Delayed fractures of the proximal tibia after tibial tubercle osteotomy are rare. Anticipation of this potential complication is highly recommended. An appropriate surgical technique and postoperative management are essential
Christian Quintart, Department of Orthopaedics and Traumatology, Hôpital de Jolimont-Lobbes, Rue Ferrer, 159, 7100 La Louvière, Belgium. E-mail: christianquintart@yahoo.fr
Introduction: Tibial tubercle osteotomy (TTO) is a surgical procedure commonly used. Several local postoperative complications have been identified in the literature, such as early proximal tibial fractures. In exceptional cases, these fractures can occur later in the postoperative period, i.e., after 6 months. The current paper described a case study of this rare delayed complication.
Case Report: An athletic 24-year-old military man was admitted to the emergency department following a spontaneous proximal tibial fracture below and arising from the TTO site realized 7 months earlier.
Conclusion: Delayed spontaneous fractures of the proximal tibia following TTO are extremely rare complications. This paper describes a case of delayed spontaneous fracture in a young athlete. Factors contributing to this fracture are analyzed. An adaptation of the surgical technique and rehabilitation protocol is discussed.
Keywords: Tibial tubercle osteotomy, complications, delayed tibial fracture, rehabilitation
Chronic patellar instability and focal patellofemoral osteoarthritis are well-known indications for tibial tubercle osteotomy (TTO). The procedure is also used in primary arthroplasties to improve limited flexion or to correct patellar implant positioning [1]. TTO allows a better surgical exposure while limiting the risk of patellar tendon avulsion in difficult revisions or primary arthroplasties. Reconstruction of the medial patellofemoral ligament and cartilage restoration can be associated with TTO. In cases of cartilage restoration, TTO should optimize the biomechanical environment of the new cartilage implant [2]. First of all, the procedure described by Elmslie-Trillat consists of a medial displacement of the tibial tuberosity (TT) to realign the extensor apparatus [3]. However, other TT displacements such as distalization, anteriorization (Maquet’s technique), or anteromedialization (Fulkerson’s technique) are also described and combinable [2,4]. Various local complications following TTO have been described. They include skin necrosis, malunion, loss of fixation, pseudarthrosis, persistent pain, arthrofibrosis and stiffness, progressive chondral deterioration, tuberosity fractures, and proximal tibial fractures [3,4,5,6]. Proximal tibial fractures are infrequent and most often occur within 8–14 postoperative weeks [5,6]. Cases of proximal tibial fractures 6 months after TTO are an exceptional occurrence. To our knowledge, only 3 cases of delayed fractures of the proximal tibia have been reported as complications of TTO [7,8]. This article reports the unusual case of a spontaneous fracture of the proximal tibia 7 months after TTO treating a chronic patellar instability. Factors contributing to this fracture were analyzed, enabling us to adapt our surgical technique and our future postoperative rehabilitation protocol.
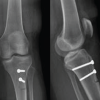
An athletic 24-year-old military man was surgically treated for an unstable and painful patella by performing a flat TTO associated with a medialization and distalization shift. The pre-operative knee injury and osteoarthritis outcome score (KOOS) were 72. The TT–trochlear groove distance (21 mm) and the Caton-Deschamps index (1.24) were normalized by the osteotomy. The chondral lesion present on the medial patellar facet was repaired using bone marrow-derived cells covered by a collagen membrane (Fig. 1). Fixation of the TT was achieved with two lag screws (4.5-mm diameter).
