Retrograde elastic nail fixation of humeral shaft fractures in children with two nails through a central entry point is a reliable technique, with a low risk of complications.
Dr. Sudhir Shankar Mane, Department of Orthopaedics, First Floor, SVS Medical College and Hospital, Yenugonda, Mahabubnagar - 509002, Telangana, India. E-mail: sdhrmane@gmail.com
Introduction: Almost all pediatric humerus fractures can be managed conservatively with a high rate of union. Surgical intervention may be indicated in a few scenarios. Retrograde nailing with titanium elastic nails through a central entry point proximal to the olecranon fossa offers several advantages over conservative management.
Case Report: Three male patients in the age group of 5–14 years with diaphyseal left humerus fractures were treated with retrograde elastic nailing after failed conservative management. The mean age of the patients was 10 years. All the surgeries were performed under general anesthesia. The mean operative time was 100 min. The mean union time was 12 weeks. All cases had excellent outcomes. One patient developed a surgical site infection, and the nails had to be removed 6 weeks after the surgery.
Conclusion: When surgical stabilization of pediatric humeral shaft fractures is indicated, retrograde elastic nail fixation with two nails through a central entry point is a reliable technique, with a low risk of complications, offering stable fixation that eliminates the need for uncomfortable immobilization and enables early mobilization of the arm.
Keywords: Retrograde elastic nailing, pediatric humerus fractures, titanium elastic nails.
Humeral shaft fractures account for about 2.5% of all traumatic fractures in children and are the second most common birth-related fractures, following clavicle fractures [1]. Almost all pediatric humerus fractures can be managed conservatively with a high rate of union. Authors suggest that before opting for non-operative treatment, the deformity should be reduced to within 30° for fractures of the proximal third, 20° for those in the middle third, and 15° for fractures of the distal third of the shaft [2]. Surgical intervention may be required in cases of polytrauma to enable early mobilization, in compound fractures for wound management, in patients with head injuries to facilitate nursing care, and in certain instances with unacceptable angulation to preserve proper alignment [3]. Several techniques of retrograde nailing