This case report highlights the importance of recognizing and addressing mechanical complications associated with specific prosthesis models in reverse total shoulder arthroplasty.
Dr. Gazi Huri, Department of Orthopaedics and Traumatology, Hacettepe University Faculty of Medicine, Ankara, Turkey. E-mail: gazihuri@yahoo.com
Introduction: The evolution of prosthesis design has increased the frequency of RTSA procedures across various indications. This rise in surgeries has also led to a growing number of associated complications. This case report highlights an unusual occurrence: a mechanical failure of a RTSA at the humeral stem tray.
Case Report: A 55-year-old male patient was admitted to our hospital with a sharp pain after 2 years of his initial reverse total shoulder arthroplasty (RTSA) surgery. A broken humeral stem of the RTSA was diagnosed on the plain radiography and the patient underwent a one-stage revision. Further complications have not arisen during his follow-up to date and the patient has a nearly full range of motion.
Conclusion: Although a humeral stem tray failure is a rarely seen complication for shoulder arthroplasty, surgeons who have used this model prosthesis should be aware that they may encounter such a complication.
Keywords: Case report, humeral stem, revision, reverse total shoulder arthroplasty, implant failure.
Although reverse total shoulder arthroplasty (RTSA) was originally designed for rotator cuff tear arthropathy in elderly patients, indications have been widened from osteoarthritis to irreparable rotator cuff tears and three or four-part proximal humeral fractures in recent years [1,2]. Improvement of the prosthesis design has let the surgeons to use RTSA more often in different kinds of indications but as the number of operations increased, a number of complications also followed this increase meanwhile [3]. Herein, we report a very unusual case, a mechanical failure of a RTSA at the humeral stem tray, which is a rarely seen complication in the literature. A written consent was obtained from the patient to publish his data.
A 55-year-old male applied to our clinic with a sudden pain in his right shoulder, 2 years after a reverse total shoulder arthroplasty (RTSA) in another hospital due to rotator cuff arthropathy. He was a gardener and returned to his work after 2 months of the operation. His range of motion (ROM) was improved and had no pain in his daily activities after several months. However, almost 2 years from the initial surgery, he suddenly felt extreme pain in his shoulder when he tried to operate a vacuum cleaner. He applied to our clinic after trying painkillers for 3 weeks. A sharp pain in the shoulder, restrained ROM, and a loosening-like feeling were his major complaints at his admission with a normal neurovascular examination and without any comorbidities. Plain radiographs of his shoulder were taken and a RTSA with a broken humeral stem was determined (Fig. 1).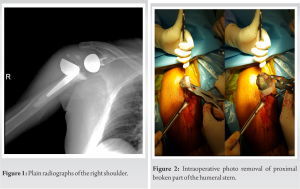 Further evaluation was done with a computed tomography of the right shoulder to evaluate any occult fracture around the shoulder girdle and bony fracture was excluded from the study. A one-stage operation was planned for revision. We used the previous incision line for the deltopectoral approach. After reaching the glenohumeral joint, the prosthesis was found to be dislocated and broken at the humeral tray of proximal stem. The model itself was a modular stem and due to the suspicion of infection, samples were taken from the surrounding synovium and joint fluid. Metallosis and debris tissue were debrided. The humeral stem and the glenoid hemisphere were removed with its cement (Fig. 2 and 3) and a cemented long humeral stem (SMR, Lima LTO, Udine, Italy) was placed (Fig. 4).
Further evaluation was done with a computed tomography of the right shoulder to evaluate any occult fracture around the shoulder girdle and bony fracture was excluded from the study. A one-stage operation was planned for revision. We used the previous incision line for the deltopectoral approach. After reaching the glenohumeral joint, the prosthesis was found to be dislocated and broken at the humeral tray of proximal stem. The model itself was a modular stem and due to the suspicion of infection, samples were taken from the surrounding synovium and joint fluid. Metallosis and debris tissue were debrided. The humeral stem and the glenoid hemisphere were removed with its cement (Fig. 2 and 3) and a cemented long humeral stem (SMR, Lima LTO, Udine, Italy) was placed (Fig. 4). The glenohumeral joint was then reduced and the layers were anatomically closed. No post-operative complications were spotted. The synovial culture which had been taken for the suspicion of an infection was reported sterile. A frozen section analysis revealed active chronic synovitis, fibrosis, and giant cell reaction of foreign bodies. Shoulder physiotherapy with ROM and strengthening exercises were applied to the patient for 3-month postoperatively. No complication has occurred during his 3-year follow-up after surgery and the patient has nearly full ROM with only 20° of loss in abduction and has neither pain nor complaints. The patient was satisfied with result of the treatment and gained full function of his right shoulder.
