Be careful of brachial plexus paralysis when performing median sternotomy on small patients
Dr. Ryunosuke Fukushi, Department of Orthopaedic Surgery, Sapporo Medical University School of Medicine S1 W16, Sapporo, Hokkaido, 060-8543, Japan. E-mail: ryunosuke_fukushi_521@yahoo.co.jp
Introduction: Thoracotomy through a median sternotomy is considered a risk factor for brachial plexus paralysis. We report a new case of poor prognosis despite lower radiculopathy.
Case Report: A 53-year-old female (height 152 cm and weight 41 kg) complained of motor impairment in her left fingers, numbness in her left forearm, and paresthesia after left thoracotomy. A descending thoracic aortic replacement (20 mg J-graft 1 branch) had been performed through a left thoracotomy. After the surgery, she noticed movement disorder, numbness, and paresthesia and was referred to an orthopedic surgeon. Vitamin B12 formulation was administered, and she was followed up. The patient recovered motor function 8 months postoperatively, but numbness in the median nerve region remained 18 months after thoracotomy.
Conclusion: Even if brachial plexus paralysis persists as lower radiculopathy, nerve compression is relatively more severe in petite patients, suggesting that the prognosis may be poor.
Keywords: Brachial plexus, paralysis, thoracotomy, lower radiculopathy.
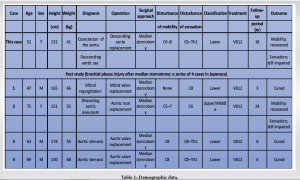
Thoracotomy through a median sternotomy is considered a risk factor for brachial plexus paralysis, and its global incidence has been reported as 0.5–38% [1]. No special treatment is required for this condition, and However, paralysis may persist in some cases. Ben-David and Stahl classified brachial plexus paralysis after thoracotomy through a median sternotomy into two types: The frequently occurring lower radiculopathy, which is characterized by a predominantly sensory impairment and a relatively good prognosis, and the less frequent upper/middle radiculopathy, which is characterized by a predominant movement disorder and a comparatively poor prognosis [2]. We previously reported four cases in which brachial plexus paralysis occurred after thoracotomy by median sternotomy. This included three cases of lower radiculopathy and one case of upper/middle radiculopathy. We also reported that the patients with lower radiculopathy had a good prognosis, whereas the one with upper/middle radiculopathy had a poor prognosis [3]. Herein, we report a new case of poor prognosis despite the presence of lower radiculopathy.
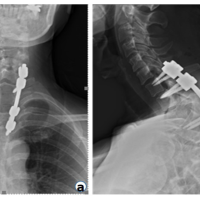
We report the case of a 53-year-old female (height 152 cm and weight 41 kg) who presented with a movement disorder in the left fingers, numbness in the left forearm, and paresthesia following thoracotomy through a median sternotomy. The patient was found to have an aneurysm at the same site as a coarctation of the aorta and underwent surgery. She was placed in a supine recumbent position with the upper limbs fixed to the side of the body. A descending thoracic aorta replacement (20 mg J-graft 1 branch) was performed through a left thoracotomy. The operation time was 194 min, and the extracorporeal circulation time was 58 min. After the surgery, she noticed a movement disorder in her left hand, numbness in her left forearm, and paresthesia and was referred to an orthopedic surgeon. During the physical examination, she was found to have numbness on the radial and dorsal sides of the palm of the left 1–4 fingers and paresthesia (decreased sensation) of the same fingers. Muscle strength measured using manual muscle testing revealed the following scores: Shoulder abduction/elbow flexion 5, elbow extension 5, wrist joint flexion 3, extension 4, finger extension 4, finger flexion 2, and opponens pollicis muscle 3. No Tinel’s sign was noted. A Vitamin B12 formulation was administered, and she was scheduled for follow-ups. She recovered motor function 8 months postoperatively, but numbness in the median nerve area persisted. At this time, carpal tunnel syndrome was suspected, and carpal tunnel surgery was performed; however, numbness in the median nerve region remained 18 months after thoracotomy (Table 1).
According to Graham et al., after performing a median sternotomy and opening the thoracic cavity using a retractor, the lateral movement of the split sternum stalk causes posterior movement of the clavicle and upward rotation of the first rib. As a result, the brachial plexus (which runs between the clavicle and the first rib) becomes compressed, resulting in paralysis [4] (Fig. 1).