with titanium elastic nails for humerus fractures have been described. Antegrade nailing is not preferred due to violation of the rotator cuff, the possibility of injury to the growth plate, and impingement on the shoulder. Plate osteosynthesis is not recommended for humerus fractures in children. Retrograde Ender nails may be used [4]. Alternatively, titanium or stainless steel elastic nails may also be used. One technique involves making a small skin incision and entry over the medial and lateral epicondyles [3]. Another technique has been described where two elastic nails are inserted in a retrograde manner through a central entry point on the posterior aspect of the humerus, slightly proximal to the olecranon fossa [5]. The second technique was used to treat three children with humerus shaft fractures in whom conservative methods had failed. Very few studies in the literature have reported the long-term outcomes using this method. This case series includes three boys aged 7 years, 9 years, and 14 years with closed middle-third fractures of the left humerus who underwent retrograde titanium elastic nailing (Table 1). None of the patients had neurovascular injury or associated injuries. All the surgeries were done under general anesthesia by the same surgeon.
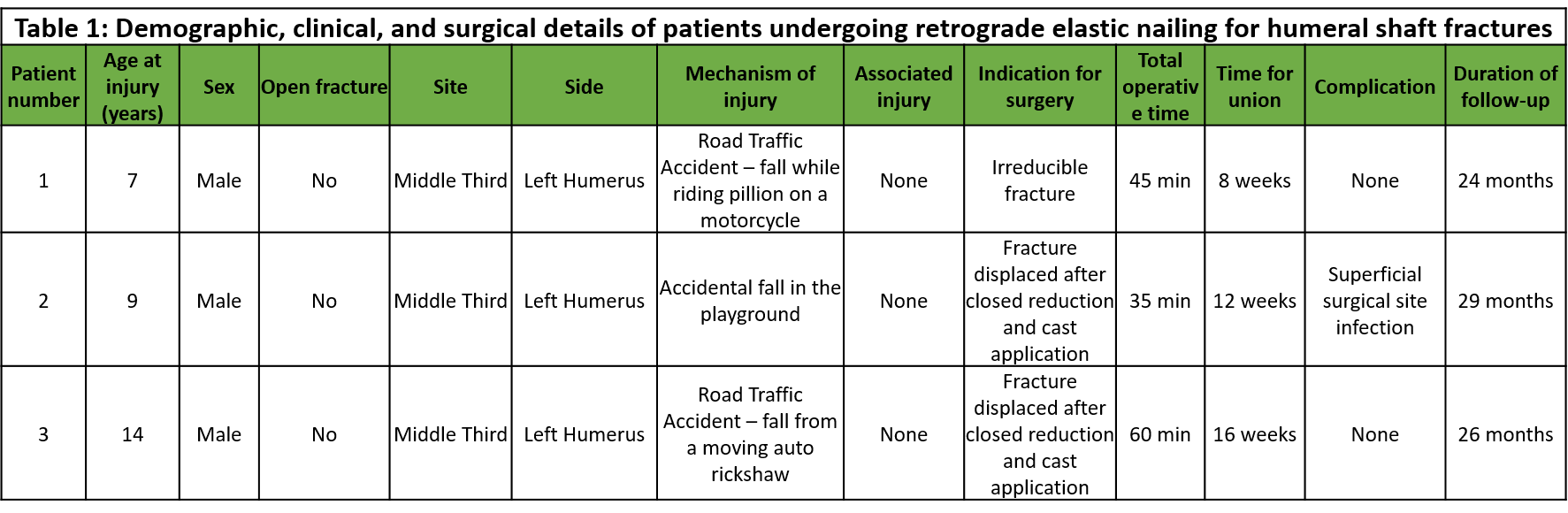
Table 1: Demographic, clinical, and surgical details of patients undergoing retrograde elastic nailing for humeral shaft fracture
Surgical Technique and Post-operative Protocol
This technique has been mentioned in detail in Lovell and Winter’s Pediatric Orthopaedics [5]. The patient was kept in a supine position with the arm on a radiolucent table. A posterior midline skin incision (Fig. 1b), 4–6 cm, was made proximal to the olecranon fossa. The incision extended through the triceps fascia, and the triceps muscle was split by blunt dissection to expose the posterior humerus. Care was taken to avoid the radial nerve, located closer to the lateral epicondyle in children compared to adults. An entry point (Fig. 1a) was made with a drill or a straight bone awl above the olecranon fossa to access the medullary canal, with the distance adjusted for the child’s size. Careful attention must be given when creating the entry point to minimize the risk of an iatrogenic fracture.
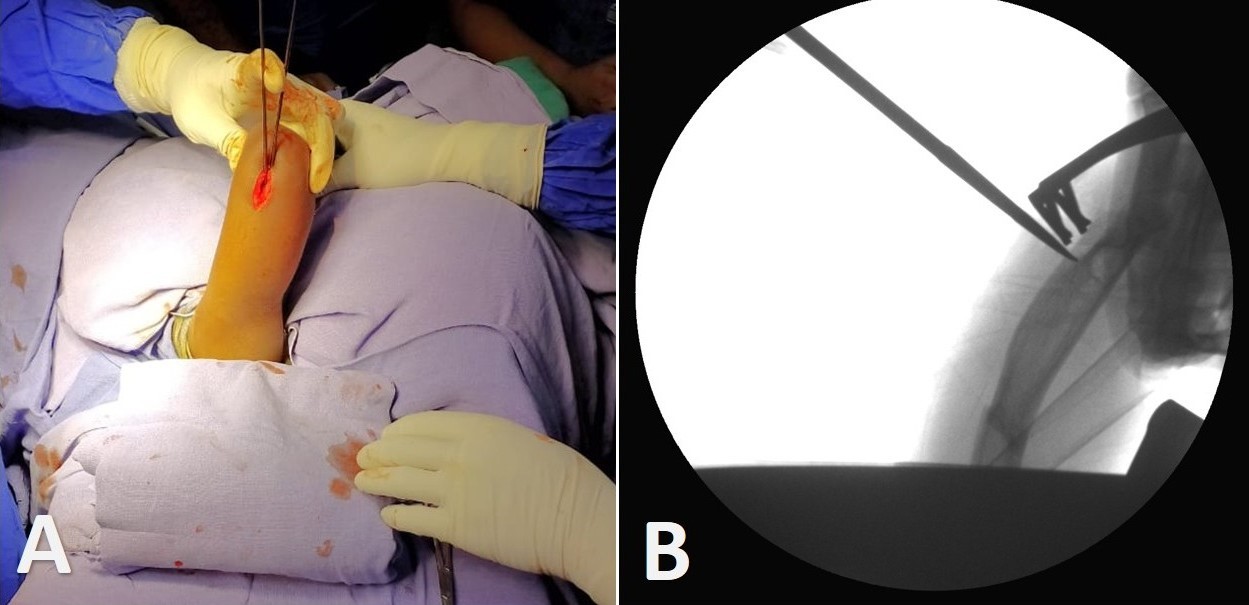
Figure 1: (a) Making an entry point using a bone awl proximal to the olecranon fossa, (b) Demonstration of the skin incision.
