Preoperative intravenous and intraoperative topical administration of tranexamic acid in patients of Intertrochanteric fractures surgeries appears to be an effective and safe practice in reducing postoperative blood loss.
Dr. Virender Kumar, Department of Orthopaedics, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India. Email- drvirender80@gmail.com
Introduction: Intertrochanteric (IT) fracture surgeries make up a significant portion of trauma operations worldwide. The routine use of tranexamic acid (TXA) for these surgeries is not common in current practice at most places. This prospective study evaluated its efficacy in reducing perioperative blood loss and accentuating its potential for a better outcome.
Materials and Methods: A total of 100 patients were divided equally into two groups, A and B. Group A was given preoperative intravenous (IV) TXA and intraoperative topical TXA through the drain, while Group B was given preoperative and intraoperative normal saline. Both groups were comparable in age, body mass index, preoperative hemoglobin (Hb), surgery performed, and duration of surgery.
Results: The mean drain volume, postoperative Hb, fall of Hb, and total blood loss were all significantly less in Group A as compared to Group B (P < 0.01). None of the patients in either group received more than one unit of blood transfusion. No complications were seen in any of the patients till the final follow-up.
Conclusion: In comparison to other studies, our study is in agreement that TXA overall helps in blood conservation; however, our study is unique in the way that the combination of preoperative IV and intraoperative topical TXA has resulted in the best possible results.
Keywords: Tranexamic acid, blood loss, intertrochanteric fractures, dynamic hip screw, dynamic condylar plate, intravenous, topical, drain volume.
Intertrochanteric (IT) fracture surgeries are currently some of the most commonly performed elective as well as emergency orthopedic procedures. Considerable blood loss after such surgeries is problematic, and postoperative blood transfusion carries a substantial risk of both immunologic reaction and transmission of diseases. Total blood loss (TBL) and thus the rate of transfusion, is greater for extracapsular hip fractures compared to intracapsular hip fractures. Therefore, the adoption of a perioperative blood management program has been widely advocated with the main aim of reducing the likelihood of allogeneic blood transfusion (ABT). Various methods have been suggested to reduce blood loss following surgery, such as autotransfusion, hypotensive anaesthesia, intravenous (IV) tranexamic acid (TXA) administration, intra-articular (IA) TXA injection, and temporary drain clamping. There are four possible routes for administering TXA to reduce blood loss in (IT fracture) surgeries: oral, intramuscular (IM), IV, and IA [1]. The time taken for maximum plasma levels of TXA to be reached has been reported to be 2 h for oral, 30 min for IM and 5–15 min for IV administration) [2]. Although some studies have found an increased risk of thromboembolic events in groups receiving TXA, larger studies and meta-analyses have uniformly found no increased risk) [3,4]. The topical application of TXA provides a high drug concentration at the site of the wound and a low systemic concentration) [5]. In IT fracture surgeries, there is a lack of capsular envelope, like in the knee, and there is significant soft tissue dissection leading to a large raw area, thereby carrying the possibility of poor efficacy of topical TXA administration in IT fracture surgeries. Given the paucity of literature regarding the effectiveness of TXA in IT fracture surgeries, this prospective study was conducted to evaluate its efficacy in reducing perioperative blood loss.
Hemoglobin (Hb) concentration was measured 1 day before surgery. Both groups were assessed in terms of the amount of blood loss, drain output, fall in haematocrit, need for blood transfusion, and complications, if any. Only patients in whom plating was considered appropriate were chosen for the study. After randomization, Group A (50 patients) received 2g IV TXA 2 h before surgery, while Group B (50 patients) received a placebo in the form of normal saline (NS). After fracture fixation by either a dynamic hip screw or dynamic condylar plate, the wound was closed over a negative suction drain. A single dose of 2 g of TXA (20 mL) in 20 mL of NS was introduced through the drain after complete wound closure, whereas a similar volume of 40 mL of NS was instilled for the placebo group, and the drain was clamped for 2 h after this. Intraoperative blood transfusion was done as per the anaesthetist’s requirement for hypotension and exceeding allowable blood loss. The drain was removed after 48 h of surgery or a break in the column of drain fluid, whichever was earlier, and the postoperative drain output volume was measured and noted. Hb concentration on the third postoperative day after surgery was noted along with details of blood loss and blood transfusions. ABT was considered if the Hb fell by 4 g% or haematocrit (calculated as per formula) dropped by 28% from baseline any time in the first 48 h of surgery or a drain collection of ≥ 500 mL (possible ongoing loss) in the first 8–10 h) [6,7]. The primary outcomes checked were TBL volume and drain output. Blood loss after surgery was estimated using two different methods. The first was the standard clinical method, where blood loss was taken as the volume recovered from the drain at removal. The second method was based on Hb balance to include the hidden loss inside the operative area, too. Blood volume was estimated according to the method of Nadler [6]. The secondary outcome measured was the number of blood units transfused.
