ACL injury can result in damage and loss of proprioceptive receptors, leading to mechanical instability. The significant differences in proprioceptive outcomes observed in the current study suggest that remnant preservation may enhance early sensory feedback post-ACLR.
Dr. Sushanth Sudhir Rao, Department of Orthopedics, Yenepoya Medical College, Mangalore, Karnataka, India. E-mail: sushwa6@gmail.com
Introduction: Anterior cruciate ligament reconstruction (ACLR) is a commonly performed procedure for patients experiencing persistent symptomatic instability, aimed at achieving a functionally stable knee while minimizing the risk of secondary injuries and long-term complications. An anterior cruciate ligament (ACL) injury can result in damage and loss of proprioceptive receptors, leading to mechanical instability. As a result, current research is exploring innovative strategies to improve ACL healing, lower the failure rate, expedite recovery, and restore the biomechanics of the knee to pre-injury levels.
Objectives: This study aimed to study the functional outcomes and post-operative proprioceptive function in patients who undergo remnant-preserving ACLR (RP-ACLR) compared to the standard ACLR (S-ACLR) technique.
Materials and Methods: This prospective study was conducted among patients who presented with ACL injury, and who underwent either arthroscopic remnant RP-ACLR or arthroscopic S-ACLR. Patient’s functional outcome was measured by International Knee Documentation Committee (IKDC) subjective knee score, Lysholm knee score, Visual Analog Scale score, and proprioception by joint position error (JPE) in degrees was noted at presentation, at 15 days, 30 days, 3 and 6 months postoperatively.
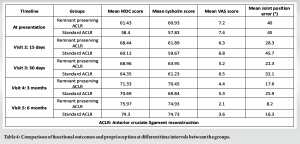
Results: A total of 30 cases of with ACL injury during the study period who underwent RP-ACLR and 30 cases of ACL injury who underwent S-ACLR. There were 83.3% males and 16.7% females in RP-ACLR group and 86.7% males and 13.3% females S-ACLR group with patients being maximally at the age group of 26–30 years (41.7%). The average time since injury of 4.04 months and average surgical time was 90 min. There was progressive improvement in functional outcome at 15 days, 30 days, 3 months, and 6 months (P = 0.01). At 6 months, the IKDC and Lysholm scores were 75.97 and 74.93 in the RP-ACLR group, 74.30 and 74.73 in S-ACLR group, respectively. There was a statistically significant enhancement in proprioception, measured by JPE in degrees between the groups as assessed at 15° flexion (P = 0.02), 45° flexion (P = 0.01), and 60° flexion (P = 0.01).
Conclusion: Our results indicated no significant difference in functional outcomes between the two groups as assessed by the IKDC and Lysholm Knee scores, although both groups demonstrated significant improvements postoperatively. In conclusion, the significant differences in proprioceptive outcomes observed in the current study suggest that remnant preservation may enhance early sensory feedback post-ACLR.
Keywords: Anterior cruciate ligament injuries, arthroscopy, anterior cruciate ligament reconstruction.