The glenohumeral joint was then reduced and the layers were anatomically closed. No post-operative complications were spotted. The synovial culture which had been taken for the suspicion of an infection was reported sterile. A frozen section analysis revealed active chronic synovitis, fibrosis, and giant cell reaction of foreign bodies. Shoulder physiotherapy with ROM and strengthening exercises were applied to the patient for 3-month postoperatively. No complication has occurred during his 3-year follow-up after surgery and the patient has nearly full ROM with only 20° of loss in abduction and has neither pain nor complaints. The patient was satisfied with result of the treatment and gained full function of his right shoulder.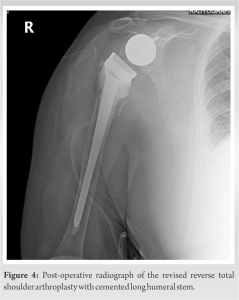
The overall complication rate of primary RTSA has been reported at between 5% and 25% and even higher in revision cases, up to 60% [4,5]. Due to extended indications, patients and orthopedic surgeons are facing complications more often in the recent years [6]. Instability, implant loosening, intraoperative or post-operative periprosthetic fracture, deltoid weakness, neurological injuries, and infection are the main complications. Among them, instability is the most common complication seen in the primary RTSA and an increasing periprosthetic fracture incidence was also observed with the aging population [7]. Among patient-related factors, smoking and male gender seem to increase risk of complications such as infection and dislocation [4]. Some studies claim that the type of prosthesis originally used may have an impact on the rates of subsequent operations [8]. Prostheses with longer stems are viable options when faced with a lack of proximal humeral bone stock and short stem or stemless designs provide shorter operative time, less blood loss, bone preservation, ease of revision, and the potential to reduce both periprosthetic fractures and stress shielding [9]. In this case, we reported a very uncommon cause of post-operative complication in RTSA with a specific prosthesis model. According to the best of our knowledge, humeral stem failure at humeral tray is a very rare complication in RTSA literature. The humeral stem failures in the literature have been reported from a particular modular reverse shoulder system manufactured by Biomet (Comprehensive Reverse Shoulder System) in 2010. The failure was caused by a problem at the design and production stage of humeral tray and this specific model of reverse shoulder arthroplasty recalled by Zimmer-Biomet in 2017 [10]. First, Lewicki et al. published an article about in vivo fatigue cracks in models whose humeral trays were produced with titanium alloy [11]. An electron microscopic analysis and a finite element simulation revealed high-stress concentration at the titanium humeral tray with a possible failure less than a year in vivo [12]. These findings were also clinically proven with the case series published by McDonald et al. Five patients with six humeral tray failures were reported from 300 patients operated by this specific RTSA model. One patient underwent a second revision for the same humeral stem failure. Although a finite element analysis by McDonald et al. revealed that the mechanical failure usually occurs in the 1st year after RTSA surgery [13]. The reported case in this paper underwent one-stage revision surgery, during which the dislocated and broken prosthesis was removed, and a cemented long humeral stem was implanted. The occurrence of stem fractures in the shoulder joint is uncommon, as the shoulder does not bear heavy cyclic loads like the hip and knee but may have been accelerated by the patient’s occupation as a gardener, which involved frequent use of the upper extremity and higher cyclic loads compared to elderly patients. Although previous studies have identified risk factors for stem failures in joint arthroplasty, such as patient age, gender, implant design, and material quality; advances in technology and material sciences have reduced the incidence of such failures, but rare cases still occur [14,15]. It underscores the need for ongoing research and improvements in implant design, material selection, and surgical techniques to optimize patient outcomes and minimize the risk of mechanical failures in shoulder arthroplasty procedures. Since the patient’s primary reverse shoulder prosthesis was performed by another center, we have no information about the intraoperative situation and the accuracy and inaccuracy of the surgical technique, which is the weakness of the study. There was neither any biomechanical study nor reported similar case reports of this specific prosthesis model. We reported the failure and sent the broken humeral stem to the manufacturer for examination. Knowing the brand model of the prosthesis and being able to remove all the parts completely during surgery are among the strengths of our report.