Postoperative care was simple. Weight-bearing was prohibited for 6 weeks. A removable knee extension splint and 2 crutches protected both the TTO and patellar cartilage repair.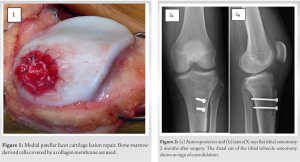
During the 1st month, the knee’s range of motion was gradually recovered, without exceeding 90° flexion. Isotonic knee locking exercises were postponed during 3–4 weeks while isometric contractions were encouraged. On his own initiative, the patient performed multiple isotonic locking exercises and frequent knee extension postures in addition to his rehabilitation program, for several weeks and months after surgery. The evolution was favorable both clinically and radiologically with a comeback to normal knee function at 3 months. However, a consolidation delay of the distal osteotomy cut was observed at 2 months (Fig. 2). 7 months after surgery, while walking around, the patient experienced severe pain at the operation site without sustaining apparent trauma. Weight-bearing was impossible.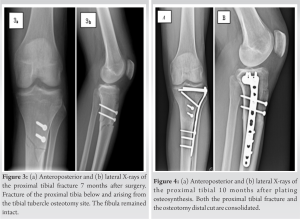
An emergency X-ray of the knee confirmed a spontaneous fracture of the proximal tibia below and arising from the TTO site. The fibula remained intact (Fig. 3). A plating osteosynthesis of the proximal tibia was carried out to avoid cast immobilization and to maintain knee’s function (Fig. 4). Weight-bearing was completely prohibited for 8 weeks while the range of motion was gradually recovered and completed after 2 weeks. A removable knee extension splint and 2 crutches protected the osteosynthesis for 8 weeks. Full weight-bearing and normal gait were obtained at 3 months. Both the proximal tibial fracture and the osteotomy distal cut were consolidated at 10 months after plating osteosynthesis (Fig. 4). KOOS score was, at that time, evaluated at 90.5.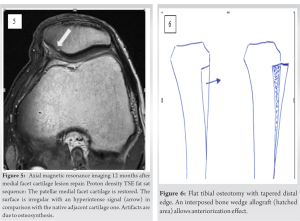
12 months after the medial cartilaginous facet repair, axial MR imaging revealed restored cartilage. However, the surface was slightly irregular with an hyperintense signal in comparison with the native adjacent cartilage one (Fig. 5). At 24-month post-implantation, the osteosynthesis plate was removed. Seven years after TTO, the patient had a full range of movement. The clinical results were good without limitations in daily activities; KOOS score was evaluated at 89.9.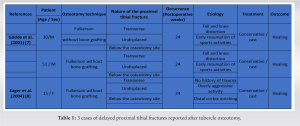
Proximal tibial fractures following TTO occur in 1–1.8% of cases [9,10]. The risk of fracture depends both on the osteotomy direction, relative to the coronal plane and its distal approach, but also on the postoperative rehabilitation protocol [10,11]. As shown in the cadaveric study conducted by Cosgarea et al. [12], mechanical stresses exerted in an oblique osteotomy (Fulkerson) will more frequently lead to a proximal tibial fracture, whereas mechanical stresses exerted in a flat osteotomy (Elmslie-Trillat) will more likely lead to a tuberosity fracture. The authors deduced that the greater the obliquity of the osteotomy cut in the frontal plane, the greater the stress on the proximal tibia and therefore the greater the risk of fracture. Stetson et al. [13] raised the possibility that overly aggressive oblique cutting in the proximal tibial metaphysis or in the posterior tibial cortex could be responsible of postoperative tibial fractures. In addition, the risk of fracture is higher in procedures requiring complete detachment of the osteotomy, such as a distalization shift [10]. Depending on surgically induced biomechanical changes, the distal approach of osteotomy is a significant element limiting the risk of proximal tibial fracture. Osteotomies which do not violate the anterior tibial cortex are associated with a lower fracture risk. Furthermore, osteotomies with a distal cut perpendicular to the anterior tibial cortex, thus violating the anterior tibial cortex, showed an increased fracture risk [8,14]. An adapted rehabilitation protocol can also prevent this risk [15]. Premature weight-bearing can cause proximal tibial fracture, especially before radiological confirmation of healing. It is therefore advisable to limit full weight-bearing for 6–8 weeks [6,15]. However, these instructions may not be sufficient to prevent delayed fracture risk, leading some practitioners to postpone resumption of activities involving heavy weight-bearing. Gödde et al. [7] first described two cases of proximal tibial fracture cases 24 weeks after Fulkerson osteotomy in athletes (Table 1). Nevertheless, weight-bearing was only allowed after bone consolidation at more than 10 weeks [7]. Authors suggested that jogging or any other activities such as contact sports or high-impact sports should be discouraged for at least 9–12 months after an anteromedialization osteotomy. They concluded that the effect of an oblique osteotomy on biomechanical properties of the proximal tibia outlasts the process of bony healing. Other cases of delayed tibial fracture after Fulkerson osteotomy have been described by Eager et al. [8]. However, among 5 reported cases, only one presented a delayed proximal tibial fracture after Fulkerson osteotomy (Table 1), proving the existence of a period of proximal tibial vulnerability which may exceed several weeks. According to the latter, vigorous activity should be suspended for a longer period, even after clear and observable consolidation of the osteotomy.
Authors also strongly recommend tapering the distal edge of the osteotomy. This would minimize the vulnerability of this area. Bone grafting at the osteotomy site would facilitate consolidation. Our patient’s case also suggests a proximal tibial vulnerability several months after flat osteotomy (Elmslie-Trillat). This has led us to modify our subsequent surgical technique by tapering the distal edge of the osteotomy and sparing the anterior tibial cortex to take proximal tibial biomechanical properties into account [8,10,11]. If an anteriorization effect is desired, we suggest to interpose a bone wedge allograft between the tibia and the flat osteotomy, allowing tubercle advancement and avoiding the oblique cut of Fulkerson osteotomy (Fig. 6). Medialization and distalization effects are also possible with this surgical technique. The prevention of tibial fractures has to integrate postoperative rehabilitation instructions and stringent advice adapted to the mechanical characteristics of the chosen osteotomy procedure. In our case, multiple locking quadricipital exercises, extension postures, and stretching undoubtedly contributed to the chronic proximal tibial weakness. In addition to 6–8 non-weight-bearing weeks and the wearing of a removable knee extension splint, hard sport activities, contact sports, or sports generating high-impact forces should be prohibited for 9–12 months [7,8,15].
