Robotic-assisted TKA offers an attractive alternative for large femoral cystic lesions, optimizing component positioning, fixation, and bone stock preservation.
Dr. Nicolas S Piuzzi, Department of Orthopaedic Surgery, Orthopaedic and Rheumatologic Institute, Cleveland Clinic, Cleveland, Ohio, USA. E-mail: piuzzin@ccf.org
Introduction: Subarticular cystic lesions, also known as geodes, present a challenge in the management of patients undergoing primary total knee arthroplasty (TKA). Although multiple treatment options are available for addressing these lesions, uncertainty persists regarding the optimal approach.
Case Report: A 58-year-old man with a history of rheumatoid arthritis presented with several years of left knee pain. Evaluation showed severe left knee degenerative osteoarthritis complicated by the presence of a large lateral femoral condyle cyst. After failing conservative management, a robotic-assisted cementless cruciate-retaining TKA was indicated. The large bone cyst was managed with augmentation using synthetic bone grafting. 1 year postoperatively, he showed excellent clinical outcomes and radiographic evidence of osteointegration.
Conclusion: This case highlights the value of robotic-assisted technology to plan and execute bone grafting of a large femoral cystic lesion while performing TKA with primary components. A computed tomography-imaged robotic TKA offers the potential benefit of screening bone cysts and thus planning a surgical approach in which bone preservation can be maximized.
Keywords: Robotic arthroplasty, geode, bone cyst, injectable regenerative graft, bone void filler.
Rheumatoid arthritis (RA) is a systemic, autoimmune, inflammatory arthritis that affects 1–2% of the population [1]. These patients can develop subarticular cystic lesions, known as geodes [1]. These lesions are usually solitary and involve major bone loss compared to subchondral cysts in osteoarthritis [2]. There are several available options for managing these large lesions during primary total knee arthroplasty (TKA), including the use of cement with screws, autologous bone graft, morselized or bulk structural allograft, modular wedges, metallic augments, porous metal cones or sleeves [3]. They also frequently require more invasive revision TKA implants with stem fixation [4,5]. However, it remains unclear which treatment approach is the most effective for managing large bony cysts. The use of robotic TKA in knee arthroplasties has increased significantly in recent years, with the possibility of representing 50% of all knee arthroplasties in the United States by 2030 [1,6,7]. Robotic assistance in TKA has been shown to have several advantages over conventional TKA, including improved accuracy and precision in implant placement as well as greater reliability in restoring a neutral mechanical axis [8,9,10,11,12]. However, its cost efficiency and value are still to be determined [11]. One potential additional benefit of using computed tomography (CT) imaging with robotic TKA is the ability to screen for bone cysts. It may therefore be advantageous to adopt a robotic-assisted total knee replacement (RA) to manage large bone cysts as it offers a more bone-preserving approach. Bone grafting is one of the most common treatment options for bone loss in joint arthroplasty [13]. Particularly, synthetic resorbable bone graft substitutes (SBGS) have gained popularity in orthopedics, demonstrating positive outcomes [14,15]. Furthermore, their utilization offers several advantages, including minimally invasive application, abundance, reliable injectability, rapid osteointegration, and no donor site morbidity [15]. Therefore, for large bone cysts, SBGS may provide an effective treatment option in filling the void and stimulating osteointegration [16]. Here, we present a case of knee osteoarthritis with a large lateral femoral condyle cyst managed with robotic-assisted primary cementless cruciate retaining (CR) TKA with augmentation using synthetic bone grafting.
A 58-year-old male with a history of RA presents with left knee osteoarthritis and an associated large bone cyst in the lateral femoral condyle.
History
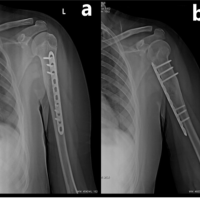
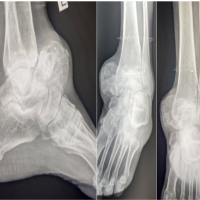
The patient initially presented at age 57 with symptomatic primary osteoarthritis of the left knee for the past 10 + years. He reported pain limiting activity and sleep, lack of full knee extension, and impaired ambulation. Symptoms were refractory to conservative treatments, including weight loss, over-the-counter NSAIDs, corticosteroid injections, a full course of physical therapy, and a prior synovectomy. On examination, body mass index was 31. Left knee alignment was neutral. Range of motion was 5°–120° with no extension lag. The knee was stable to varus/valgus and anterior/posterior stress. Left hip examination was unremarkable. Left knee radiographs showed severe tricompartmental degeneration with tricompartmental osteophytes, joint space narrowing, and multiple intraarticular loose bodies (Fig. 1). CT showed a large lytic lesion involving most of the lateral femoral condyle, with no aggressive features, most consistent with a benign bone cyst (Fig. 2). After extensive discussion of non-surgical and surgical options, the patient elected to undergo left robotic-assisted TKA, including bone cyst debridement and grafting. The decision to use a cementless knee prosthesis in this case was driven by the patient’s relatively young age, the need to preserve bone stock, and the potential benefits of osteointegration. The possibility of requiring revision TKA implants was discussed.
