Unilateral biportal endoscopic discectomy in the lateral position is a viable and advantageous minimally invasive option for treating spinal disc pathologies.
Dr. Sharafuddeen Mammu, Senior Resident Department of Orthopaedics, Government Medical College, Kozhikode, Kerala, India. E-mail: Sharafuddeen786@gmail.com
Introduction: Endoscopic spine surgery (ESS) is a minimally invasive technique that allows for direct visualization of spinal pathologies and has become a safe and effective alternative to traditional open spine surgery. Conventionally performed in the prone position, biportal endoscopy can also be done in the lateral position to avoid prone-associated complications. To our knowledge, the use of unilateral biportal endoscopy (UBE) in the lateral position has not been previously reported.
Case Report: We present the case of a 53-year-old male who experienced severe low back pain and right-sided radiculopathy due to a disc protrusion at the L4-L5 level. The patient was managed surgically using UBE in the lateral position once the conservative management was ineffective. This innovative approach aimed to minimize the complications associated with the prone position typically used in such procedures.
Conclusion: The successful management of L4–L5 intervertebral disc prolapse using UBE in the lateral position in this case demonstrates the potential of this technique as an effective and minimally invasive alternative to conventional surgical methods. This approach could offer a viable solution for treating degenerative spinal diseases while mitigating the steep learning curve associated with ESS. Further research and clinical studies are necessary to validate and optimize this technique.
Keywords: Biportal endoscopy, lateral position, disc prolapse, discectomy.
Endoscopic spine surgery (ESS) has revolutionized spinal procedures by offering a minimally invasive method that enables direct visualization of spinal pathologies. ESS has emerged as a reliable and efficient alternative to traditional open spine surgeries, with its applications extending from the lumbar to the cervical regions. The traditional treatments for lumbar disc herniation include open posterior lumbar interbody fusion [1], transforaminal lumbar interbody fusion [2], and posterior decompression [3]. The development of comprehensive endoscopic systems has made targeted decompression procedures possible through various surgical approaches, depending on the location of the spinal lesion and the surgeon’s expertise. The advancement in endoscopic technology and equipment has significantly bolstered the adoption of endoscopic treatments among spinal surgeons and patients alike. This preference stems from its distinct advantages, such as minimal iatrogenic trauma, reduced blood loss, shorter hospital stays, and favorable clinical outcomes. Discectomy and intervertebral fusion performed through a single portal represent advancements in minimally invasive spinal surgery, offering benefits such as reduced iatrogenic trauma, minimal bleeding, and accelerated recovery [4]. However, these procedures are characterized by a single-portal approach where both the visualization and instrument manipulation occur through the same frame, in a coaxial manner. Despite their advantages, this technique has drawbacks including challenges in achieving precise stereoscopic positioning, limited instrument maneuverability, and reduced surgical efficiency. In addition, the specialized instruments and equipment required for these procedures impose constraints on their broader adoption and further development in ESS. Hence, many spine surgeons have advocated for the use of biportal endoscopy with intraoperative irrigation for the treatment of lumbar disc herniation and lumbar spinal stenosis, citing successful outcomes achieved with this approach [5]. This surgical technique employs two key portals: the viewing portal and the working portal. The viewing portal accommodates the endoscope to provide a clear surgical field of vision, essential for precise visualization during the procedure. Through the working portal, surgeons utilize specialized tools such as the plasma radiofrequency wand, burr, chisel, and kerrison rongeur to perform intricate surgical tasks inside and around the spinal canal [6]. By leveraging two-port technology, this approach enables surgeons to conduct multidirectional surgeries, overcoming the limitations of traditional coaxial endoscopic techniques such as restricted field of view and maneuverability. Biportal endoscopic techniques have been developed to simplify procedures traditionally performed with patients in the prone position. Exploring the lateral position for biportal endoscopy may offer additional advantages by potentially reducing complications associated with prone positioning. This case report highlights the successful application of unilateral biportal endoscopy (UBE) in the lateral position for treating a patient suffering from severe radicular symptoms due to a disc protrusion at the L4–L5 level.
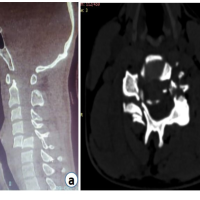
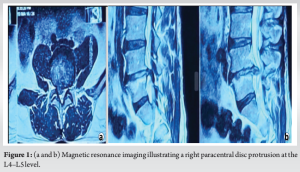
A 44-year-old male presented with severe low back pain radiating to the right lower limb, accompanied by numbness in the foot and toes. The pain, rated 8/10 on the Visual Analog Scale (VAS), had persisted for 6 months, significantly impairing his quality of life, as indicated by an Oswestry Disability Index score of 70%. His symptoms worsened with bending forward and performing daily activities, with notable aggravation over the past month. Physical examination revealed Right Extensor Hallucis Longus weakness with intact deep tendon reflexes. Pre-operative X-rays showed no instability, while magnetic resonance imaging revealed a right paracentral disc protrusion at the L4–L5 level (Fig. 1a and b).