Anterior cruciate ligament (ACL) injuries are a prevalent among athletes and rank as one of the most frequently treated knee conditions [1]. ACL reconstruction (ACLR) is the sixth most commonly performed procedure in orthopedics and has become a widely used and effective treatment for knees with ACL deficiencies [2]. ACLR is a commonly performed surgery for patients experiencing persistent symptomatic instability, aimed at providing a functionally stable knee while reducing the risk of secondary injuries and long-term complications. It is noted that 83% of the athletes return to their pre-injury level post-procedure [3]. The estimated number of ACLRs performed annually in the United States varies significantly, ranging from 60,000 to 175,000 procedures [4,5]. Whereas, in India, the epidemiology regarding ACLR is not systematically reported, however in advanced centers 20–100 procedures have been reported each year [6,7]. The primary objectives of ACLR are to stabilize the knee joint, restore normal movement mechanics, and prevent the early development of degenerative arthritis [8]. Proprioceptors of the knee joint are located at the tibial bone insertion area of the ACL [9]. Schultz et al. were the first to demonstrate the presence of mechanical receptors in the ACL of the human knee joint through histopathological examination, suggesting that the ACL may play a role in proprioception [10]. Consequently, an ACL injury can result in damage and loss of proprioceptive receptors, leading to reduced afferent information input and increased mechanical instability [11]. To mitigate the loss of proprioception, the technique of preserving the remaining ACL tissue during reconstruction has been suggested. Preserving the ACL remnant during reconstruction may also promote better integration of the implanted graft and enhance clinical function [12]. In addition, the ACL remnant contains stem cells that aid in tendon-bone healing following ACLR [13]. Current research is exploring innovative strategies to improve ACL healing, lower the failure rate, speed up recovery, and restore the biomechanics of the knee to pre-injury levels. Numerous studies have indicated that preserving the ACL remnant aids in stabilizing the knee, promotes tissue healing, and may reduce the risk of graft rupture post-surgery [14,15]. Research comparing the effects of remnant-preserving ACLR (RP-ACLR) on proprioception with those of standard ACLR (S-ACLR) techniques, as well as its relationship to functional stability, has been limited. Therefore, it is necessary to evaluate the outcome in terms of proprioception and functional recovery post-arthroscopic ACLR by remnant preservation in comparison with S-ACLR technique. This study aimed to study the functional outcomes and post-operative proprioceptive function in patients who undergo RP-ACLR versus S-ACLR technique.
Study protocol
This prospective comparative study was conducted in Yenepoya group of Institutions, Yenepoya Medical College Hospital and Yenepoya Superspeciality Hospital, Karnataka, India from January 2024 to October 2024 after obtaining the ethical clearance from the Yenepoya Ethics Committee-2 (YEC2/2024/086).
Sample size estimation
where,
n = Required sample size
Zα/2 = Standard normal distribution for a 95% confidence interval (1.96)
Z(1-β) = Power (0.84)
P1 = proportion with the outcome in the first group (18.2)
P2 = proportion with the outcome in the second group (17.8)
Sample size calculated is 25. Considering dropout rates and lost to follow-up rates (20%), 30 cases were selected for RP-ACLR with and 30 for S-ACLR. After informed, written consent, all the patients above the age of 18 years were assigned to the groups based on intraoperative findings and inclusion criteria. Patients with complete ACL injury, with tibial insertion of the ACL remnant being intact, were included in the remnant-preserving ACL group. Patients above the age of 18 years, with complete ACL injury, were included in the standard ACL group. Patients with concurrent posterior cruciate ligament injury, posterior lateral corner injury, or medial collateral ligament injury, with prior neurological disorders, and patients with osteochondral fractures and articular cartilage defects were excluded from the study. Patients who were admitted under the Department of Orthopedics, Yenepoya Medical College, with a history of trauma, instability to the knee joint were examined, demographic information, mode of injury, pain, and disability were measured by Visual Analog Scale (VAS). Symptoms related to ACL tear such as knee instability, pain, and a decrease in joint function were noted. At the presentation, patient’s functional outcome was measured by International Knee Documentation Committee (IKDC) subjective knee score (IKDC), Lysholm knee score, VAS score, and proprioception by joint position error (JPE) in degrees was noted. Intraoperatively, patients who meet inclusion criteria underwent arthroscopic RP-ACLR surgery and rest of the patients underwent S-ACLR by a single orthopedic surgeon. The standard of care was not affected, delayed denied, or modified for the purpose of this study.
Outcome measures
Patients were followed up at 15 days, 30 days, 3 months, and 6 months postoperatively. At every follow-up, functional outcome was assessed by Lysholm knee scoring system, IKDC score, VAS score, and proprioception by JPE in degrees. Standardized anteroposterior and lateral radiographs were used to assess the tunnel position.