Observations
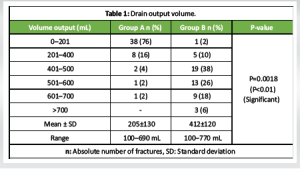
Group A (n = 50) patients received TXA, while Group B (n = 50) patients received a placebo. It was observed that both groups were comparable in terms of age, sex, body mass index (BMI), side involvement, implant choice, duration of surgery, and intraoperative blood loss, but differed significantly in the drain output volume, postoperative Hb, mean TBL and postoperative blood transfusion (POBT) (Table 1).
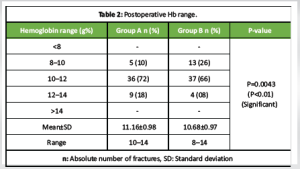
The mean preoperative Hb in Groups A and B was 12.1 ± 1.07 and 12.41 ± 0.98 g%, respectively (Table 2).
The significant fall in Hb percentage is shown in Fig. 1. P = 0.0034 (P < 0.01) (Fig. 1).
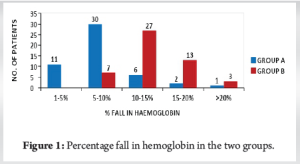
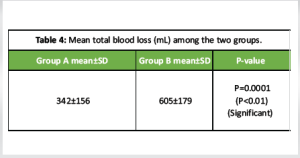
The mean fall in Group A was 0.94 (7.76%) and 1.73 (14%) in Group B (Table 3 and 4).

A total of nine patients (18%) in Group A and six patients (12%) in Group B required intraoperative blood transfusion. All nine patients requiring intraoperative blood transfusion had a duration of surgery of more than 2 h in Group A. Similarly, in Group B, four out of six requiring it had a duration of surgery of more than 2 h. Only one patient (2%) in the TXA group required POBT, whereas five patients (10%) in the control group required POBT (each patient receiving only one unit). All these five had >500 mL drain output in the first 10 h.
Perioperative blood loss is an important complication that leads to significant morbidity in the form of anaemia, resulting in delayed recovery and the need for postoperative transfusion. A variety of measures have been advocated to minimize these complications, like the use of preoperative ABT, acute normovolemic hemodilution, re-transfusion, tourniquet, and the use of antifibrinolytic agents like TXA. TXA, being an antifibrinolytic, is widely used in many clinical situations, including trauma, to reduce blood loss and prevent consequent morbidity and mortality. IT fracture surgeries involve a fair amount of soft-tissue dissection and are performed without any tourniquet. As a result, they lead to a significant amount of perioperative blood loss, thereby indicating a requirement to reduce this loss. Further, due to extensive exposure to raw bleeding surfaces during dissection, the possibility of topical TXA acting is higher, at the same time it has a chance to get absorbed into systemic circulation reducing its concentration locally, unlike knee surgeries, where topical TXA remains in high concentration due to the capsular envelope and less raw surface causing low systemic absorption. This absorption of topical TXA into the systemic circulation may not provide enough blood concentration to act as in IV TXA, so absorption is a possible disadvantage to be considered. A variety of routes of administration (IV, topical, and oral) have been advocated in the literature, though there is no consensus on its dosage, schedule, or route of administration. There is a lack of literature on the optimal timing for administering oral TXA. The peak levels are attained immediately after administration of topical TXA locally at the site while IV TXA achieves its peak levels 2–3 h after administration. Based on its pharmacokinetics, topical TXA is administered in the wound just after closure, whereas the administration of IV TXA 2 h preoperatively seems appropriate) [8]. Therefore, the present study was conducted to evaluate the efficacy of the combined use of preoperative IV and intraoperative topical application of TXA in reducing perioperative blood loss after IT fracture surgeries. The present study was conducted on 100 patients undergoing IT fracture surgeries, who were divided into two groups, having 50 patients each, with one group receiving TXA and the other group receiving a placebo in the form of IV and topical NS. It was observed that both groups were comparable in terms of age, sex, BMI, side involvement, implant choice, preoperative implant, duration of surgery, and intraoperative blood loss. Drain volume is an important indicator of postoperative blood loss, whereas TBL as calculated by the Hb difference formula, indicates perioperative blood loss. The mean drain output volume observed in the present study compared to other studies is shown in Table 5. It is quite evident that the combination of IV and topical TXA was observed to be quite effective in reducing the drain output, with a mean difference of 207 mL between the two groups. Zufferey et al. had a slightly higher drain output in the TXA group compared to the control group despite two IV doses (15 mg/kg), possibly because the drug concentration was higher at the wound site following topical TXA, as compared to IV route, as evident in the present study) [9]. Kang et al. and Kim et al. in their studies involving hip arthroplasty observed a slightly lower mean drain volume. It could be due to their use of a higher dosage (3 g topical TXA and 1 g/10 mL NS, respectively) [10,11]. However, in the above studies, the difference in the drain output between the TXA group and control group is less compared to the present study, which shows the better efficacy of the combined dose of TXA. Vijay et al. observed a very low day 0 drain output possibly due to higher IV doses of TXA (0.5 g in 50 mL NS before surgery followed by continuous IV infusion