CT showed a large lytic lesion involving most of the lateral femoral condyle, with no aggressive features, most consistent with a benign bone cyst (Fig. 2). After extensive discussion of non-surgical and surgical options, the patient elected to undergo left robotic-assisted TKA, including bone cyst debridement and grafting. The decision to use a cementless knee prosthesis in this case was driven by the patient’s relatively young age, the need to preserve bone stock, and the potential benefits of osteointegration. The possibility of requiring revision TKA implants was discussed.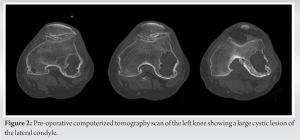
Pre-operative planning
Extensive pre-operative planning was undertaken to address the technical challenges faced by this case. Planning objectives were to aim for a CR construct to minimize bone resection (Fig. 3). Alternative plans were made for stemmed posterior stabilized (PS), and total stabilized (TS) constructs with the use of femoral stem as needed. Pre-operative CT scanning was performed using the standard RA-TKA protocol (Stryker Mako, Mahwah, NJ). CT characterized a cystic lesion measuring 5 cm in its axial dimension. The resulting anatomical models demonstrated severe medial and lateral compartment osteoarthritis with genu valgus alignment.
Robotic-assisted TKA
After standard preparation for knee arthroplasty, the left knee was exposed using a limited anterior-midline incision. A median para-patellar arthrotomy was performed and standard procedure was followed to expose and register the knee for robotic arthroplasty. Assessment of the knee joint revealed severe end-stage articular damage with no remaining medial weight-bearing cartilage. The lateral compartment was severely eburnated with bone loss on the posterior tibia and posterior femoral condyles, resulting in the valgus deformity. Soft-tissue balance was performed, the pre-operative robotic plan was updated accordingly, and the robotic arm was utilized to execute the planned cuts. The patella was assessed and showed minimal degenerative changes, midline tracking, and no instability, so the decision was made not to resurface it. The bone defect in the lateral femoral condyle was then assessed and debrided from the membrane. The bone cyst was found to compromise 30–40% of the distal femoral cut. A decision had to be made between bone grafting and aiming for a CR construct or choosing a PS or TS construct with a stem. To avoid removing a substantial amount of host bone from a healthy medial and central aspects of the femur to prepare for the femoral box, we decided to proceed with bone grafting the cyst and placing a primary CR cementless femoral component (Fig. 4). The graft used consisted of autologous bone obtained from the cuts and 22 cc of a CSH/brushite/β-TCP graft containing 75% calcium sulfate (CaS) and 25% calcium phosphate (Pro-Dense™, Wright Medical Technology Inc., Memphis, TN) and it was placed in a doughy state (Fig. 4). Final implants were placed showing excellent press-fit, tracking, and stability with a 9-mm CS polyethylene. The extensor mechanism and capsule were anatomically repaired and range of motion was 0–135 without excessive stress. Standard skin closure was followed and the patient recovered adequately in PACU.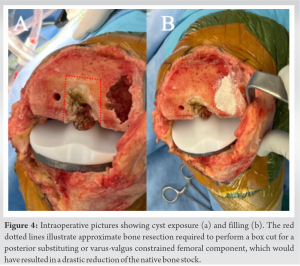
Post-operative course
Post-operatively, weight bearing was protected to 25% body weight with a walker for the first 4 weeks and increased gradually until full weight bearing on week 12. He otherwise followed the standard post-operative TKA physical therapy protocol, starting as an inpatient on post-operative day 1 and continuing at home.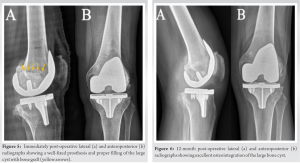
Follow-up
At 1-year follow-up, he reported no pain and no activity limitations. He has no effusion, tenderness, or instability. He has achieved 0°–120° knee range of motion without pain. Radiographs show well-fixed TKA with radiographic evidence of osteointegration and no osteolysis (Fig. 5 and 6).