The elastic nails were selected based on the humerus size and bent slightly at the distal end. The nail was inserted, driven to the fracture site (Fig. 2a), and passed into the proximal fragment after reduction (Fig. 2b). A second rod was inserted for rotational stability, with one nail directed toward the greater tuberosity and the other toward the humeral head (Fig. 2c). Under fluoroscopic guidance, the rods are positioned correctly. The excess length is trimmed, leaving sufficient protrusion for removal (Fig. 2d). Fluoroscopy ensures proper positioning and fracture reduction.
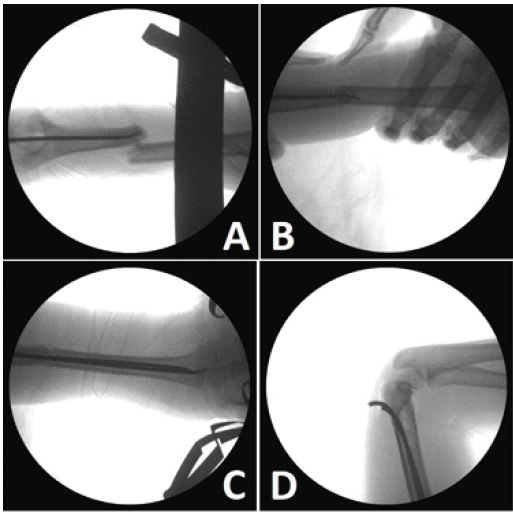
Figure 2: (a) First elastic nail brought to the fracture site, (b) nail passed into the proximal fragment after reducing the fracture, (c) orientation of the nails relative to the greater tuberosity and humeral head, (d) the elastic nails are cut and trimmed at the level of the entry point to avoid soft-tissue irritation and to facilitate their removal.
A sling or shoulder immobilizer is typically sufficient for stabilization. Range-of-motion exercises can usually begin within 3–4 weeks as healing progresses. Rods are removed electively after complete healing.
Patient 1
A 7-year-old boy presented with a closed fracture involving the middle third of the left humerus (Fig. 3a), sustained from a road traffic accident after falling while riding as a pillion on a motorcycle. The fracture was irreducible through conservative means, necessitating surgical intervention (Fig. 3b). The fracture united within 8 weeks (Fig. 3c), with no reported complications. Implant removal was done after 3 months. The patient was followed up for 24 months, demonstrating satisfactory recovery and healing with a full range of motion (ROM) at the shoulder and elbow (Fig. 3d and e).
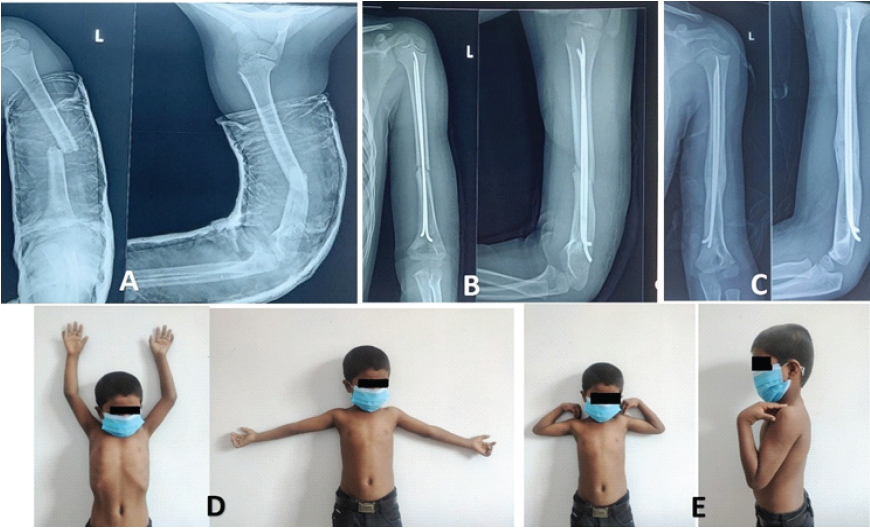
Figure 3: (a) Pre-operative X-ray of Patient 1, (b) Immediate post-operative X-ray of Patient 1, (c) Follow-up X-ray at 8 weeks, (d and e) Full range of motion at the shoulder and elbow after implant removal.