Delayed spontaneous fractures of the proximal tibial following TTO are rare but severe complications. An adaptation of the surgical technique and rehabilitation protocol is necessary to avoid this risk. A flat TTO technique with tapered distal edge is preferred to osteotomies that violate the posterior or the anterior cortex of the proximal tibia. Even if the X-ray shows the healing of the osteotomy site, vigorous activities, contact, or high-impact sports should be prohibited for 9–12 months.
Tibial tubercle osteotomy is frequently performed in case of chronic patellar instability, focal patellofemoral osteoarthritis or to allow a better surgical exposure in cases of primary or revision joint replacements. However, performing a tibial tubercle osteotomy weakens the proximal tibia; this can lead to an early or much more rarely delayed fracture of the proximal tibia. An appropriate surgical technique and postoperative management are essential to avoid this deplorable complication.
References
- 1.Piedade SR, Pinaroli A, Servien E, Neyret P. Tibial tubercle osteotomy in primary total knee arthroplasty: A safe procedure or not? Knee 2008;15:439-46. [Google Scholar | PubMed]
- 2.Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J 2nd, Bach BR Jr, et al. Tibial tuberosity osteotomy: Indications, techniques, and outcomes. Am J Sports Med 2014;42:2006-17. [Google Scholar | PubMed]
- 3.Trillat A, Dejour H, Couette A. Diagnosis and treatment of recurrent dislocations of the patella. Rev Chir Orthop Reparatrice Appar Mot 1964;50:813-24. [Google Scholar | PubMed]
- 4.Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res 1983;177:176-81. [Google Scholar | PubMed]
- 5.Johnson AA, Cosgarea AJ, Wolfe EL. Complications of tibial tuberosity osteotomy. Sports Med Arthrosc Rev 2017;25:85-91. [Google Scholar | PubMed]
- 6.Bellemans J, Cauwenberghs F, Brys P, Victor J, Fabry G. Fracture of the proximal tibia after Fulkerson anteromedial tibial tubercle transfer. A report of four cases. Am J Sports Med 1998;26:300-2. [Google Scholar | PubMed]
- 7.Gödde S, Rupp S, Dienst M, Seil R, Kohn D. Fracture of the proximal tibia six months after Fulkerson osteotomy. A report of two cases. J Bone Joint Surg Br 2001;83:832-3. [Google Scholar | PubMed]
- 8.Eager MR, Bader DA, Kelly JD 4th, Moyer RA. Delayed fracture of the tibia following anteromedialization osteotomy of the tibial tubercle: A report of 5 cases. Am J Sports Med 2004;32:1041-8. [Google Scholar | PubMed]
- 9.Saltzman BM, Rao A, Erickson BJ, Cvetanovich GL, Levy D, Bach BR Jr, et al. A systematic review of 21 tibial tubercle osteotomy studies and more than 1000 knees: Indications, clinical outcomes, complications, and reoperations. Am J Orthop (Belle Mead NJ) 2017;46:E396-407 [Google Scholar | PubMed]
- 10.Payne J, Rimmke N, Schmitt LC, Flanigan DC, Magnussen RA. The incidence of complications of tibial tubercle osteotomy: A systematic review. Arthroscopy 2015;31:1819-25. [Google Scholar | PubMed]
- 11.Koëter S, Diks MJ, Anderson PG, Wymenga AB. A modified tibial tubercle osteotomy for patellar maltracking: Results at two years. J Bone Joint Surg Br 2007;89:180-5. [Google Scholar | PubMed]
- 12.Cosgarea AJ, Schatzke MD, Seth AK, Litsky AS. Biomechanical analysis of flat and oblique tibial tubercle osteotomy for recurrent patellar instability. Am J Sports Med 1999;27:507-12. [Google Scholar | PubMed]
- 13.Stetson WB, Friedman MJ, Fulkerson JP, Cheng M, Buuck D. Fracture of the proximal tibia with immediate weightbearing after a Fulkerson osteotomy. Am J Sports Med 1997;25:570-4. [Google Scholar | PubMed]
- 14.Luhmann SJ, Fuhrhop S, O’Donnell JC, Gordon JE. Tibial fractures after tibial tubercle osteotomies for patellar instability: A comparison of three osteotomy configurations. J Child Orthop 2011;5:19-26 [Google Scholar | PubMed]
- 15.Salari N, Horsmon GA, Cosgarea AJ. Rehabilitation after anteromedialization of the tibial tuberosity. Clin Sports Med 2010;29:303-11, ix. [Google Scholar | PubMed]