Surgical technique
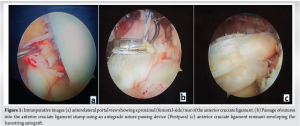
Under spinal anesthesia, the patient is positioned supine and a tourniquet is applied to proximal thigh. The surgical knee is painted and covered. The typical anteromedial (AM) which is the working portal and anterolateral (AL), which is the viewing portal, are established. During the diagnostic arthroscopy, the nature of the ACL tear is assessed, and a decision is taken to retain the ACL stump (Fig. 1a). The meniscal and articular cartilage are assessed, and either a meniscal repair or meniscectomy is carried out as needed. An autograft is taken from the ipsilateral hamstring. Standard ACL technique is carried out for patients meeting the inclusion criteria for the same. The “envelope” technique of RP-ACLR is described below.
Preparation of tunnels and remnant
While viewing through the AL portal, the anatomical starting point for the femoral tunnel is marked using an angled awl. The appropriate tunnel size (at least 8 mm in diameter and a minimum depth of 20 mm to fit the graft) is drilled independently from the AM portal. The knee is held in full flexion during femoral tunnel reaming. If graft impingement is expected, a bony notchplasty, especially on the medial wall of the lateral femoral condyle, may be performed. Next, a suture is passed into the ACL remnant using a flexible cannula and an antegrade self-retrieving suture passer (Fig. 1b). The suture material used is Number. 2 ultrahigh-molecular-weight polyethylene. The goal is to make crisscross suture passes in the ACL stump from distal to proximal, attempting a minimum of 4–5 passes. The sutures are then retrieved through the AM portal. With the knee at 90° of flexion and viewing from the AL portal, the tibial tunnel is drilled using a guide. The tunnel exits parallel to the posterior border of the anterior horn of the lateral meniscus, within the native ACL stump. To avoid damaging the stump and sutures, it is crucial to hand ream the inner cortex. Clearing both tunnels of soft tissue and bone debris is essential, as it facilitates smooth graft passage.
Graft passage and tensioning of remnant
A beath pin loaded with shuttle suture is passed through the AM portal into the femoral tunnel, exiting on the lateral side of the thigh. The free ends of the shuttle suture are clamped and secured. Using a suture grasper, all the sutures are pulled through the tibial tunnel in a single pass to avoid entangling the tissue. The sutures of the adjustable-loop button (Procinch) are then passed into the shuttle suture. The No. 2 ultrahigh-molecular-weight polyethylene sutures from the ACL remnant are threaded through the button from below and then into the shuttle suture, following the same direction as the button sutures. The adjustable-loop button is passed and flipped into position, which is confirmed by viewing through the AM portal for an end-on view of the tunnel. After confirming the button flip, the scope is switched back to the AL portal for further viewing. The graft is then pulled into the joint while the remnant sutures are tensioned. Once the graft is inserted to the appropriate depth (at least 20 mm), the remnant sutures are tensioned further. Tibial fixation is done using a bio-composite interference screw (Biosure Regenesorb) that is one size larger than the tibial tunnel diameter, after cycling the knee in 30° of flexion. The remnant sutures are tensioned and secured with 4 or 5 reversing half-hitches over the button using a knot pusher, ensuring the knot does not lock over the iliotibial band. At the conclusion of the procedure, the remnant appears to envelop the graft (Fig. 1c). Any additional or loose remnants are shaved off to prevent roof impingement or the formation of a cyclops lesion.
Statistical analysis
Statistical analysis was carried out using Statistical Packages for the Social Sciences version 29. A Chi-square test was applied for qualitative variables. Confidence interval was set at 95%. An independent sample t-test was applied to compare the statistical difference of quantitative variables between the groups. Paired sample t-test was applied to compare the statistical difference of quantitative variables (LYSHOM knee score, IKDC score) between pre-operative and post-operative 15 days, 30 days, 3 months, and 6 months intervals.