Patient 2
A 9-year-old boy sustained a closed fracture of the middle third of the left humerus due to an accidental fall in a playground. Initially managed with closed reduction and cast application, the fracture subsequently displaced (Fig. 4a), warranting surgical treatment (Fig. 4b). Callus formation was achieved at 6 weeks (Fig. 4c). However, the patient experienced a superficial surgical site infection necessitating implant removal. The fracture united in 12 weeks. The infection was controlled with IV antibiotics, and the patient had no further complications. Follow-up continued for 29 months, showing good long-term outcomes and full ROM of the elbow.
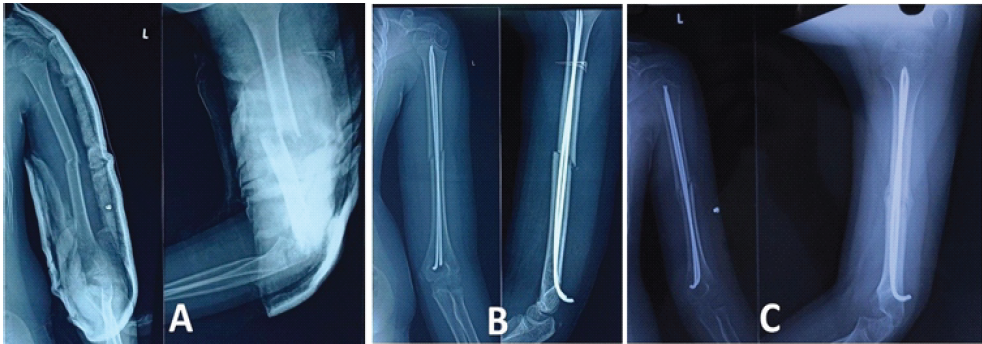
Figure 4: (a) Pre-operative X-ray of Patient 2, (b) Immediate post-operative X-ray of Patient 2, (c) Follow-up X-ray at 6 weeks when implant removal was planned.
Patient 3
A 14-year-old boy suffered a closed fracture of the middle third of the left humerus (Fig. 5a) following a road traffic accident, involving a fall from a moving auto rickshaw. Despite initial conservative management with cast application, the fracture was found to be displaced, necessitating surgical intervention (Fig. 5b). Fracture union occurred within 16 weeks, with no reported complications. Implant removal was done at 4 months. The patient was followed up for 60 months, indicating a favorable outcome with no residual issues and full ROM in the elbow.
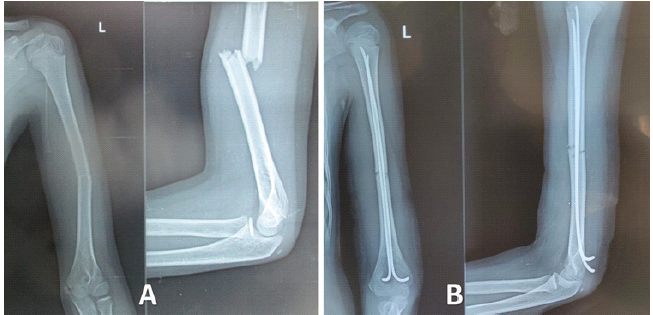
Figure 5: (a) Pre-operative X-ray of Patient 3, (b) Immediate post-operative X-ray of Patient 3.