throughout surgery) [12]. However, zero-day drain output may not truly reflect the actual drain output. The higher drain volume in the study by Lošťák et al. may be due to only one dose of IA TXA) [13]. Aggarwal et al. reported lesser drain volumes with IA TXA (252 mL) in their study on TKA, which is lower than that of the present study, which could be due to the lesser dissection required in TKA and also due to the capsular envelope in the joint providing a tamponade effect, unlike that of IT fracture surgeries proving higher efficacy of IA TXA in knee surgeries) [14]. Patients with a longer duration of surgery have drain output on the higher side, hence suggesting that the duration of surgery and extent of dissection increased the postoperative blood loss. The mean postoperative Hb (in g/dL) in the present study versus comparative studies is shown in Table 5.

However, the data of postoperative Hb alone in each study carries no significance on its own, hence the fall of Hb is calculated to determine the efficacy of TXA. In the present study, the postoperative Hb values were noted on the 3rd day after surgery. It was assumed that by the third postoperative day, the effect of haemodilution on postoperative Hb would be neutralised. The mean difference between pre- and postoperative Hb in various studies is listed in Table 5. Vijay et al. used an IV dose with a second continuous infusion during the surgery. This may indicate better efficacy of the IV regimen since the fall of Hb is less; however, the present study has a simpler way of administration with similar efficacy) [12]. Studies comparing different modes of administration have reported almost similar reductions in pre- and postoperative Hb. The former four studies with the IV route in hip surgeries show higher fall in postoperative Hb compared to the present study thus making our combined route a better alternative, supported by the study by Kwak et al. [15] Though Kang et al. and Sanz-Reig et al. used the topical route in their hip surgeries, they still had higher falls which could be due to the single route of administration of TXA as compared to the present study) [10,16]. In the present study, only one patient (2%) in the TXA group required POBT, whereas five patients (10%) in the control group required it (each patient receiving only one unit). The only patient in the TXA group who received a transfusion was due to the presence of persistent hypotension. The number of patients requiring POBT as observed in different studies is shown in Table 5. These observations reaffirm the view that TXA application in all forms (IV, topical, and oral) results in decreased blood loss, thereby reducing the need for ABT to maintain postoperative Hb. Moreover, the triggering criteria for POBT are different in different studies. The overall lower incidence of transfusion in the present study in both the groups could be due to a lenient trigger point of fall of postoperative Hb by 4 g/dL, whereas, the study conducted by Carling et al., Kang et al., Kwak et al., and Gautam et al. shows an increased percentage of transfusion rates owing to their strict transfusion trigger point at postoperative Hb of 8 g/dL) [10,15,17,18]. The TBL indicates overall blood loss as seen in drain output as well as internal collection in the tissue or the residual blood in the joint capsule. Thus, the TBL calculation is a better indicator of actual blood loss following the surgical procedure. It was calculated using the formula described by Nadler et al. [6]. A comparison of our study with other studies is shown in Table 5. The studies by Gandhi et al., Kwak et al., and Xie et al. have shown similar results to our study) [15,19,20]. The higher TBL observed by Kang and Sanz-Reig et al. could be related to the single dose of topical TXA at a lesser concentration, whereas, Carling et al. observed a higher TBL which could be explained by the extensive dissection in hip surgeries and also that topical TXA has a better or similar efficacy in both knee and hip) [10,16,17]. In the present study, none of the patients showed any clinical signs or symptoms of deep vein thrombosis or pulmonary embolism in the immediate postoperative period and subsequent follow-ups. Thus, our findings are consistent with the studies of Kang et al. and Sanz Reig et al., both of which used a topical route of TXA administration) [10,16]. However, the study with IV routes has reported some incidence of venous thromboembolism (VTE) as seen in the study by Zufferey et al. (15% in the TXA group vs. 5% in the control group) [9]. All the above three studies relied on clinical parameters to assess the incidence of VTE. Therefore, the use of topical TXA at the dose used in the present study is both effective and safe in reducing perioperative blood loss in patients undergoing IT fracture surgeries. In the patients treated with TXA, there was a significant reduction in blood loss recovered in the surgical drain, a lower decrease in Hb concentration postoperatively, and an overall reduction in TBL. The decrease in blood loss due to TXA administration was also associated with a reduction in the number of blood units transfused during the postoperative period. It can be stated that the combined IV and topical route is more effective than individual routes and is both cost-effective and safe.
