Closed reduction with K-wire fixation offers a minimally invasive, effective approach for rare pediatric proximal humerus fractures, leading to excellent outcomes with early mobilization and minimal complications.
Dr. Sahil Chowdhary, Department of Orthopaedics, Dr. D.Y. Patil Medical College Hospital and Research Institute, Pimpri-Chinchwad, Maharashtra, India. E-mail: 22020366@dpu.edu.in
Introduction: Proximal humerus fractures are uncommon in children, accounting for <5% of pediatric fractures, with glenohumeral dislocation being an even rarer occurrence. These injuries are challenging due to the complex shoulder anatomy and the risk of growth disturbances, as the proximal humeral physis contributes ~80% of humeral growth. While many fractures can be managed conservatively, severe displacement or associated dislocations, such as Neer-Horwitz Type IV fractures, may require surgical intervention. Treatment options include K-wires, elastic stable intramedullary nailing, and plate fixation, with K-wires offering a less invasive alternative. We present a case of a 12-year-old girl with a Neer-Horwitz Type IV fracture-dislocation, successfully treated with closed reduction and K-wire fixation, demonstrating the effectiveness of this technique in preserving growth potential while achieving stability.
Case Report: We present the case of a 5-year-old right-hand dominant girl who sustained a severely displaced proximal humerus fracture with anterior glenohumeral dislocation after falling from a train berth. She landed on her outstretched left hand, resulting in severe pain, deformity, and loss of arm function. Radiographs and CT imaging confirmed a Neer-Horwitz Type IV fracture with significant displacement and varus angulation. Closed reduction and percutaneous K-wire fixation were performed under general anesthesia using the Kapandji and Jyoctiky maneuver, achieving satisfactory fracture alignment and joint reduction. Postoperatively, the arm was immobilized with a Dynaplast bandage, allowing for early pendulum exercises. The patient was discharged on post-operative day two with maintained reduction and proper K-wire positioning. This case highlights the efficacy of minimally invasive techniques for complex pediatric fractures, preserving growth potential while restoring joint stability.
Conclusion: This case highlights the effectiveness of closed reduction and K-wire fixation in managing complex pediatric proximal humerus fracture dislocations. The technique provides adequate stability while minimizing iatrogenic physeal damage, leading to excellent functional outcomes. However, each case should be approached individually, considering factors such as age, fracture pattern, and surgeon experience.
Keywords: Proximal humerus fracture, Glenohumeral dislocation, Pediatric orthopedic trauma
Proximal humerus fractures in the pediatric population are relatively uncommon, accounting for <5% of all pediatric fractures [1]. These injuries become even rarer when combined with glenohumeral dislocation, posing a unique management challenge due to complex anatomy and potential growth disturbances [2]. Most proximal humerus fractures in children can be managed non-operatively, thanks to the remarkable remodeling potential of young bones [3]. However, significant displacement or associated injuries may necessitate surgical intervention. The Neer-Horwitz classification system is widely used to categorize pediatric proximal humerus fractures, with Type IV fractures representing the most severe, involving displacement of more than 2/3 of the shaft width and often requiring surgical management [4]. When accompanied by glenohumeral dislocation, the complexity increases, with only a handful of cases reported in the literature [5]. Managing these injuries requires balancing adequate stability for healing and minimizing iatrogenic damage to the proximal humeral physis, responsible for approximately 80% of humeral longitudinal growth [6]. This case report describes the successful management of a rare Neer-Horwitz Type IV proximal humerus fracture with concurrent glenohumeral dislocation in a 5-year-old girl using closed reduction and percutaneous K-wire fixation.
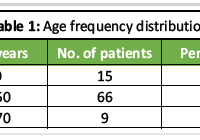
A 5-year-old right-hand dominant girl presented to the emergency department after falling approximately 5 ft from the second birth of a train onto her outstretched left hand, resulting in severe pain and visible shoulder deformity. She experienced immediate swelling and inability to move her left arm but had no loss of consciousness or other injuries. On examination, the left shoulder appeared grossly deformed with a visible sulcus sign, extensive swelling, and ecchymosis. The patient held her arm in slight abduction and external rotation, refusing movement due to pain. Neurovascular examination revealed intact distal pulses and no sensory or motor deficits. Radiographs revealed a severely displaced proximal humerus fracture with anterior glenohumeral dislocation. CT confirmed a Neer-Horwitz Type IV fracture with significant displacement and varus angulation (Fig. 1).
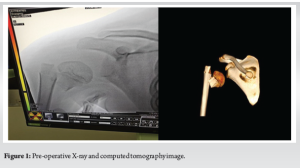
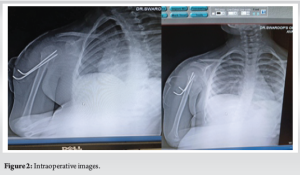
Under general anesthesia, closed reduction was achieved using the Kapandji and Jyoctiky maneuver, and the fracture was stabilized with percutaneous K-wires under fluoroscopic guidance (Fig. 2). Post-reduction alignment was satisfactory, with complete varus correction and mild residual translation (Fig. 3). The patient’s arm was immobilized with Dynaplast strapping (Fig. 4).