We present a case series of three boys aged 7 years, 9 years, and 14 years with closed middle third fractures of the left humerus treated with retrograde titanium elastic nail fixation through a single entry point made proximal to the olecranon fossa. The outcomes in our case series were excellent. All the patients had a full range of motion in the elbow joint. Only one patient had to undergo implant removal earlier than indicated due to a surgical site infection. In this study, the average age of the patients was 10 years, with a fracture union time of 12 weeks and an average follow-up duration of 37.6 months. The QuickDASH score [6] for all patients at 3-month follow-up was 0. All fractures achieved healing in good alignment, with no intraoperative complications such as neurologic or vascular injuries. Closed reduction may fail due to the interposition of muscle or periosteum between the fracture ends. In patients where closed reduction fails, open reduction may be attempted by making a skin incision over the fracture site. A retrospective study of 13 patients (mean age 12.0 years) by Garg et al. from the USA reported that all fractures healed in good alignment with no intraoperative complications or infections [3]. The dual entry point technique with two nails was followed in 11 patients, whereas antegrade nailing was done for two patients. Two cases of nail migration occurred, including one with skin protrusion, and one patient required tendon transfer for pre-operative radial nerve injury. Notably, 12 of 13 patients returned to full activities without limitations, aligning with our study’s findings. Samara et al. reported a single nail technique of retrograde nailing for proximal humerus fractures in 19 children, where the entry point was made 10–20 mm proximal to the lateral epicondyle [7]. All fractures appeared united on the radiographs at a median of 6 weeks. A Nepali study that included 28 children reported excellent results in 85.71% of patients and good outcomes in 14.29% [8]. A single retrograde nail was used. The average patient age was 8.85 ± 1.84 years (range: 6–12), and the mean time to fracture union was 8.28 ± 2.43 weeks (range: 6–12). Complications included one case each of malunion (~10°), nail migration, superficial infection, transient radial nerve palsy, and nail protrusion. Wang et al. from China reported excellent outcomes in 37 children using the dual entry point technique for the proximal humerus [9]. They reported skin irritation due to protruding hardware at the distal humerus in two cases. This was resolved after implant removal. The mean union time was 8 weeks (range 7–10 weeks) after surgery. A Korean study evaluated the antegrade and retrograde two-nail technique in 12 patients [10]. No neurovascular injuries or infections occurred during surgery. However, four patients experienced nail site irritation, with two requiring early nail removal at 6 weeks due to skin lesions and pain. One boy had a fracture near the proximal nail insertion site. All patients regained a full range of motion and returned to daily life by the final follow-up. The retrograde double nail technique through a central entry point offers more advantages compared to the single nail technique, though the single nail technique is quicker and more