A total of 30 cases of with ACL injury during the study period who underwent arthroscopic RP-ACLR and 30 cases of ACL injury who underwent arthroscopic S-ACLR. In our study, 83.3% were males and 16.7% were females RP-ACLR group, and were 86.7% males and 13.3% were females S-ACLR group. Patients were maximally at the age group of 26–30 years (41.7%) and 20–25 years (38.3%) in both groups of the study. The mean age of patients in RP-ACLR group was 26.52 ± 3.87 years and in S-ACLR group was 27.07 ± 3.64 years. Sports was the most common mode of injury causing ACL tear in both groups followed by self-fall and road traffic accidents. In our study, the patients presented at an average time since injury of 4.04 months. Our study consisted of 14 patients in RP-ACLR group and 13 patients in S-ACLR group with medial meniscal injury. There were nine patients in RP-ACLR group and 12 patients in S-ACLR group with lateral meniscal injury. The average surgical time was found to be 90 min. In our study, there was a statistically significant improvement (P = 0.01) in the mean IKDC score, and mean Lysholm Knee score of the pre-operative and post-operative assessment within the groups. All the patients showed a progressive increase in their functional outcome 15 days, 30 days, 3 months, and 6 months (P = 0.02). The IKDC and Lysholm scores of all the patients were excellent at the end of 6 months with an average of 75.97 and 74.93 in the RP-ACLR group, and 74.30 and 74.73 in S-ACLR group, respectively. In our study, there was a statistically significant improvement in the proprioception by JPE in degrees between the groups as assessed at 15° flexion (P = 0.02), 45°flexion (P = 0.01), and 60° flexion (P = 0.01). All post-operative X-rays showed the graft to be in an anatomical position. In our study, two patients in RP-ACLR group and one patient in the S-ACLR group showed superficial infection. Eleven patients in RP-ACLR group and eight patients in the S-ACLR showed some degree of knee stiffness at 6 months follow-up (Fig. 2-4) (Table 1-4, ).
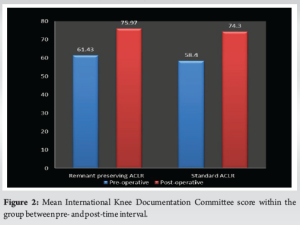
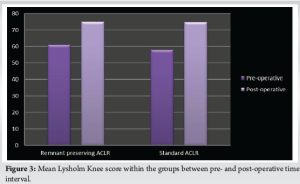
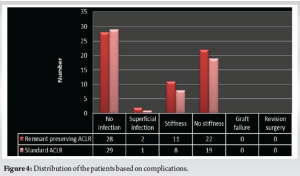

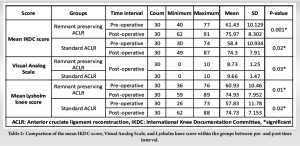
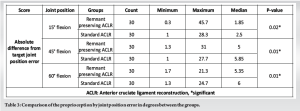
The aim of this study was to evaluate the functional outcomes and post-operative proprioceptive function in patients undergoing RP-ACLR compared to those receiving the S-ACLR technique. Patients were assessed for functional outcome by IKDC score, Lysholm knee score, VAS score, and proprioception by JPE in degrees at presentation, and postoperatively. Recent research has indicated that the remnant bundle plays a vital role in the biological healing of allograft tendons in ACL injury treatment, helps maintain proprioception, and exerts a biomechanical effect by inhibiting anterior translation of the knee joint. Consequently, efforts are being made to preserve the remnant bundle [16-20]. The study included 30 participants in RP-ACLR group and S-ACLR group, respectively. The majority of patients in both study groups were aged between 26 and 30 years (41.7%), with an average age of 24.2 years. There was male predominance of 83.3% in RP-ACLR group and 86.7% in S-ACLR group. Patients had maximally affected on the left side (65%) with an average time since injury of 4.04 months at presentation. Adachi et al. [21] conducted a comparison between ACL augmentation and reconstruction, revealing no significant differences in physical examination outcomes. The authors also noted that the ACL remnant bundle could contribute to the stability of the knee joint. Ochi et al. [22] implemented selective bundle reconstruction in approximately 10% of patients receiving ACLR. They suggested that remnant-preserving augmentation offers several advantages, including promoting the biological healing of the graft tendon, maintaining mechanoreceptors at the tibial insertion, mitigating anterior instability of the remnant bundle, and preventing tibial tunnel enlargement. A significant portion of patients in both groups had associated meniscal injuries, with the RP-ACLR group showing slightly more lateral meniscal injuries. Meniscal preservation or reconstruction during ACL surgery is critical for preventing future instability. Levy et al. [23] reported that the medial meniscus serves as a secondary restraint structure that prevents anterior translation of the tibia in the event of an ACL injury. They also noted that excising the medial meniscus led to a significantly greater increase in anterior displacement following medial meniscectomy (P < 0.05). In