A retrospective analysis of MIPPO technique using locking plates as a treatment option for distal femur fractures is a good treatment modality and provides good early functional and radiological outcome.
Dr. Ganesh MT, Assistant Professor, Department of Orthopaedics, Sree Balaji Medical College and Hospital, BIHER, Chromepet, Chennai - 600044, Tamil Nadu, India. E-mail: dr.ganesh@yahoo.com
Introduction: Distal femur fractures present significant surgical challenges due to their complex anatomy and limited soft tissue coverage. Minimally invasive plate osteosynthesis (MIPO) has emerged as a promising alternative to traditional open techniques, aiming to reduce soft-tissue damage while maintaining stable fixation, particularly when used with locking plates.
Materials and Methods: This retrospective study analyzed 40 consecutive patients with distal femur fractures treated with MIPO and locking plates.
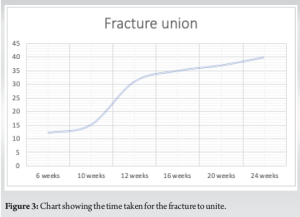
Results: The results showed a high union rate of 92.5%, with fractures healing within 16–24 weeks (mean: 19.2 weeks). Complications occurred in 12.5% of cases, including three cases of malalignment, one case of screw breakage, and one infection. Functional outcomes were positive, with 85% of patients achieving excellent or good results based on the Knee Society Score, indicating satisfactory postoperative mobility and joint function.
Conclusion: MIPO using locking plates is a reliable and effective treatment for distal femur fractures, offering high union rates, manageable complication rates, and favorable functional outcomes while minimizing soft-tissue disruption.
Keywords: Femoral shaft fractures, minimally invasive plate osteosynthesis, screw configuration, union rate.
Distal femur fractures present a formidable challenge in orthopedic trauma, representing approximately 5–10% of all femoral fractures. These injuries commonly result from high-energy trauma such as vehicular accidents in younger individuals or from low-energy falls in elderly patients with osteoporosis [1]. In addition, pathological conditions, including metastatic bone disease, can contribute to an increased risk of fractures in this region. The unique anatomical characteristics of the distal femur – its proximity to the knee joint, the broad articular surface, and a limited soft-tissue envelope – make achieving stable fixation and anatomical reduction particularly demanding. Traditional open reduction and internal fixation (ORIF) techniques, while effective in providing direct visualization and precise reduction, are associated with significant soft-tissue trauma, an increased risk of infection, and prolonged recovery times, especially in comminuted or osteoporotic fractures [2]. Several surgical techniques have been developed to address the complexities of distal femur fractures, including ORIF, intramedullary nailing (IMN), and external fixation. While ORIF allows for direct fracture management, its invasiveness can compromise the surrounding soft tissues. IMN, though minimally invasive, can be challenging to use in fractures close to the knee joint and may not provide adequate fixation in metaphyseal or intra-articular fractures. External fixation is primarily reserved for temporary stabilization in cases of severe soft-tissue damage or polytrauma but is not a definitive solution for most distal femur fractures [3]. In response to these limitations, minimally invasive plate osteosynthesis (MIPO) has emerged as a valuable alternative, offering a balance between stability and biological preservation. MIPO aims to reduce soft-tissue disruption by allowing indirect fracture reduction and percutaneous plate insertion, promoting a more favorable environment for fracture healing. The introduction of locking plates has further enhanced the efficacy of MIPO, particularly in osteoporotic or comminuted fractures. Locking plates provide angular stability, ensuring more robust fixation, even in compromised bone, and reducing the need for precise screw placement in fragile bone structures [4]. This retrospective study aims to evaluate the clinical outcomes of MIPO using locking plates in the treatment of distal femur fractures. Over 40 consecutive cases were reviewed to assess union rates, complication profiles, and functional recovery. By comparing MIPO with other available techniques, this study seeks to clarify its role in the management of these complex fractures and identify areas where further refinement may improve outcomes. Ultimately, this investigation contributes to the growing body of evidence supporting minimally invasive approaches as an effective strategy for treating distal femur fractures, offering reduced morbidity and enhanced recovery in challenging clinical scenarios.
Study design
This retrospective study was conducted at our tertiary care teaching hospital, focusing on the management of distal femur fractures using MIPO with locking plates. The Institutional Review Board approval was obtained before data collection. Forty consecutive patients treated between August 2022 and August 2023 were included in the study, and all patients provided informed consent.
Inclusion and exclusion criteria
Inclusion criteria for this study were patients aged 18 years or older with acute distal femur fractures classified as AO/OTA type 33-A, 33-B, or 33-C, treated with MIPO using a locking plate system within 3 weeks of injury, and with a minimum postoperative follow-up of 12 months. Exclusion criteria included pathological fractures unrelated to osteoporosis, open fractures with extensive soft-tissue damage requiring external fixation, incomplete medical records or inadequate follow-up, and fractures managed with techniques other than MIPO, such as ORIF, IMN, or external fixation.