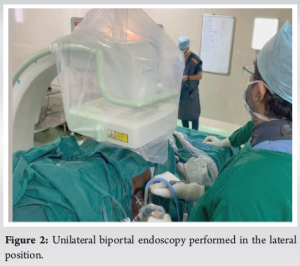
To alleviate his symptoms, we performed a unilateral biportal endoscopic discectomy (UBE) in the lateral position for L4–L5 protruded disc (Fig. 2). The procedure lasted approximately 45 minutes with minimal blood loss of around 40 ml. The post-operative period was uneventful. The patient was able to start full weight-bearing the next day and was discharged on the second day.
Follow-up was conducted after 1 week and then after 1 month followed by a visit after 6 months. The patient’s pain and tingling sensations in the legs improved significantly by the 1st-week follow-up, with a VAS score of 0/10. At the 1-year follow-up, completely recovered with full return to his daily routine activities, indicating a substantial recovery. Patient satisfaction, assessed using Macnab’s criteria at the final follow-up visit, was excellent. The patient was able to resume his routine activities without the need for medication, demonstrating the effectiveness and positive outcome of the procedure.
Technical Note and Surgical Approach
Under general anesthesia, the patient is placed in the left lateral position for a right-sided disc pathology (Fig. 3). Positioning in the right lateral position for right-sided pathology can negatively affect water dynamics and orientation, making it challenging to direct the scope upward. Two bolsters support the patient, and the hip is flexed just short of 90° to bring the spine into a flexed posture, widening the interlaminar area and reducing the amount of bone removal required. Flexing the hip beyond 90° can hinder C-arm imaging. Adequate padding of bony prominences is essential to avoid inadvertent neurovascular issues.

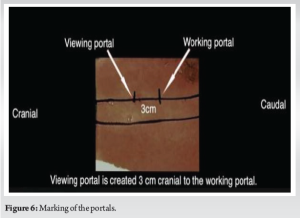
Once the patient is positioned and necessary trial imaging is done, the patient is draped and prepared for the procedure. The lateral position allows the surgeon the flexibility to either stand or sit during the surgery. Under C-arm guidance, midline and medial pedicular lines are marked (Fig. 4). Using a 30° scope, the working portal is made in line with the superior endplate of the lower vertebra (Fig. 5), and the viewing portal is placed 3 cm cranial to the working portal (Fig. 6). Once the portals are created, the working space is established at the spinolaminar junction with the aid of a blunt periosteum, shaver, and radiofrequency ablation (Fig. 7).

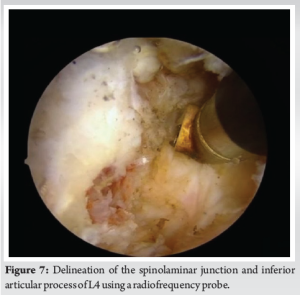
After triangulating and reaching the spinolaminar junction, the rest of the procedure, including flavectomy and discectomy, is performed similarly to when the patient is in the prone position. The procedure involves careful dissection and removal of the disc material to decompress the affected nerve root. Throughout the process, continuous irrigation is used to maintain clear visualization and to minimize thermal injury from the radiofrequency ablation. The wound is then closed with surgical staples.
The biportal endoscopic technique represents a significant advancement in the field of minimally invasive spine surgery, particularly for the treatment of lumbar disc herniation and spinal stenosis. By utilizing separate viewing and working portals, this approach enhances surgical precision and flexibility compared to traditional single-portal methods. UBE offers distinct advantages over microscopic decompression for treating lumbar canal stenosis. It allows surgeons to swiftly access deep anatomical sites and provides a well-illuminated surgical field with optimal magnification [7-9]. In addition, the technique minimizes unnecessary invasion of surrounding tissues and preserves the facet joint. This preservation offers significant benefits for patients, including reduced post-operative back pain and a quicker return to normal activities [7]. In this case, we had a male patient with symptomatic L5–S1 disc herniation managed with UBE. Conventionally, UBE is performed with the patient placed prone with the abdomen free over a radiolucent frame. However, this position presents several issues due to increased pressure on anterior structures, which can lead to complications such as pressure sores, postoperative visual loss from inappropriate orbital pressure, lateral femoral cutaneous neuropathy, and ischemic optic neuropathy [10]. Cardiac arrest during spine surgery in the prone position is particularly challenging to manage due to poor access, making cardiopulmonary resuscitation and defibrillation difficult. Advanced age is a significant risk factor for cardiac arrest, necessitating a thorough evaluation of cardiac risk factors preoperatively [11]. In our case, the UBE procedure was performed with the patient in the lateral position. This position offers unique advantages, such as ensuring free abdominal movement and eliminating the need to turn the patient, thereby reducing manpower requirements. The lateral position provides easier positioning, less intra-abdominal pressure, and thus lesser bleeding. It is also hemodynamically better, maintaining constant access to the airway, which is crucial for promptly addressing any tube issues. In addition, the lateral position widens the interlaminar space as the spine is less extended, requiring less bony work. The lateral positioning is particularly useful for spinal surgeries during pregnancy. One of the most significant advantages of the lateral position is the potential reduction in intraoperative and post-operative complications. The reduction in intra-abdominal pressure translates to decreased blood loss, which is a critical factor in maintaining hemodynamic stability, particularly in high-risk patients. Furthermore, the enhanced access to the airway allows for continuous monitoring and quick intervention in the event of anesthesia-related complications, thus improving overall patient safety. From a surgical perspective, the lateral position offers improved ergonomics for the surgeon. The natural alignment of the patient’s anatomy in this position allows for better maneuverability of instruments and more precise targeting of the surgical site. This can lead to more efficient procedures and potentially shorter operation times, reducing the overall burden on the healthcare system and improving patient throughput. Despite these advantages, it is essential to recognize the challenges associated with this technique. Surgeons must undergo specific training to adapt to the lateral position’s unique requirements, and there is a learning curve for those not accustomed to this approach. In addition, careful attention must be paid to avoid compression or stretching of neurovascular structures, which can lead to complications.