Large subchondral cysts are common in osteoarthritic knees of RA patients [1]. Due to bone resorption caused by bone cysts and overall poor bone quality in these patients, treatment strategies should be tailored to optimize bone stock. A limited number of cases has been reported in the literature regarding the treatment of bone cysts in an osteoarthritic knee [16,17,18]. Moreover, only one case has been described using SBGS and TKA for the treatment of bony cysts. Thiery et al. [16] described a case of a male patient with a large lateral femoral condyle cyst. He was treated with curettage, filling with a CaS/HA bone graft substitute composed of 40% HA and 60% CaS (Cerament, Bonesupport, Lund, Sweden) and primary CR TKA. At 4 months post-operatively, they reported complete osseointegration of the bone graft. However, the patient developed arthrofibrosis and eventually required revision. In planning for TKA in patients with large bone cysts, management options usually involve revision implants with more invasive constructs [4,5]. Therefore, the use of robotic-assisted TKA may help to obtain reliable component positioning and optimal lower leg alignment. It is also possible to use a CT scan as a pre-operative tool to screen, detect, and delineate bony cysts to maximize bone preservation during surgical planning [19]. It should be noted that bone preservation was also a consideration in the decision to place a cementless CR prosthesis. Indeed, cementless prostheses have shown several advantages over cemented prostheses, such as better bone stock preservation, avoidance of cement debris, decreased operative time, and the potential value of osteointegration [20]. Moreover, selecting a femoral CR was preferred as PS designs which would have required a box cut (Fig. 4). As a result of this box cut, the intercondylar notch would have been further weakened and the cyst defect would have been connected, creating a massive bone defect and increasing the risk of periprosthetic fractures [21]. The use of robotic technology allowed the surgery to be performed without the placement of an endomedullary femoral rod, which is often necessary in manual TKA procedures. Performing this maneuver could have further debilitated or increased bone loss in the distal femur, thus jeopardizing the possibility of performing the surgery using primary components. Then, SBGS was chosen based on favorable clinical results and the mechanical properties that it provides once it sets [22,23,24]. For instance, Evaniew et al. [22] demonstrated rapid radiographic integration and early return to activities of daily living in patients with primary benign bone tumors. These observations are in agreement with our patient’s last follow-up, which showed excellent clinical outcomes and 1-year X-rays displaying a well-fixed prosthesis with graft oteointegration without impairing mechanical stability (Fig. 6). In sum, we presented the case of a rheumatoid patient with a large lateral femoral condyle cyst that was managed with robotic-assisted cementless CR TKA and augmentation with SBGS. Our approach limited the amount of healthy bone loss and ensured optimal component positioning and fixation in his altered anatomy. At 1-year follow-up, clinical and radiographic results are promising, suggesting that this approach may offer a bone-preserving and effective treatment option. Finally, CT-imaged robotic TKA offers the potential added benefit of screening bone cysts and thus planning a surgical approach in which bone preservation can be maximized.
This case highlights the value of robotic-assisted technology to plan and execute bone grafting of a large femoral cystic lesion while performing TKA with primary components. A computed tomography-imaged robotic TKA offers the potential benefit of screening bone cysts and thus planning a surgical approach in which bone preservation can be maximized.
The presented case underscores the significant role of robotic-assisted technology in facilitating the use of primary components and bone grafting for the management of a large femoral cystic lesion during TKA. Utilizing CT-imaged robotic TKA, clinicians can effectively identify and evaluate bone cysts, enabling the formulation of a surgical strategy focused on optimal bone preservation. This approach holds promise for enhancing surgical planning and execution, ultimately improving patient outcomes.
References
- 1.Sigmund A, Russell LA. Optimizing rheumatoid arthritis patients for surgery. Curr Rheumatol Rep 2018;20:48. [Google Scholar | PubMed]
- 2.Ostrowska M, Maśliński W, Prochorec-Sobieszek M, Nieciecki M, Sudoł-Szopińska I. Cartilage and bone damage in rheumatoid arthritis. Rheumatology 2018;56:111-20. [Google Scholar | PubMed]