addition, Cho et al. [24] conducted a study examining the impact of meniscectomy on outcomes following ACLR. They found that anterior instability increased in cases where medial meniscectomy was performed, or when both medial and lateral meniscectomies were conducted together, compared to cases where only ACLR was performed. While these studies did not find significant differences in functional outcomes based on meniscal involvement, preserving the meniscus, particularly the medial meniscus, may play an essential role in long-term knee stability. The results of our study demonstrated no significant difference in post-operative functional outcomes between the RP-ACLR and S-ACLR groups at 6 months. The mean IKDC scores improved significantly within both groups postoperatively, but between-group differences were statistically insignificant (RP-ACLR: 75.97 vs. S-ACLR: 74.30, P = 0.42). This aligns with previous research by Ahn et al. [16] and Lee et al. [17], who also found that the amount of remnant preservation had limited influence on post-operative functional outcomes. These studies emphasize that ACL remnants may contribute to proprioception but do not necessarily enhance long-term functional results. The Lysholm Knee score was assessed between two groups at various follow-up periods. Both groups exhibited significant improvements within the pre- and post-operative intervals (P = 0.00), but the difference between the RP-ACLR (74.93) and S-ACLR (74.73) groups was minimal (P = 0.91). Ochi et al. [22] also reported that ACL augmentation procedures focusing on remnant preservation offer no clear advantage in functional scores. Lee et al. [17] found that among a group of 16 patients, those with a preserved remnant >20% of the ACL length exhibited better proprioceptive and functional outcomes compared to those with a remnant shorter than 20%. In this study, proprioception was assessed using JPE at three angles of knee flexion: 15°, 45°, and 60°. The RP-ACLR group demonstrated superior proprioceptive outcomes compared to the S-ACLR group across all angles. The median JPE at 15° flexion was considerably lower in the RP-ACLR group (1.85°) compared to the S-ACLR group (2.5°, P = 0.02), indicating better proprioceptive function early in the range of motion. This is consistent with findings from Adachi et al. [21] who observed that remnant-preserving techniques better maintained the mechanoreceptors responsible for proprioception, contributing to improved joint position sense postoperatively. At 45° and 60° flexion, the RP-ACLR group continued to show lower JPE (5.0° and 5.35°, respectively) compared to the S-ACLR group (5.85° and 6.0°, respectively), with the differences at both angles showing statistical significance (P = 0.01 and P = 0.00, respectively). These findings are consistent with studies by Ahn et al. [16] and Ochi et al. [22 ] who suggested that preserving the ACL remnant may help retain mechanoreceptors, thus contributing to enhanced proprioception during post-operative recovery. The proprioceptive benefits observed in this study align with the theory that the preserved remnant provides sensory feedback, improving joint stability and position sense. This could potentially result in a more natural gait pattern and reduced injury risk during rehabilitation. However, while the RP-ACLR group demonstrated statistically better proprioception, it remains uncertain whether these improvements translate into long-term functional benefits. Lee et al. [17] reported similar short-term gains in proprioception with remnant preservation but noted that these advantages diminished over time as proprioception naturally recovered in both groups. Further studies with extended follow-up periods are needed to assess whether the proprioceptive benefits of remnant-preserving techniques result in lasting clinical advantages. Moreover, Ahn et al. [25] demonstrated in their magnetic resonance imaging (MRI)-based study that the remnant bundle enhances graft remodeling, which in turn aids in proprioceptive recovery. This suggests that not only does remnant preservation help maintain proprioceptive fibers but it may also facilitate biological graft healing, contributing to superior proprioceptive outcomes. This enhanced proprioception could lead to a more natural restoration of joint mechanics and potentially reduce the risk of re-injury during the rehabilitation phase. In the study by Igdir et al. [26] 44 patients were prospectively assigned to two groups: 22 underwent RP-ACLR, and 22 underwent S-ACLR with remnant excision. The functional outcomes assessed by the