cost-effective. However, the insertion of two nails provides better rotational stability [5,9]. Compared to conservative management, surgical intervention allows quicker recovery, and inconvenient immobilization can be avoided. Surgical fixation allows polytrauma patients with lower limb injuries to be mobilized earlier with the aid of assistive devices such as walkers and crutches. The key findings of all the studies are compared in Table 2. There are a few limitations in this study. The case series included only three patients who were operated on by a single surgeon. A multicentric study done over a longer period can provide more insights into how fractures treated by this method remodel over time.
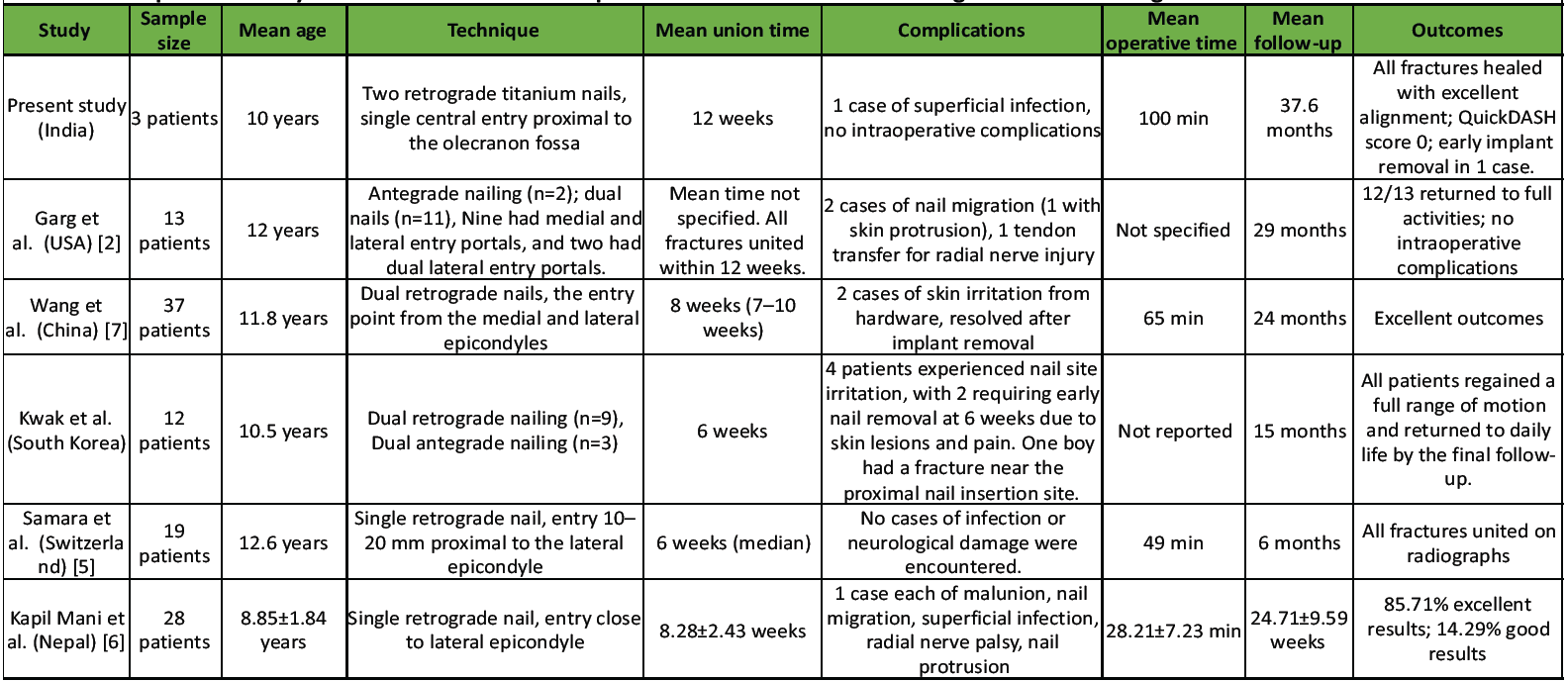
Table 2: Comparative analysis of outcomes and techniques from various studies on retrograde elastic nailing for humeral shaft fractures in children
Retrograde elastic nail fixation of humeral shaft fractures in children with two nails through a central entry point is a reliable technique, with a low risk of complications, offering stable fixation that eliminates the need for uncomfortable immobilization and enables early mobilization of the arm.
References
- 1. Herring JA. Upper extremity injuries. In: Herring JA, editor. Tachdjian’s Pediatric Orthopaedics. Philadelphia, PA: WB Saunders; 2002. p. 2132-8. [Google Scholar] [PubMed]
- 2. Webb L, Mooney J. Fractures and dislocations about the shoulder. In: Green N, Swiontkowski M, editors. Skeletal Trauma in Children. Philadelphia, PA: WB Saunders; 2003. p. 322-43. [Google Scholar] [PubMed]
- 3. Garg S, Dobbs MB, Schoenecker PL, Luhmann SJ, Gordon JE. Surgical treatment of traumatic pediatric humeral diaphyseal fractures with titanium elastic nails. J Child Orthop 2009;3:121-7. [Google Scholar] [PubMed]
- 4. Shazar N, Brumback RJ, Vanco B. Treatment of humeral fractures by closed reduction and retrograde intramedullary ender nails. Orthopedics 1998;21:641-6. [Google Scholar] [PubMed]
- 5. Lovell WW, Weinstein SL, Flynn JM, editors. Lovell Winters Pediatric Orthopaedics. 7th ed., Vol. 2. Philadelphia, PA: Wolters Kluwer Health, Lippincott Williams and Wilkins; 2014, p. 1704-5. [Google Scholar] [PubMed]
- 6. Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group. Development of the QuickDASH: Comparison of three item-reduction approaches. J Bone Joint Surg Am 2005;87:1038-46. [Google Scholar] [PubMed]
- 7. Samara E, Tschopp B, Kwiatkowski B, Vardar E, Lutz N, Zambelli PY. A single retrograde intramedullary nail technique for treatment of displaced proximal humeral fractures in children: Case series and review of the literature. JBJS Open Access 2021;6:e20.00119. [Google Scholar] [PubMed]
- 8. Kapil Mani KC, Acharya P, Pangeni BR, Marahatta SB. Pediatric humeral fracture fixed by a single retrograde titanium elastic nail. Apollo Med 2017;14:212-7. [Google Scholar] [PubMed]
- 9. Wang X, Shao J, Yang X. Closed/open reduction and titanium elastic nails for severely displaced proximal humeral fractures in children. Int Orthop 2013;38:107-10. [Google Scholar] [PubMed]
- 10. Kwak YH, Min SK, Lee YB, Park KB. Operative treatment of pediatric humeral diaphyseal fractures with flexible intramedullary nails. J Korean Orthop Assoc 2012;47:250-6. [Google Scholar] [PubMed]