- 3.Siddiqi A, Chen AF, Piuzzi NS, Kelly MA. The use of metaphyseal cones and sleeves in revision total knee arthroplasty. J Am Acad Orthop Surg 2021;29:e904-20. [Google Scholar | PubMed]
- 4.Sheth NP, Bonadio MB, Demange MK. Bone loss in revision total knee arthroplasty: Evaluation and management. J Am Acad Orthop Surg 2017;25:348-57. [Google Scholar | PubMed]
- 5.Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: Defect classification and alternatives for reconstruction. Instr Course Lect 1999;48:167-75 [Google Scholar | PubMed]
- 6.Emara AK, Zhou G, Klika AK, Koroukian SM, Schiltz NK, Higuera-Rueda CA, et al. Is there increased value in robotic arm-assisted total hip arthroplasty?: A nationwide outcomes, trends, and projections analysis of 4,699,894 cases. Bone Joint J 2021;103-B:1488-96. [Google Scholar | PubMed]
- 7.Rullán PJ, Zhou G, Emara AK, Klika AK, Koroukian S, Piuzzi NS. Understanding rates, risk factors, and complications associated with manipulation under anesthesia after total knee arthroplasty (TKA): An analysis of 100,613 TKAs. Knee 2022;38:170-7. [Google Scholar | PubMed]
- 8.Siddiqi A, Mont MA, Krebs VE, Piuzzi NS. Not all robotic-assisted total knee arthroplasty are the same. J Am Acad Orthop Surg 2021;29:45-59. [Google Scholar | PubMed]
- 9.Emara AK, Zhou G, Klika AK, Koroukian SM, Schiltz NK, Krebs VE, et al. Robotic-arm-assisted knee arthroplasty associated with favorable in-hospital metrics and exponentially rising adoption compared with manual knee arthroplasty. J Am Acad Orthop Surg 2021;29:e1328-42. [Google Scholar | PubMed]
- 10.Siddiqi A, Horan T, Molloy RM, Bloomfield MR, Patel PD, Piuzzi NS. A clinical review of robotic navigation in total knee arthroplasty: Historical systems to modern design. EFORT Open Rev 2021;6:252-69. [Google Scholar | PubMed]
- 11.Rajan PV, Khlopas A, Klika A, Molloy R, Krebs V, Piuzzi NS. The cost-effectiveness of robotic-assisted versus manual total knee arthroplasty: A markov model-based evaluation. J Am Acad Orthop Surg 2022;30:168-76. [Google Scholar | PubMed]
- 12.Rothfusz CA, Emara AK, Piuzzi NS, Bloomfield MR. Robotic arm-assisted total knee arthroplasty in the setting of severely deficient distal femoral bone stock. JBJS Case Connector 2021;12;11(3) [Google Scholar | PubMed]
- 13.Shafaghi R, Rodriguez O, Schemitsch EH, Zalzal P, Waldman SD, Papini M, et al. A review of materials for managing bone loss in revision total knee arthroplasty. Mater Sci Eng C Mater Biol Appl 2019;104:109941. [Google Scholar | PubMed]
- 14.Wang W, Yeung KW. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioact Mater 2017;2:224-47. [Google Scholar | PubMed]
- 15.Baldwin P, Li DJ, Auston DA, Mir HS, Yoon RS, Koval KJ. Autograft, allograft, and bone graft substitutes: Clinical evidence and indications for use in the setting of orthopaedic trauma surgery. J Orthop Trauma 2019;33:203-13. [Google Scholar | PubMed]
- 16.Thiery A, Tapos O, Anagnostakos K. Giant solitary cyst at the site of knee osteoarthritis: Treatment with a synthetic resorbable bone graft substitute and Primary total knee arthroplasty. Case Rep Orthop 2018;2018:1693131. [Google Scholar | PubMed]
- 17.Ohishi T, Takahashi M, Suzuki D, Matsuyama Y. Giant intraosseous cyst in an osteoarthritic knee. Orthopedics 2016;39:e1193-6. [Google Scholar | PubMed]
- 18.Rajani AM, Kumar R, Shyam A. Huge subchondral cyst communicating with medulary canal of femur in OA knee-treated by extension stem and bone grafting. J Orthop Case Rep 2014;4:81-4. [Google Scholar | PubMed]
- 19.Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: A systematic review. EFORT Open Rev 2019;4:611-7. [Google Scholar | PubMed]
- 20.McCormick BP, Rigor P, Trent SM, Lee JW, Tefera E, Mistretta KL, et al. Short-term outcomes following cemented versus cementless robotic-assisted total knee arthroplasty. Cureus 2022;14:e30667. [Google Scholar | PubMed]
- 21.Ashraf M, Sharma OP, Priyavadhana S, Sambandam SN, Mounasamy V. Rationale of cruciate retaining design in rheumatoid arthritis: A review of clinical analysis and its role in rheumatoid arthritis. Open Orthop J 2017;11:1023-7. [Google Scholar | PubMed]
- 22.Evaniew N, Tan V, Parasu N, Jurriaans E, Finlay K, Deheshi B, et al. Use of a calcium sulfate-calcium phosphate synthetic bone graft composite in the surgical management of primary bone tumors. Orthopedics 2013;36:e216-22. [Google Scholar | PubMed]
- 23.Damron TA, Lisle J, Craig T, Wade M, Silbert W, Cohen H. Ultraporous β-tricalcium phosphate alone or combined with bone marrow aspirate for benign cavitary lesions: Comparison in a prospective randomized clinical trial. J Bone Joint Surg Am 2013;95:158-66. [Google Scholar | PubMed]
- 24.Nunziato C, Williams J, Williams R. Synthetic bone graft substitute for treatment of unicameral bone cysts. J Pediatr Orthop 2021;41:e60-6. [Google Scholar | PubMed]