IKDC and Lysholm knee scores showed no significant differences between the groups. The study showed that remnant-preserving anatomical single-bundle ACLR using a hamstring autograft can enhance proprioception and increase quadriceps femoris muscle strength. In a retrospective study by Liu et al. [27] 46 patients underwent ACLR with remnant preservation. The patients were divided into two groups based on the extent of remnant tissue preserved: Group A had more than one-third of the original ACL length preserved, while Group B had less than one-third preserved. At 3 months postoperatively, Group A demonstrated significantly better proprioception at all tested angles compared to Group B. In addition, activity levels, measured by the Tegner score, were higher in Group A at 12 months postoperatively and at the final follow-up. These findings suggest that preserving a greater portion of the ACL remnant may enhance early proprioceptive recovery and promote higher activity levels postoperatively. In addition, enhanced graft remodeling was verified through arthroscopic second-look evaluations [28,29]. Ahn et al. [25] performed second-look assessments on 62% of patients who underwent ACLR with remnant preservation, finding that 91% displayed adequate synovialization of the ACL graft. Kondo et al. [30] demonstrated in their second-look evaluations that the remnant-preserving technique was significantly more effective than the remnant-resecting procedure in terms of post-operative graft lacerations or tears, as well as synovial and fibrous tissue coverage of the grafts. Pain, assessed by the VAS, decreased significantly in both groups over the study period. However, the RP-ACLR group had a slightly lower pain score at 6 months (2.1) compared to the S-ACLR group (3.6). While the difference in pain levels was not statistically significant (P > 0.05), the trend toward lower pain in the remnant-preserving group suggests a potential advantage in early recovery, which could be related to reduced tissue trauma during surgery. Moreover, the faster reduction in pain levels observed in the RP-ACLR group may positively impact rehabilitation outcomes. Patients experiencing less pain during early recovery are likely to have better compliance with rehabilitation protocols, which is essential for restoring knee function and reducing long-term disability. A study by Kim et al. [31] examined pain outcomes using the VAS score in patients undergoing RP-ACLR versus S-ACLR (ACLR) at various intervals: Preoperatively, immediately postoperatively, and at follow-up visits at 3 and 6 months. Kim et al. [31] hypothesized that the preserved remnant tissue might help promote early biological healing and reduce the need for extensive graft manipulation during surgery, which could explain the lower post-operative pain in the RP-ACLR group. This is in line with the findings of our study, where the RP-ACLR group consistently showed lower VAS scores throughout the post-operative period, culminating in a significant difference at the 6-month mark (RP-ACLR: 2.1, S-ACLR: 3.6, P < 0.05). Regarding complications, the RP-ACLR group had a slightly higher incidence of superficial infections at 6.7%, compared to 3.3% in the S-ACLR group. However, the rates of knee stiffness were higher in the RP-ACLR group (36.7% vs. 26.7%). This could be due to the increased complexity of the remnant-preserving technique, which might limit early mobility. In a meta-analysis by Xie et al. [32] evaluated the impact of RP-ACLR compared to S-ACLR. The study found that RP-ACLR significantly improved patient functional scores. In addition, RP-ACLR was associated with less tibial tunnel enlargement. Importantly, there were no significant differences between the two groups regarding complications. While many studies suggest that remnant preservation may lead to better synovial coverage, this meta-analysis indicated insufficient evidence to support this claim, possibly due to variations in remnant preservation techniques. The potential risks associated with longer operation times in RP-ACLR are also worth considering.
Limitations
While these findings are promising, our study has certain limitations. The limited sample size and absence of long-term follow-up data constrain the generalizability of our findings. Larger, randomized controlled trials comparing remnant-preserving techniques to conventional ACLR methods are needed to validate these findings. In addition, future studies should include advanced imaging techniques like MRI or computed tomography scans to more accurately assess graft positioning and integration.