UBE in the lateral position demonstrates significant potential as a minimally invasive technique for spinal surgery. Its benefits in terms of surgical precision, reduced tissue invasion, and improved patient outcomes are promising. As the experience with this technique grows and more evidence accumulates, UBE in the lateral position could become a standard practice, offering substantial benefits to patients and surgeons alike. The ability to minimize complications, reduce operative time, and enhance recovery positions this approach as a forward-looking solution in the evolving landscape of spinal surgery. Further research and larger, randomized studies are warranted to fully establish the long-term benefits and safety profile of this innovative technique.
Unilateral biportal endoscopic discectomy in the lateral position is an effective and minimally invasive technique for treating spinal disc pathologies. This approach offers significant advantages, including precise surgical intervention, minimal tissue disruption, reduced operative time, and accelerated recovery. As experience with this technique grows, it holds the potential to become a standard practice in spinal surgery, providing substantial benefits for both patients and surgeons. This method minimizes complications and improves patient outcomes, making it a promising advancement in the field of spinal surgery.
References
- 1.Allen CR, Kaplan LD, Fluhme DJ, Harner CD. Posterior cruciate ligament injuries. Curr Opin Rheumatol 2002;14:142-9. [Google Scholar | PubMed]
- 2.Sonin AH, Fitzgerald SW, Hoff FL, Friedman H, Bresler ME. MR imaging of the posterior cruciate ligament: Normal, abnormal, and associated injury patterns. Radiographics 1995;15:551-61. [Google Scholar | PubMed]
- 3.Hooper PO 3rd, Silko C, Malcolm TL, Farrow LD. Management of posterior cruciate ligament tibial avulsion injuries: A systematic review. Am J Sports Med 2018;46:734-42. [Google Scholar | PubMed]
- 4.Sun HQ, Ren YJ, Zhang YQ. Treatment of posterior cruciate ligament avulsion fracture with pressurized staples. Chi J Orthop Trauma 2011;13:1189-90. [Google Scholar | PubMed]
- 5.Fu YP, Hang CM, Fam HQ. Treatment of posterior cruciate ligament avulsion fracture using anchor system combined with cannulated screw. J Pract Orthop 2011;17:73-4. [Google Scholar | PubMed]
- 6.Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res 1990;254:216-9. [Google Scholar | PubMed]
- 7.Jung YB, Tae SK, Lee YS, Jung HJ, Nam CH, Park SJ. Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc 2008;16:729-33. [Google Scholar | PubMed]
- 8.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1978;52:1677-84. [Google Scholar | PubMed]
- 9.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982;10:150-4. [Google Scholar | PubMed]
- 10.Zhao JZ, He YH, Wang JH. Treatment of acute posterior cruciate ligament avulsion fracture via arthroscopically assisted double posteromedial approach. Chi J Orthop 2005;25:16-20. [Google Scholar | PubMed]
- 11.Lu HX, Huangpu XQ, Zhang J. Treatment of acute posterior cruciate ligament avulsion fracture with arthroscopically assisted cannulated screw fixation. J Pract Orthop 2012;18:797-9. [Google Scholar | PubMed]
- 12.Horas U, Meissner SA, Heiss C, Schnettler R. Arthroscopic fixation of posterior cruciate ligament avulsion fractures: A new minimally invasive technique. Knee Surg Sports Traumatol Arthrosc 2010;18:781-3. [Google Scholar | PubMed]
- 13.Chen W, Tang D, Kang L, Ding Z, Sha M, Hong J. Effects of microendoscopy-assisted reduction and screw fixation through a single mini-incision on posterior cruciate ligament tibial avulsion fracture. Arch Orthop Trauma Surg 2012;132:429-35. [Google Scholar | PubMed]
- 14.Sasaki SU, Da Mota e Albuquerque RF, Amatuzzi MM, Pereira CA. Open screw fixation versus arthroscopic suture fixation of tibial posterior cruciate ligament avulsion injuries: A mechanical comparison. Arthroscopy 2007;23:1226-30. [Google Scholar | PubMed]