The patient had a successful outcome, with no post-operative complications, nearly full range of motion, minimal loss in abduction, and no pain or complaints during a 3-year follow-up period. This specific model is not under production anymore, but it is known that it was used in many patients during the 2010. The investigation will reveal whether it is a one-time event or if all the same model prosthesis is at risk. Shoulder surgeons should be aware of this very rare complication, especially when using modular prostheses which have trays to connect the stem and modular head. This case report highlights the importance of recognizing and addressing mechanical complications associated with specific prosthesis models in RTSA.
Although the shoulder joint does not carry heavy cyclic loads as hip or knee joints do, implant failure can rarely be seen in conjunction with design/material problems. Orthopedic surgeons should be aware of improper design or manufacturing of the modular RTSA designs, which can lead to mechanical complications in shoulder arthroplasty patients.
References
- 1.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 1993;16:65-8. [Google Scholar | PubMed]
- 2.Baulot E, Sirveaux F, Boileau P. Grammont’s idea: The story of Paul Grammont’s functional surgery concept and the development of the reverse principle. Clin Orthop Relat Res 2011;469:2425-31. [Google Scholar | PubMed]
- 3.Villacis D, Sivasundaram L, Pannell WC, Heckmann N, Omid R, Hatch GF 3rd. Complication rate and implant survival for reverse shoulder arthroplasty versus total shoulder arthroplasty: Results during the initial 2 years. J Shoulder Elbow Surg 2016;25:927-35. [Google Scholar | PubMed]
- 4.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg 2011;20:146-57. [Google Scholar | PubMed]
- 5.Ma GC, Bradley KE, Jansson H, Feeley BT, Zhang AL, Ma CB. Surgical complications after reverse total shoulder arthroplasty and total shoulder arthroplasty in the United States. J Am Acad Orthop Surg Glob Res Rev 2021;5:e21.00146. [Google Scholar | PubMed]
- 6.Saltzman BM, Chalmers PN, Gupta AK, Romeo AA, Nicholson GP. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:1647-54. [Google Scholar | PubMed]
- 7.Canton G, Fazzari F, Fattori R, Ratti C, Murena L. Post-operative periprosthetic humeral fractures after reverse shoulder arthroplasty: A review of the literature. Acta Biomed 2019;90:8-13. [Google Scholar | PubMed]
- 8.Baram A, Ammitzboell M, Brorson S, Olsen BS, Amundsen A, Rasmussen JV. What factors are associated with revision or worse patient-reported outcome after reverse shoulder arthroplasty for cuff-tear arthropathy? A study from the Danish shoulder arthroplasty registry. Clin Orthop Relat Res 2020;478:1089-97. [Google Scholar | PubMed]
- 9.Upfill-Brown A, Satariano N, Feeley B. Stemless shoulder arthroplasty: Review of short and medium-term results. JSES Open Access 2019;3:154-61. [Google Scholar | PubMed]
- 10.Class 1 Device Recall Biomet Comprehensive Reverse Shoulder Humeral. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfres/res.cfm?id=151859 [Last accessed on 2023 May 27]. [Google Scholar | PubMed]
- 11.Lewicki KA, Martin AJ, Bell JE, Van Citters DW. Fatigue failure of reverse shoulder humeral tray components of a single design. J Shoulder Elbow Surg 2016;25:1288-96. [Google Scholar | PubMed]
- 12.MacDonald PB, Petrak MJ, Gascoyne TC, Bohm ER. In vivo fracture of a reverse total shoulder replacement humeral tray: A case report. Proc Inst Mech Eng H J Eng Med 2016;230:1141-7. [Google Scholar | PubMed]
- 13.McDonald LS, Dines JS, Chin C, Warren RF, Dines DM. Humeral tray-taper failure in modular reverse total shoulder arthroplasty. HSS J 2016;12:8-12. [Google Scholar | PubMed]
- 14.14. Bitzer A, Rojas J, Patten IS, Joseph J, McFarland EG. Incidence and risk factors for aseptic baseplate loosening of reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2018;27:2145-52. [Google Scholar | PubMed]
- 15.Mahony GT, Werner BC, Chang B, Grawe BM, Taylor SA, Craig EV, et al. Risk factors for failing to achieve improvement after anatomic total shoulder arthroplasty for glenohumeral osteoarthritis. J Shoulder Elbow Surg 2018;27:968-75. [Google Scholar | PubMed]