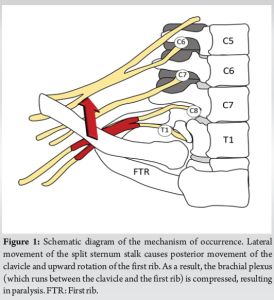
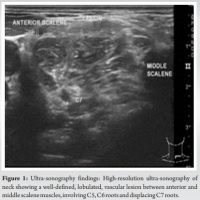
However, Ben-David and Stahl classified brachial plexus paralysis after thoracotomy through a median sternotomy into two types: Lower radiculopathy, which is characterized by a predominantly sensory impairment and a relatively good prognosis, and upper/middle radiculopathy, which is characterized predominantly by a movement disorder and has a comparatively poor prognosis. Lower radiculopathy is said to occur more frequently [2]. We previously reported four cases of brachial plexus paralysis after thoracotomy through a median sternotomy (three with lower radiculopathy and one with upper/middle radiculopathy) [3]. The case of upper/middle radiculopathy involved a 75-year-old petite woman (all three cases of lower radiculopathy involved men). Thoracotomy through a median sternotomy requires a fixed surgical field and, considering that the thoracotomy width relatively increases the lateral movement of the sternum in smaller patients, the movement of the sternum is thought to move the clavicle posteriorly and the first rib further upward. On this basis, we speculated that upper/middle radiculopathy would occur through a different mechanism to that reported by Graham et al. [4]. In addition, it has been reported that lower radiculopathy has a good prognosis, whereas upper/middle radiculopathy has a poor prognosis. One of the three patients with lower radiculopathy only had sensory impairment, and all patients showed improvement within 6 months. In contrast, in one patient with upper/middle radiculopathy, the movement disorder improved but sensory impairment persisted for more than 24 months postoperatively. The patient in this present report had a poor prognosis, despite having a lower radiculopathy. Similar to the patient in our previously reported case with upper/middle radiculopathy and poor prognosis, this case also involved a petite woman. It is presumed that the lateral movement of the sternum is relatively large in small patients. Thus, even if lower radiculopathy persists, the nerve compression is relatively more severe, suggesting that the prognosis may be worse than that of the usual lower radiculopathy. It is necessary to keep in mind that brachial plexus paralysis after thoracotomy by median sternotomy in petite women may have a poor prognosis, regardless of whether the patient has upper/middle or lower radiculopathy. The mystery of this disease is why there are upper/middle and lower types. Anatomically, it seems that if the upper/middle part is damaged, the lower part cannot be damaged. There seems to be a difference in the pathogenic mechanism. In a study by Healey et al., the risk factors for brachial plexus palsy after thoracotomy through a median sternotomy included extracorporeal dislocation, shoulder fixation (90° or more) during surgery, addition of internal thoracic artery bypass surgery, insertion of an internal cervical pulse catheter, presence or absence of a longer extracorporeal circulation time (over 240 min), first rib fracture, and potential peripheral neuropathy [5-7]. In addition, there have been a number of reports in the past that have reported “women” as a risk factor, but they do not mention the mechanism [810]. There are various reports of similar cases where it was difficult to identify the particular cause; in the future, it will be necessary to accumulate more cases and verify them along with cadaveric specimens.
We report a case of lower radiculopathy with brachial plexus paralysis after thoracotomy through a median sternotomy. Even if brachial plexus paralysis persists as lower radiculopathy, nerve compression is relatively more severe in petite patients, suggesting that the prognosis may be poor.
If brachial plexus paralysis occurs in a small patient undergoing median sternotomy, even if it is a lower radiculopathy, it will be more severe. Because there is a possibility of a poor prognosis, more care must be taken in small patients.
References
- 1.Ünlü Y, Velioğlu Y, Koçak H, Becit N, Ceviz M. Brachial plexus injury following median sternotomy. Interact Cardiovasc Thorac Surg 2007;6:235-7. [Google Scholar | PubMed]
- 2.Ben-David B, Stahl S. Prognosis of intraoperative brachial plexus injury; a review of 22 cases. Br J Anaesth 1997;79:440-5. [Google Scholar | PubMed]
- 3.Ryunosuke F, Kohei Kanaya Kousuke iba,Toshihiko Yamashita et al. Brachial plexus injury after median sternotomy: A series of 4 cases in Japanese (2185-4092). J. Jpn. Soc. Surg. Hand. 2017;33:886-8. [Google Scholar | PubMed]
- 4.Graham JG, Pye IF, McQueen IN. Brachial plexus injury after median sternotomy. J Neurol Neurosurg Psychiatry 1981;44:621-5. [Google Scholar | PubMed]
- 5.Healey S, O’Neill B, Bilal H, Waterworth P. Does retraction of the sternum during median sternotomy result in brachial plexus injuries? Interact Cardiovasc Thorac Surg 2013;317:151-7. [Google Scholar | PubMed]
- 6.Sylvestre DL, Sandson TA, Nachmanoff DB. Transient brachial plexopathy as a complication of internal jugular vein cannulation. Neurology 1991;41:760-0. [Google Scholar | PubMed]
- 7.Trentman TL, Rome JD, Messick JM Jr. Brachial plexus neuropathy following attempt at subclavian vein catheterization. Case report. Reg Anesth 1996;21:163-5. [Google Scholar | PubMed]
- 8.Gil Y, Yun MJ, Kim JE, Lee MA, Kim DH. Brachial plexus injury following median sternotomy. Korean J Anesthesiol 2012;63:286-7. [Google Scholar | PubMed]
- 9.Seyfer AE, Grammer NY, Bogumill GP, Provost JM, Chandry U. Upper extremity neuropathies after cardiac surgery. J Hand Surg 1985;10A:16-9. [Google Scholar | PubMed]
- 10.Honet JC, Raikes JA, Kantrowitz A, Pursel SE, Rubenfire M. Neuropathy in the upper extremity after open-heart surgery. Arch Phys Med Rehabil 1976;57:264-7. [Google Scholar | PubMed]