Limitation
The initial limitation of this study was the potential for surgeon bias, as involving a single surgeon across all cases could have eliminated variances in surgical procedures and preferences affecting surgery duration and dissection extent. Moreover, being a single-center study may restrict the generalizability of the findings. However, this study included multiple surgeons with varying levels of experience. Future research involving larger sample sizes and randomized controlled trials at multiple centers may yield stronger evidence for the effectiveness of TXA in surgeries for IT fractures. All procedures followed were based on the ethical standards of the responsible committee on human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients to be included in the study. Trial registered at Clinical Trials Registry – India bearing no.: CTRI/2023/08/056281 registered on August 08, 2023. This study is not funded or sponsored by any individual, group or society/institution.
The findings and observations from this study indicate that administering TXA intravenously preoperatively and topically during IT fracture surgeries is a safe and effective strategy. This approach markedly diminishes postoperative blood loss and lowers the requirement for blood transfusions after surgery.
TXA usage leads to reduced blood loss and lower transfusion needs in IT fracture surgeries. Patients receiving TXA experienced a marked decrease in blood loss in the surgical drain, a smaller decline in Hb levels post-surgery, and an overall reduction in TBL. This decrease in blood loss associated with TXA also corresponds to fewer blood units transfused after surgery. It can be concluded that using both IV and topical methods together is more effective than using each method separately, proving to be safe and cost-efficient.
References
- 1.Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S. Timing of the administration of tranexamic acid for maximum reduction in blood loss in arthroplasty of the knee. J Bone Joint Surg Br 2001;83:702-5. [Google Scholar]
- 2.Benoni G, Björkman S, Fredin H. Application of pharmacokinetic data from healthy volunteers for the prediction of plasma concentrations of tranexamic acid in surgical patients. Clin Drug Invest 1995;10:280-7. [Google Scholar]
- 3.Emara WM, Moez KK, Elkhouly AH. Topical versus intravenous tranexamic acid as a blood conservation intervention for reduction of post-operative bleeding in hemiarthroplasty. Anesth Essays Res 2014;8:48-53. [Google Scholar]
- 4.Duncan CM, Gillette BP, Jacob AK, Sierra RJ, Sanchez-Sotelo J, Smith HM. Venous thromboembolism and mortality associated with tranexamic acid use during total hip and knee arthroplasty. J Arthroplasty 2015;30:272-6. [Google Scholar]
- 5.De Bonis M, Cavaliere F, Alessandrini F, Lapenna E, Santarelli F, Moscato U, et al. Topical use of tranexamic acid in coronary artery bypass operations: A double-blind, prospective, randomized, placebo-controlled study. J Thorac Cardiovasc Surg 2000;119:575-80. [Google Scholar]
- 6.Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery 1962;51:224-32. [Google Scholar]
- 7.Quintó L, Aponte JJ, Menéndez C, Sacarlal J, Aide P, Espasa M, et al. Relationship between haemoglobin and haematocrit in the definition of anaemia. Trop Med Int Health 2006;11:1295-302. [Google Scholar]
- 8.Pilbrant Å, Schannong M, Vessman J. Pharmacokinetics and bioavailability of tranexamic acid. Eur J Clin Pharmacol 1981;20:65-72. [Google Scholar]