Our findings showed no significant difference in functional outcomes between the two groups based on IKDC and Lysholm Knee Scores, although both groups demonstrated significant improvements postoperatively. The significant differences in proprioceptive outcomes observed in the current study suggest that remnant preservation may enhance early sensory feedback post-ACLR. This could potentially facilitate quicker neuromuscular adaptations during rehabilitation, although the clinical relevance of these findings in long-term functional outcomes warrants further investigation. Overall, while RP-ACLR appears to offer short-term advantages in proprioception and pain relief, its long-term functional benefits remain comparable to those of S-ACLR. Future research with longer follow-up periods is needed to determine whether the early proprioceptive gains observed in remnant-preserving techniques translate into sustained functional improvements over time. In addition, patient-specific factors, such as activity level and meniscal involvement, should be considered when choosing the most appropriate surgical technique for ACLR.
The clinical message of this study is that RP-ACLR offers enhanced proprioceptive function in the early post-operative period compared to S-ACLR, with significant improvements in joint position sense. This suggests that remnant preservation may facilitate quicker neuromuscular adaptation during rehabilitation. However, further research with extended follow-up is necessary to determine whether these early proprioceptive advantages translate into sustained clinical benefits over time.
References
- 1.Bollen SR, Scott BW. Rupture of the anterior cruciate ligament--a quiet epidemic? Injury 1996;27:407-9. [Google Scholar | PubMed]
- 2.Prodromos C, Brown C, Fu FH, Georgoulis AD, Gobbi A, Howell SM, et al. The Anterior Cruciate Ligament: Reconstruction and Basic Science. Netherlands: Elsevier Health Sciences; 2007. [Google Scholar | PubMed]
- 3.Lai CC, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med 2018;52:128-38. [Google Scholar | PubMed]
- 4.Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 1997;79:1556-76. [Google Scholar | PubMed]
- 5.Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med 2008;359:2135-42. [Google Scholar | PubMed]
- 6.Prasad S, Anand Kumar BS, Gadiyar HB, Satyarup D. Does delay in ACL reconstruction increases incidence of associated injuries? Indian J Orthop Surg 2015;1:279-81. [Google Scholar | PubMed]
- 7.Devgan A, Singh A, Gogna P, Singla R, Magu NK, Mukhopadhyay R. Arthroscopic anatomical double bundle anterior cruciate ligament reconstruction: A prospective longitudinal study. Indian J Orthop 2015;49:136-42. [Google Scholar | PubMed]
- 8.Howells N. Injuries of the knee and leg. In: Blom A, Warwick D, Whitehouse MR, editors. Apley & Solomon’s System of Orthopaedics and Trauma. 10th ed. United States: CRC Press; 2017. p. 917. [Google Scholar | PubMed]
- 9.Çabuk H, Kuşku Çabuk F. Mechanoreceptors of the ligaments and tendons around the knee. Clin Anat 2016;29:789-95. [Google Scholar | PubMed]
- 10.Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am 1984;66:1072-6. [Google Scholar | PubMed]
- 11.Kim HJ, Lee JH, Lee DH. Proprioception in patients with anterior cruciate ligament tears: A meta-analysis comparing injured and uninjured limbs. Am J Sports Med 2017;45:2916-22. [Google Scholar | PubMed]
- 12.Matsumoto T, Kubo S, Sasaki K, Kawakami Y, Oka S, Sasaki H, et al. Acceleration of tendon-bone healing of anterior cruciate ligament graft using autologous ruptured tissue. Am J Sports Med 2012;40:1296-302. [Google Scholar | PubMed]
- 13.Song GY, Zhang J, Li X, Li Y, Feng H. Biomechanical and biological findings between acute anterior cruciate ligament reconstruction with and without an augmented remnant repair: A comparative in vivo animal study. Arthroscopy 2016;32:307-19. [Google Scholar | PubMed]