Follow-up at 2 weeks included Dynaplast removal, initiation of gentle pendulum exercises, and progressive rehabilitation. By 3 months, the patient had nearly full range of motion, with radiographs confirming complete healing without growth disturbance. At 6 months, she had returned to pre-injury activities, including sports, with no pain or functional limitations.
This case highlights the challenges of managing rare pediatric proximal humerus fractures with concurrent glenohumeral dislocation. Proximal humerus fractures account for 0.45% of all pediatric fractures, and the incidence of associated dislocation is exceptionally low, reported as 2.14% in some series [9]. The Neer-Horwitz classification guided treatment, as Type IV fractures often necessitate surgical intervention for optimal alignment and function [6]. Closed reduction with the Kapandji and Jyoctiky maneuver, followed by K-wire fixation, allowed for fracture reduction with minimal physeal disruption. This minimally invasive technique aligns with literature emphasizing the importance of preserving the proximal humeral physis to prevent growth complications [7]. Our decision for early mobilization with pendulum exercises at 2 weeks contrasts with more conservative protocols recommending longer immobilization [2]. However, this approach facilitated rapid functional recovery, with the patient regaining full shoulder motion within 3 months. Literature supports the use of K-wires in pediatric proximal humerus fractures, with studies showing comparable outcomes to intramedullary nailing but with fewer complications [8]. Our case’s favorable outcome, with no growth disturbance or avascular necrosis, aligns with findings that careful K-wire placement reduces iatrogenic risks [11].
This case report illustrates the successful management of a rare Neer-Horwitz Type IV proximal humerus fracture with concurrent glenohumeral dislocation in a pediatric patient using closed reduction and K-wire fixation. The minimally invasive approach preserved the proximal humeral physis, allowing for complete fracture healing and full functional recovery. This case underscores the importance of individualized treatment strategies and highlights the efficacy of early rehabilitation in achieving optimal outcomes. This case demonstrates that even complex pediatric fractures, such as a Neer-Horwitz Type IV proximal humerus fracture with concurrent glenohumeral dislocation, can be successfully managed with a minimally invasive approach. Closed reduction and percutaneous K-wire fixation provided adequate stability while preserving the proximal humeral physis, enabling rapid functional recovery and preventing long-term complications.
Early initiation of physiotherapy played a key role in restoring the full range of motion, highlighting the importance of individualized, evidence-based management strategies for rare and challenging pediatric fractures.
Early recognition and classification of severe pediatric proximal humerus fractures with lenohumeral dislocation are essential for optimal outcomes. Closed reduction with percutaneous K-wire fixation provides a minimally invasive solution, balancing stability with growth plate preservation. Early mobilization, supported by close radiographic follow-up, promotes faster recovery and minimizes long-term complications, emphasizing the value of an individualized, patient-centered approach.
References
- 1.Pahlavan S, Baldwin KD, Pandya NK, Namdari S, Hosalkar H. Proximal humerus fractures in the pediatric population: A systematic review. J Child Orthop 2011;5:187-94. [Google Scholar | PubMed]
- 2.Bahrs C, Zipplies S, Ochs BG, Rether J, Oehm J, Eingartner C, et al. Proximal humeral fractures in children and adolescents. J Pediatr Orthop 2009;29:238-42. [Google Scholar | PubMed]
- 3.Popkin CA, Levine WN, Ahmad CS. Evaluation and management of pediatric proximal humerus fractures. J Am Acad Orthop Surg 2015;23:77-86. [Google Scholar | PubMed]
- 4.Neer CS 2nd, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res 1965;41:24-31. [Google Scholar | PubMed]
- 5.Fannouch G, Al Khalife YI, Al Turki AS, Jawadi AH. Traumatic pediatric shoulder fracture dislocation treated with closed reduction and intramedullary nailing: A case report. Trauma Case Rep 2017;9:22-6. [Google Scholar | PubMed]
- 6.Dobbs MB, Luhmann SL, Gordon JE, Strecker WB, Schoenecker PL. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop 2003;23:208-15. [Google Scholar | PubMed]
- 7.Pritchett JW. Growth plate activity in the upper extremity. Clin Orthop Relat Res 1991;268:235-42. [Google Scholar | PubMed]
- 8.Hutchinson PH, Bae DS, Waters PM. Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: A comparison of complications and early radiographic results. J Pediatr Orthop 2011;31:617-22. [Google Scholar | PubMed]
- 9.Sénès FM, Catena N. Intramedullary osteosynthesis for metaphyseal and diaphyseal humeral fractures in developmental age. J Pediatr Orthop B 2012;21:300-4. [Google Scholar | PubMed]
- 10.Hong P, Rai S, Liu R, Tang X, Li J. Glenohumeral joint dislocation is rare in children with proximal humeral fractures: A descriptive study and literature review. BMC Musculoskelet Disord 2022;23:36. [Google Scholar | PubMed]
- 11.Beaty JH. Fractures of the proximal humerus and shaft in children. Instr Course Lect 1992;41:369-72. [Google Scholar | PubMed]