- 9.Zufferey PJ, Miquet M, Quenet S, Martin P, Adam P, Albaladejo P, et al. Tranexamic acid in hip fracture surgery: A randomized controlled trial. Br J Anaesth 2010;104:23-30. [Google Scholar]
- 10.Kang JS, Moon KH, Kim BS, Yang SJ. Topical administration of tranexamic acid in hip arthroplasty. Int orthop 2017;41:259-63. [Google Scholar]
- 11.Kim JT, Kim HH, Kim JH, Kwak YH, Chang EC, Ha YC. Mid-term survivals after cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients. J Arthroplasty 2018;33:777-82. [Google Scholar]
- 12.Vijay BS, Bedi V, Mitra S, Das B. Role of tranexamic acid in reducing postoperative blood loss and transfusion requirement in patients undergoing hip and femoral surgeries. Saudi J Anaesth 2013;7:29-32. [Google Scholar]
- 13.Lošťák J, Gallo J, Večeřa M, Špička J, Langova K. Local application of tranexamic acid in total hip arthroplasty decreases blood loss and consumption of blood transfusion. Acta Chir Orthop Traumatol Cech 2017;84:254-62. [Google Scholar]
- 14.Aggarwal AK, Singh N, Sudesh P. Topical vs intravenous tranexamic acid in reducing blood loss after bilateral total knee arthroplasty: A prospective study. J Arthroplasty 2016;31:1442-8. [Google Scholar]
- 15.Kwak DK, Jang CY, Kim DH, Rhyu SH, Hwang JH, Yoo JH. Topical tranexamic acid in elderly patients with femoral neck fractures treated with hemiarthroplasty: Efficacy and safety?- A case-control study. BMC Musculoskelet Disord 2019;20:228. [Google Scholar]
- 16.Sanz-Reig J, Mas Martinez J, Verdu Román C, Morales Santias M, Martínez Gimenez E, De Puga DB. Matched cohort study of topical tranexamic acid in cementless primary total hip replacement. Eur J Orthop Surg Traumatol 2018;28:1335-9. [Google Scholar]
- 17.Carling MS, Jeppsson A, Eriksson BI, Brisby H. Transfusions and blood loss in total hip and knee arthroplasty: A prospective observational study. J Orthop Surg Res 2015;10:48. [Google Scholar]
- 18.Gautam PL, Katyal S, Yamin M, Singh A. Effect of tranexamic acid on blood loss and transfusion requirement in total knee replacement in the Indian population: A case series. Indian J Anaesth 2011;55:590-3. [Google Scholar]
- 19.Xie J, Hu Q, Huang Q, Chen G, Zhou Z, Pei F. Efficacy and safety of tranexamic acid in geriatric hip fracture with hemiarthroplasty: A retrospective cohort study. BMC Musculoskelet Disord 2019;20:304. [Google Scholar]
- 20.Gandhi R, Evans HM, Mahomed SR, Mahomed NN. Tranexamic acid and the reduction of blood loss in total knee and hip arthroplasty: A meta-analysis. BMC Res Notes 2013;6:184. [Google Scholar]
- 21.Blanié A, Bellamy L, Rhayem Y, Flaujac C, Samama CM, Fontenay M, et al. Duration of postoperative fibrinolysis after total hip or knee replacement: A laboratory follow-up study. Thromb Res 2013;131:e6-11. [Google Scholar]
- 22.Lee C, Freeman R, Edmondson M, Rogers BA. The efficacy of tranexamic acid in hip hemiarthroplasty surgery: An observational cohort study. Injury 2015;46:1978-82. [Google Scholar]
- 23.Irwin A, Khan SK, Jameson SS, Tate RC, Copeland C, Reed MR. Oral versus intravenous tranexamic acid in enhanced-recovery primary total hip and knee replacement: Results of 3000 procedures. Bone Joint J 2013;95:1556-61. [Google Scholar]
- 24.Haj-Younes B, Sivakumar BS, Wang M, An VV, Lorentzos P, Adie S. Tranexamic acid in hip fracture surgery: A systematic review and meta-analysis. J Orthop Surg (Hong Kong) 2019;28:2309499019887995. [Google Scholar]
- 25.Whiting DR, Gillette BP, Duncan C, Smith H, Pagnano MW, Sierra RJ. Preliminary results suggest tranexamic acid is safe and effective in arthroplasty patients with severe comorbidities. Clin Orthop Relat Res 2014;472:66-72. [Google Scholar]