[box type=”bio”] What to Learn from this Article?[/box]
Degenerative spondylolisthesis can also occur at S1-S2.
Case Report | Volume 5 | Issue 3 | JOCR July-Sep 2015 | Page 90-91 | Thakre Kunwar Rajendra, Thomas Issac, B Mallikarjuna Swamy. DOI: 10.13107/jocr.2250-0685.320.
Authors: Thakre Kunwar Rajendra[1], Thomas Issac[1], B Mallikarjuna Swamy[1].
[1] Department of Orthopaedics, St. John’s Medical College and Hospital, Bengaluru, Karnataka, India.
Address of Correspondence
Dr. Thakre Kunwar Rajendra
Department of Orthopaedics, St. John’s Medical College and Hospital, Bengaluru – 560034, Karnataka, India. Email kunwar_thakre@yahoo.com
Abstract
Introduction: Degenerative spondylolisthesis (DS) is usually seen at L4-L5 level and less frequently at L5-S1 level. This is a rare case report of spondylolisthesis of S1 over S2 with lumbarization of S1. Lumbarization of S1 is seen in just 1-2% of the population and to have spondylolisthesis in this segment is even rarer. The purpose is to report a rare case of DS at S1-S2 level.
Case Report: This is a single case report of a 66-year-old gentleman who presented with complains of lower backache for 2 years and acute retention of urine to the emergency department. Detailed clinical and radiological evaluation of the spine was done which revealed lumbarization of S1 with spondylolisthesis at S1-S2 and facetal hypertrophy at L5, S1, and S2. He underwent decompression and stabilization at L5, S1, and S2 along with placement of autologous bone graft. The bladder symptoms disappeared after 3 weeks. At 1-year follow-up, patient’s clinical symptoms were relieved, and he improved clinically.
Conclusion: To the best of our knowledge, this is probably the first case of DS of sacral vertebrae to be reported in English literature. The prevalence of complete lumbarization is around 1.8% and to get spondylolisthesis in this segment is even rarer, hence the lack of literature in this regard. Since this is the first of its kind of case, further case series or longitudinal studies of such cases may help understand better the pathomechanics related to spondylolisthesis at this level.
Keywords: Sacrolisthesis, degenerative spondylolisthesis, lumbarization, sacralization.
Introduction
Spondylolisthesis is defined as an anterior migration of a vertebral body in relation to the vertebra located immediately caudal. In 1930 Junghanns was the first to describe anterior translation of a lumbar vertebra without any defect in the neural arch[1] following this the term ‘“degenerative spondylolisthesis (DS)” was introduced by Newman in 1955 [2].Five types of spondylolisthesis have been described including dysplastic, isthmic, traumatic, pathologic, and degenerative [3]. There are many predisposing factors like sagittally-placed facet joint, a high iliac crest [4-6], etc. DS which is characterized by an intact vertebral ring is presumed to result from degeneration of facet joints and intervertebral discs with aging [3,7] and thus has traditionally been considered to represent instability of the vertebral segment [7]. Here is a case report regarding this instability at S1-S2 level.
Case Report
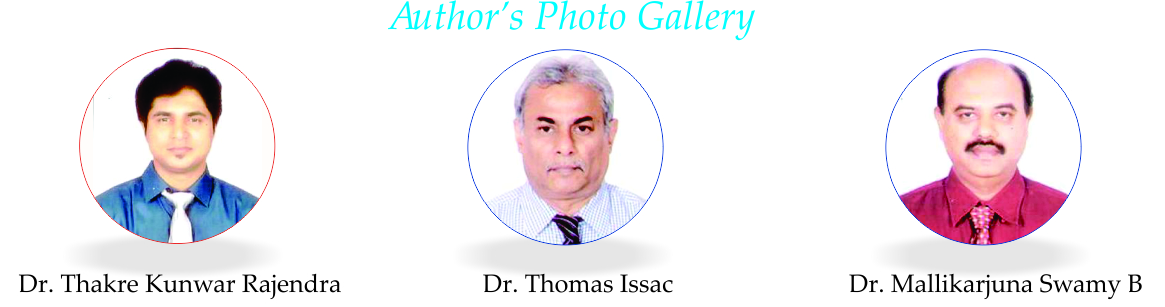
A 66-year-old gentleman, farmer by occupation, came with complaints of lower backache for 2 years which was insidious in onset, gradually progressive and non-radiating. He also complained of acute retention of urine since 15 days for which he was catheterized. He also had a history of neurogenic claudication at a distance of 100 m. There was no history of any trauma. A detailed systemic and neurological examination revealed power of flexor hallucis longus(FHL) and flexor digitalis longus(FDL) as 4/5, ankle jerks were absent, sensory deficits in S1-S2 dermatome and per-rectal examination revealed decreased perianal sensations and anal tone with absent anal wink. Hematological investigations did not reveal any abnormalities. Plain radiographs of lumbo-sacral spine revealed spondylolisthesis of S1-S2 (Meyerding’s grade 1) (Fig.1). Magnetic resonance imaging and computed tomography scan of the spine revealed lumbarization of S1 with spondylolisthesis of S1 over S2, facetal hypertrophy at L5-S1 and canal stenosis at S1-S2 (Figs.2,and 3).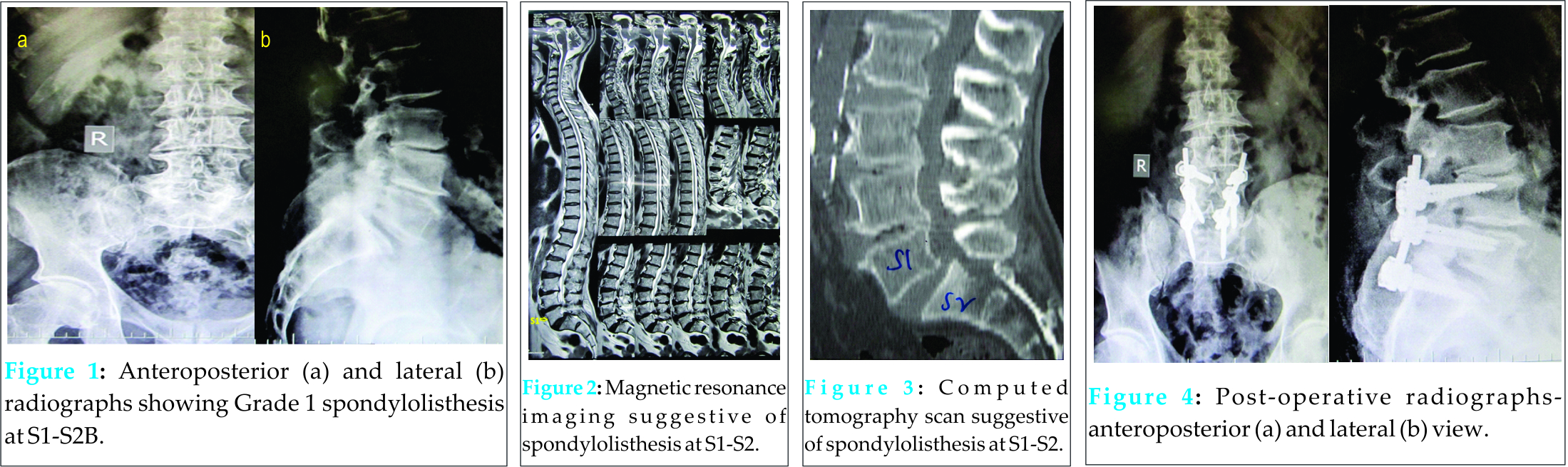