- 14.Nakayama H, Kambara S, Iseki T, Kanto R, Kurosaka K, Yoshiya S. Double-bundle anterior cruciate ligament reconstruction with and without remnant preservation - comparison of early postoperative outcomes and complications. Knee 2017;24:1039-46. [Google Scholar | PubMed]
- 15.Takazawa Y, Ikeda H, Kawasaki T, Ishijima M, Kubota M, Saita Y, et al. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med 2013;1(4):2325967113505076. [Google Scholar | PubMed]
- 16.Ahn JH, Lee YS, Ha HC. Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: Technical note. Arch Orthop Trauma Surg 2009;129:1011-5. [Google Scholar | PubMed]
- 17.Lee BI, Kwon SW, Kim JB, Choi HS, Min KD. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy 2008;24:560-8. [Google Scholar | PubMed]
- 18.Ochi M, Adachi N, Uchio Y, Deie M, Kumahashi N, Ishikawa M, et al. A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy 2009;25:117-22. [Google Scholar | PubMed]
- 19.Zantop T, Brucker PU, Vidal A, Zelle BA, Fu FH. Intraarticular rupture pattern of the ACL. Clin Orthop Relat Res 2007;454:48-53. [Google Scholar | PubMed]
- 20.Siebold R, Fu FH. Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 2008;24:1289-98. [Google Scholar | PubMed]
- 21.Adachi N, Ochi M, Uchio Y, Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 2000;120:128-33. [Google Scholar | PubMed]
- 22.Ochi M, Adachi N, Deie M, Kanaya A. Anterior cruciate ligament augmentation procedure with a 1-incision technique: Anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy 2006;22:463.e1-5. [Google Scholar | PubMed]
- 23.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 1982;64:883-8. [Google Scholar | PubMed]
- 24.Cho HJ, Lee JH, Bae DK, Song SJ, Yoon KH. The effect of meniscectomy on clinical result after ACL reconstruction. J Korean Arthrosc Soc 2010;14:7-12. [Google Scholar | PubMed]
- 25.Ahn JH, Lee SH, Choi SH, Lim TK. Magnetic resonance imaging evaluation of anterior cruciate ligament reconstruction using quadrupled hamstring tendon autografts: Comparison of remnant bundle preservation and standard technique. Am J Sports Med 2010;38:1768-77. [Google Scholar | PubMed]
- 26.Igdir V, Gencer B, Dogan O, Caliskan E, Orhan A, Demir Ozbudak S. The effects of remnant-preserving anterior cruciate ligament reconstruction on proprioception: A prospective comparative study. Acta Orthop Traumatol Turc 2023;57:109-15. . [Google Scholar | PubMed]
- 27.Liu Y, Li C, Ma N, Qi W, Gao F, Hu B, et al. Proprioceptive and clinical outcomes after remnant preserved anterior cruciate ligament reconstruction: Assessment with minimal confounding factors. Orthop Surg 2021;14:44-54. [Google Scholar | PubMed]
- 28.Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: Clinical and magnetic resonance imaging results. Arthroscopy 2011;27:1079-89. [Google Scholar | PubMed]
- 29.Lee JH, Bae DK, Song SJ, Cho SM, Yoon KH. Comparison of clinical results and second-look arthroscopy findings after arthroscopic anterior cruciate ligament reconstruction using 3 different types of grafts. Arthroscopy 2010;26:41-9. [Google Scholar | PubMed]
- 30.Kondo E, Yasuda K, Onodera J, Kawaguchi Y, Kitamura N. Effects of remnant tissue preservation on clinical and arthroscopic results after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med 2015;43:1882-92. [Google Scholar | PubMed]
- 31.Kim H, Lee J, Lee DH. Remnant-preserving versus conventional reconstruction of the anterior cruciate ligament: A systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2018;26:1060-9. [Google Scholar | PubMed]
- 32.Xie H, Fu Z, Zhong M, Deng Z, Wang C, Sun Y, et al. Effects of remnant preservation in anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Front Surg 2022;9:952930 [Google Scholar | PubMed]