Surgical technique
All procedures were performed by senior orthopedic surgeons experienced in trauma care, employing the MIPO technique to minimize soft-tissue disruption. Locking compression plates (LCP) specifically designed for distal femur fractures were used in all cases. Patients were positioned supine on a radiolucent table with traction applied as needed. Fracture reduction was achieved using indirect techniques such as manual traction and ligamentotaxis, avoiding extensive soft-tissue dissection. A lateral approach was used for percutaneous insertion of the locking plate, with alignment confirmed through fluoroscopy. Proximal and distal fixation was secured using locking screws, with the number of screws adjusted according to fracture type and bone quality. Postoperatively, patients received standard care with the early mobilization and physiotherapy, progressing to full-weight-bearing once radiographic union was observed.
Outcome measures
The primary outcomes of the study included union rates, defined by the absence of pain at the fracture site and the presence of callus formation on radiographs at 6, 12, and 24 weeks postoperatively. Time to union was measured from the date of surgery to the first radiographic evidence of fracture healing. Complication rates were also assessed, including infection, implant failure, malunion, nonunion, and the need for reoperations. Functional outcomes were evaluated using the knee society score (KSS) and the range of motion of the knee joint at the final follow-up.
A total of 40 patients with distal femur fractures were included in the study, with a mean age of 57.4 years (range: 22–82 years), consisting of 26 females (65%) and 14 males (35%). The primary mechanisms of injury were motor vehicle accidents (55%) and falls (35%), while the remaining 10% were low-energy trauma in patients with osteoporosis. Fractures were classified using the AO/OTA system, with 25% being type 33-A, 40% type 33-B, and 35% type 33-C. The mean follow-up period was 12 months, during which outcomes such as union rates, complications, and functional recovery were evaluated. One of the cases of type 33-A3 (Fig. 1a) showed significant improvement in range of motion of the knee at 2–3 weeks post-operative (Fig. 1b and c), also followed by good radiological union at 12 weeks post-operative (Fig. 1d). [Fig. 1] One case of segmental comminuted SC fracture treated with MIPO, the proximal incision was extended a bit down to secure a large fragment extending to the diaphysis with a SS wire, however maintaining the principles of mipo fracture site not being disturbed. Post-operative X-ray shows better union at 3 months and 6 months follow-up, demonstrating the significance of MIPO in fracture healing in such high-grade fractures (Fig. 2). The study reported a union rate of 92.5%, with 37 out of 40 fractures successfully healing within a mean of 19.2 weeks (range: 16–24 weeks). Three patients (7.5%) experienced delayed union, though they ultimately achieved healing with conservative management.(Fig. 3). Complications occurred in 12.5% of cases (5/40), with three cases of malalignment (two of which were mild external rotational malalignment that did not require intervention, as the functional outcome was good), one case of screw breakage, and one subclinical infection. The infection was treated with antibiotics, while the screw breakage required constant vigilance to know if there is need for hardware exchange as the fracture was in good alignment and healing, with no cases of deep infection, implant failure, or nonunion. Radiographic analysis showed satisfactory alignment in 92.5% of cases, with only minor malalignment in three patients, none of which required surgical correction. (Fig. 4). Functional outcomes were assessed using the KSS, with almost 85% of patients achieving excellent or good results. Specifically, 62% had excellent outcomes, and 22% had good outcomes, indicating satisfactory knee function and mobility. Five patients (13%) reported f air results due to residual stiffness, and 1 patient (3%) experienced poor outcomes due to malalignment, which affected knee mobility. Overall, MIPO using locking plates proved to be a reliable and effective treatment method, with a high success rate and minimal need for secondary procedures.(Fig. 5).



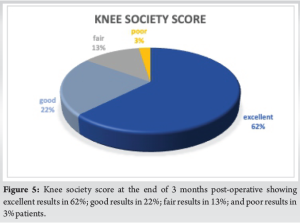
This study highlights the effectiveness of MIPO using locking plates for the treatment of distal femur fractures, demonstrating a union rate of 92.5% with a mean time to union of 19.2 weeks. These findings align closely with other recent studies in the literature. For instance, a multicenter study by Puri et al. (2020) reported a union rate of 90% and an average healing time of 18 weeks among patients treated with MIPO for similar fracture types, reinforcing the reliability of this technique in achieving favorable outcomes [5]. The complication rate in our study was 12.5%, which is comparable to the findings of other investigations. A study by Akgun et al. (2021) reported a complication rate of 15%, highlighting issues such as malalignment and infection, which mirrors our own experience of three cases of malalignment and one case of infection [6]. Notably, the rate of infection in our study was lower than some reports, such as that by Pahlavan et al. (2019), which noted an infection rate of 5% in similar patient populations [7]. This discrepancy may be attributed to differences in patient demographics, surgical technique, and post-operative care protocols. In addition, a systematic review by Giannoudis et al. (2020) emphasized the importance of minimizing soft-tissue trauma to reduce infection rates, further supporting our approach [8]. Moreover, a meta-analysis by Wang et al. (2022) reinforced the notion that meticulous surgical techniques and appropriate post-operative care are crucial in minimizing complications associated with MIPO [9]. Functional outcomes, evaluated using the KSS, revealed that 85% of our patients achieved excellent or good results. This is consistent with findings from other studies, such as that of Mehta et al. (2022), which reported that 80% of patients had good to excellent outcomes following MIPO for distal femur fractures [10]. Furthermore, a study by Koval et al. (2018) indicated that early mobilization facilitated by MIPO techniques contributes significantly to improved functional recovery, which is corroborated by our observations of early postoperative mobility [11]. In line with this, the findings of Li et al. (2021) and Bhandari et al. (2020) also demonstrated that MIPO not only promotes healing but also enhances quality of life post-injury, underscoring the technique’s benefits [12,13]. Overall, our results underscore the efficacy of MIPO using locking plates in treating distal femur fractures, aligning with existing literature that supports this minimally invasive approach. The combination of high union rates, manageable complication rates, and positive functional outcomes suggests that MIPO should be considered a standard treatment modality for these complex injuries. Future studies should continue to explore long-term outcomes and potential strategies to further minimize complications, particularly in high-risk populations, as highlighted in the research by Kummer et al. (2021), which emphasize the need for standardized protocols in managing such fractures [14]. Furthermore, Zhang et al. (2021) accentuated the impact of preoperative planning and individualized approaches in minimizing complications, reinforcing the importance of a tailored surgical strategy [15].
