Figure 5. Postoperative radiographs showing graft fixation with femoral Endobutton and tibial ‘T’ button.
ACL reconstruction in the setting of Hereditary Multiple Exostoses is rare, with only a limited number of cases reported in the literature. The presence of multiple osteochondromas around the knee leads to altered bony morphology, making identification of conventional arthroscopic landmarks challenging. This increases the risk of non-anatomical tunnel placement and fixation failure if standard techniques are employed. Thorough preoperative evaluation using radiographs and magnetic resonance imaging is therefore critical to delineate exostosis location and to facilitate safe surgical planning [1,2].
Distorted proximal tibial and distal femoral anatomy in HME necessitates modification of standard tunnel drilling techniques. Preoperative imaging assists in determining alternative tunnel trajectories that avoid cortical breach or exostotic interference. Femoral tunnel drilling via the anteromedial portal allows improved control of tunnel orientation and facilitates anatomical graft placement in knees with atypical geometry. Such modified approaches have been recommended to minimize technical complications and optimize graft biomechanics [5,7].
Selection of an appropriate graft is a crucial determinant of success in ACL reconstruction, particularly in adolescent athletes with complex knee anatomy. Although hamstring tendon autografts are widely used, their harvest may be compromised in HME due to altered pes anserinus anatomy or adjacent exostoses. Literature supports the use of alternative autografts in such situations to avoid intraoperative difficulties and compromised graft quality [2,3,8]. The peroneus longus tendon has emerged as a reliable alternative, demonstrating biomechanical strength comparable to conventional grafts with minimal donor-site morbidity and no significant impact on ankle stability [6,8]. In the present case, its use allowed adequate graft diameter and length while circumventing the challenges posed by distorted medial knee anatomy.
Fixation technique is another critical consideration in knees affected by HME. Irregular metaphyseal bone and altered cortical integrity may limit the reliability of interference screw fixation. Suspensory cortical fixation devices provide consistent biomechanical stability while minimizing dependence on local bone quality. Biomechanical and clinical studies have demonstrated comparable or superior load-to-failure characteristics of cortical button fixation when compared with interference screws, particularly in anatomically abnormal knees [5,10]. In our patient, the use of femoral and tibial cortical buttons provided secure fixation while avoiding compromised bone regions.
Adolescent athletes represent a high-risk group for graft failure and reinjury following ACL reconstruction. Autografts remain the preferred option in this population due to superior incorporation and lower failure rates compared to allografts [8,9]. When anatomical abnormalities coexist, as in HME, careful customization of graft choice, tunnel placement, and fixation becomes even more essential to ensure durable outcomes.
Previous case reports have described successful ACL reconstruction in patients with HME using hamstring and quadriceps tendon grafts, while emphasizing the technical difficulty associated with tunnel placement and graft harvest [2,3]. Our case expands the existing literature by demonstrating that a peroneus longus autograft, combined with modified tunnel orientation and suspensory fixation, is a safe and effective alternative in this rare clinical scenario.
Postoperative rehabilitation in HME does not differ significantly from standard ACL protocols, although careful monitoring is warranted due to potential limb deformity or altered mechanics. Our patient progressed uneventfully and resumed sports-specific training, suggesting that once anatomical challenges are successfully addressed intraoperatively, functional recovery parallels that of routine ACL reconstruction.
Only a limited number of cases describing ACL reconstruction in HME exist in the literature. Zmerly et al. reported successful ACL reconstruction using hamstring grafts but highlighted the difficulty of tunnel placement in the presence of exostoses [2]. Mulford et al. described quadriceps tendon graft use due to hamstring involvement, reinforcing the importance of alternative graft options [3]. Our case further supports these findings and is unique in demonstrating the effective use of a peroneus longus autograft combined with customized tunnel placement and suspensory fixation.
Overall, this case emphasizes that ACL reconstruction in patients with HME is safe and effective when approached with meticulous preoperative planning, individualized graft selection, and modified surgical techniques. Understanding the unique anatomical challenges posed by HME is crucial to avoid complications and achieve optimal functional outcomes.
ACL reconstruction in patients with Hereditary Multiple Exostoses is technically demanding but feasible when meticulous preoperative planning and individualized surgical strategies are employed. Alternative graft options, modified tunnel placement, and suspensory cortical fixation can successfully overcome the anatomical challenges posed by exostoses. These considerations are particularly important in adolescent athletes, where long-term graft survival and functional recovery are paramount.
Individualized tunnel placement and suspensory cortical fixation can overcome distorted anatomy in HME and enable effective anatomical ACL reconstruction.
References
- 1. Schmale GA, Conrad EU, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am. 1994;76(7):986–92. [Google Scholar] [PubMed]
- 2. Zmerly H, Akkawi I, Libri R, Moscato M, Di Gregori V. Arthroscopic anterior cruciate ligament reconstruction in a patient with multiple hereditary exostoses. Acta Biomed. 2021 Jul 26;92(S3):e2021004. [Google Scholar] [PubMed]
- 3. Mulford JS, Hutchinson SE, Hang JR. Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013 Aug;21(8):1882-8 [Google Scholar] [PubMed]
- 4. Macaulay AA, Perfetti DC, Levine WN. Anterior cruciate ligament graft choices. Sports Health. 2012;4:63–8. [Google Scholar] [PubMed]
- 5. Kercher J, Xerogeanes J, Tannenbaum A, Al-Hakim R, Black JC, Zhao J. Anterior cruciate ligament reconstruction in the skeletally immature: an anatomical study utilizing 3-dimensional magnetic resonance imaging reconstructions. J Pediatr Orthop. 2009 Mar;29(2):124-9. [Google Scholar] [PubMed]
- 6. Shi FD, Hess DE, Zuo JZ, Liu SJ, Wang XC, Zhang Y, et al. Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg. 2019;32:804–11. [Google Scholar] [PubMed]
- 7. Rahnemai-Azar AA, Sabzevari S, Irarrázaval S, Chao T, Fu FH. Anatomical Individualized ACL Reconstruction. Arch Bone Jt Surg. 2016 Oct;4(4):291-297. [Google Scholar] [PubMed]
- 8. Paschos NK, Vasiliadis HS. Allograft versus autograft for reconstruction of anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2018 Sep 27;2018(9):CD010661. [Google Scholar] [PubMed]
- 9. Shea KG, Grimm NL, Ewing CK, Aoki SK. Youth sports anterior cruciate ligament and knee injury epidemiology: who is getting injured? In what sports? When? Clin Sports Med. 2011 Oct;30(4):691-706. [Google Scholar] [PubMed]
- 10. Mayr R, Smekal V, Koidl C, Coppola C, Eichinger M, Rudisch A, Kranewitter C, Attal R. ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc. 2020 Apr;28(4):1036-1044. [Google Scholar] [PubMed]