Operative procedure
The patient underwent posterior spine surgery where decompression was done with laminotomy of S1 bilaterally and then pedicular screw fixation was done bilaterally at L5, S1, and S2 (Fig.4). S1 and S2 fixation were difficult as the trajectory was inferior. Nerve roots were decompressed and inter-transverse autologous bone grafting was done.
Result
Soon after the surgery patient had relief of his presenting symptoms. The bladder symptoms disappeared after 3 weeks and the power of FHL/FDL improved from 4/5 to 5/5. The ankle jerk recovered to normal after 5 weeks. Latest follow-up of patient at 1year is satisfactory.
Discussion
DS usually occurs in patients older than 40 years. The deformity occurs at L4-5 6 times more often than at other lumbar levels and four times more often above a sacralized L5. L3-4 is affected more often than L5-S1 [8]. The lumbosacral junction and middle lumbar spine are most often involved, but the lesion is also found in cervical or rarely the thoracic vertebra [9]. To the best of our knowledge, DS of sacral vertebrae has not been reported in the available English literature till now. The prevalence of complete lumbarization is 1.8% [10] and to get a spondylolisthesis is even rarer. There have been many publications in the literature mentioning incidence of spondylolisthesis with sacralization but hardly any on spondylolisthesis with lumbarization.
Conclusion
There are few reports on traumatic spondylolisthesis [11] but probably none on DS. Further case series or longitudinal studies of such cases may help understand better the pathomechanics related to spondylolisthesis at this level.
Clinical Message
DS of S1-S2 is a very rare entity and further case reports will help us to explore the biomechanics at this level.
Reference
1. Junghanns H. Spondylolisthesen ohne spalt im Zwishengelenkstuck. Arch Orthop Unfall-Chir 1930;29:118-27.
2. Newman PH. Spondylolisthesis, its cause and effect. Ann R Coll Surg Engl 1955;16(5):305-23.
3. Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res 1976;(117):23-9.
4. Grobler LJ, Robertson PA, Novotny JE, Pope MH. Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology. Spine (Phila Pa 1976) 1993;18(1):80-91.
5. Cinotti G, Postacchini F, Fassari F, Urso S. Predisposing factors in degenerative spondylolisthesis. A radiographic and CT study. Int Orthop 1997;21(5):337-42.
6. Fitzgerald JA, Newman PH. Degenerative spondylolisthesis. J Bone Joint Surg Br 1976;58(2):184-92.
7. Rosenberg NJ. Degenerative spondylolisthesis. Predisposing factors. J Bone Joint Surg Am 1975;57(4):467-74.
8. Gardocki RJ, Camillo FX. Other disorders of the spine. Campbell’s Operative Orthopaedics.12thed, Vol.2. Ch. 44. Philadelphia, PA: Elsevier Mosby: 2013. p. 2006-9.
9. Metz LN, Deviren V. Low-grade spondylolisthesis. Neurosurg Clin N Am 2007;18(2):237-48.
10. Mahato NK. Morphological traits in sacra associated with complete and partial lumbarization of first sacral segment. Spine J 2010;10(10):910-5.
11. Rodriguez-Fuentes AE. Traumatic sacrolisthesis S1-S2. Report of a case. Spine (Phila Pa 1976) 1993;18(6):768-71.
| How to Cite This Article: Kunwar RT, Issac T, Swamy BM. Degenerative Sacrolisthesis of S1-S2: A Case Report. Journal of Orthopaedic Case Reports 2015 July – Sep;5(3): 90-91 . Available from: https://www.jocr.co.in/wp/2015/07/10/2250-0685-320-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com