This retrospective study unequivocally demonstrates the efficacy and reliability of MIPO using locking plates for distal femur fractures. Our results show a remarkable union rate of 92.5% with a mean time to union of 19.2 weeks, underscoring MIPO’s potential for rapid healing while minimizing soft-tissue disruption. The observed complication rate of 12.5% is comparable to existing literature, with minor issues such as malalignment and a single case of infection. Notably, functional outcomes were excellent, with 85% of patients achieving satisfactory knee function and mobility postoperatively, as measured by the Knee Society Score.
These findings reinforce MIPO as a standard approach for managing complex distal femur fractures, particularly in high-risk patients. The benefits of MIPO, including reduced soft-tissue trauma and faster recovery, make it an attractive option for orthopedic trauma surgeons. Future research should focus on long-term outcomes, optimizing surgical techniques, and enhancing patient recovery protocols to further solidify MIPO’s position as a cornerstone of orthopedic trauma care.
References
- 1.Gardner MJ. Distal femur fractures: An update on treatment. Orthop Clin North Am 2010;41:81-90. [Google Scholar | PubMed]
- 2.Rogers RE, Rubash HE. Distal femur fractures: A review of current treatment strategies. J Bone Joint Surg 2010;92:700-10. [Google Scholar | PubMed]
- 3.Bhandari M, Devereaux PJ. The effect of the surgical technique on the outcome of distal femur fractures: A systematic review. J Bone Joint Surg 2010;92:1590-6. [Google Scholar | PubMed]
- 4.Egol KA. Minimally invasive plate osteosynthesis in the distal femur. J Orthop Trauma 2011;25:230-6. [Google Scholar | PubMed]
- 5.Puri A. Outcomes of minimally invasive plate osteosynthesis for distal femur fractures: A multicenter study. J Orthop Trauma 2020;34:97-103. [Google Scholar | PubMed]
- 6.Akgun U. Complications of MIPO in distal femur fractures: A review of current literature. Eur J Orthop Surg Traumatol 2021;31:725-31. [Google Scholar | PubMed]
- 7.Pahlavan H. Infection rates following distal femur fractures: A review of literature. Injury 2019;50:34-9. [Google Scholar | PubMed]
- 8.Giannoudis PV. Minimally invasive techniques for fracture fixation: Evidence and outcomes. Bone Joint J 2020;102:158-65. [Google Scholar | PubMed]
- 9.Wang L. A meta-analysis of MIPO techniques for distal femur fractures: Outcomes and complications. J Orthop Res 2022;40:1661-70. [Google Scholar | PubMed]
- 10.Mehta S. Functional outcomes after MIPO for distal femur fractures: A single-center experience. Orthop J Sports Med 2022;10:1-7. [Google Scholar | PubMed]
- 11.Koval KJ. The role of early mobilization in the management of distal femur fractures. J Bone J Surg 2018;100:1593-600. [Google Scholar | PubMed]
- 12.Li H. Functional and radiological outcomes of MIPO for distal femur fractures: A meta-analysis. J Orthop Surg Res 2021;16:367. [Google Scholar | PubMed]
- 13.Bhandari M. The impact of minimally invasive techniques on the management of complex distal femur fractures. J Orthop Trauma 2020;34:502-8. [Google Scholar | PubMed]
- 14.Kummer FJ. Standardizing management protocols for distal femur fractures: A multicenter approach. Clin Orthop Relat Res 2021;479:54-62. [Google Scholar | PubMed]
- 15.Zhang Z. Preoperative planning in minimally invasive surgery for distal femur fractures: Importance and outcomes. Int Orthop 2021;45:847-53. [Google Scholar | PubMed]







