Timely surgical fixation using locking plates in displaced sternal fractures ensures optimal chest wall stability and faster functional recovery.
Dr. Rakesh Dhaka, Department of Orthopaedics, All India Institute of Medical Sciences, Raipur, Chhatisgarh, India. E-mail: dhakarakesh341@gmail.com
Introduction: Sternal fractures, although uncommon, pose significant clinical challenges due to potential complicationssuch as respiratory compromise and chest wall instability. Prompt diagnosis and appropriate management are crucial to reduce morbidity.
Case Report: We report a case of a 43-year-old male who sustained displaced sternal and rib fractures following a road traffic accident. A midline incision allowed open reduction and internal fixation using a 3.5 mm locking reconstruction plate for the sternum and a 2 mm plate for the rib. Postoperative recovery was uneventful, with significant pain relief and improved respiratory function.
Conclusion: This case reinforces the importance of early surgical intervention in unstable sternal fractures. Locking plate fixation offers superior biomechanical stability, faster healing, and fewer complications compared to conservative management or traditional wiring techniques.
Keywords: Sternal fracture, chest trauma, locking plate fixation, rib fracture, surgical stabilization.
A sternum fracture is relatively rare, representing about 0.5% of all fractures. It usually occurs due to severe traumatic events such as car accidents or high-impact blunt trauma to the chest, with such injuries happening in 3–8% of these situations [1-5]. It is characterized by severe pain, respiratory compromise, and deformity of the anterior chest wall, necessitating careful monitoring in an intensive or critical care unit. In older individuals, sternum fractures can also result from low-energy trauma [1,2,4]. Associated injuries must be assessed promptly, and management should include adequate analgesia to prevent respiratory distress, as well as ruling out pulmonary contusion and respiratory insufficiency. When it comes to fixation, surgical plating offers superior stability and more effective restoration of chest wall function compared to sternal wiring. Recent studies indicate that plating leads to better bone healing, fewer complications, and reduced rates of non-union [3,4]. In this particular case, sternal plating was performed through a midline incision, along with rib plating. This approach allowed for chest wall exploration to rule out any underlying trauma and facilitated the fixation of both the sternum and rib fractures, providing stability to the chest wall.
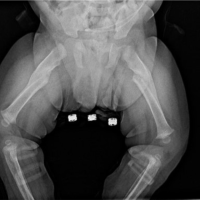
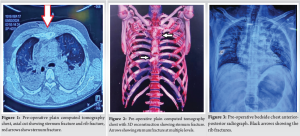
A 43-year-old man with a history of a road traffic accident arrived at the trauma and emergency department. On initial assessment, the patient was conscious and hemodynamically stable but complained of severe chest pain and pain in the right lower limb. Primary and secondary surveys were conducted according to the advanced trauma life support protocol. Clinical examination, an open wound was noted on the proximal right tibia with visible bone fragments, suggesting a Grade IIIB open fracture.. There was noticeable limb deformity, abnormal mobility, and crepitus at the fracture site. The affected limb was neurovascularly intact distally. Accompanied by severe chest pain, especially in the mid-sternum region, along with a chest wall deformity. Palpation elicited tenderness over the mid-sternum. The chest compression test was positive. Crepitus was present over the left lateral chest wall, and there was pain radiating to the sternum on movement of both glenohumeral joints. However, a full range of motion was preserved. Breath sounds were reduced on the left side. After stabilization, computed tomography (CT) (Fig. 1, 2) and a plain chest X-ray (Fig. 3) scan of the chest were performed. These imaging studies showed a fracture in the proximal one-third of the tibia shaft with an open wound on the medial side, a transverse fracture of the corpus divided into three fragments, and two associated rib fractures. Following initial stabilization, an intercostal drainage tube was placed on the left side of the chest, and the patient was monitored overnight in the critical care unit. Surgery was indicated due to severe deformity with dislocated and overlapping sternal edges. The primary goal was to restore anatomical alignment, ensure chest wall stability, and prevent complications such as chronic nonunion or restrictive pulmonary dysfunction.
Hematological and biochemical parameters were at presentation and during the perioperative period; the patient’s blood investigations were within normal limits:
- Hemoglobin: 11.2 g/dL
- Total leukocyte count: Normal
- Erythrocyte sedimentation rate and C-reactive protein: Within normal limits during evaluation for definitive tibial fixation
- Liver function tests, renal function tests, prothrombin time/international normalized ratio, and activated partial thromboplastin time: All within normal range.
Intraoperative and postoperative parameters remained stable. There was no requirement for blood transfusion as there were no significant drops in hemoglobin or other parameters post-surgery.
Intraoperative findings
The patient was scheduled for open reduction and internal fixation using standard plating. The patient was taken to the operating theater after obtaining informed high-risk consent. General anesthesia was administered with endotracheal intubation, and broad-spectrum intravenous antibiotics were given preoperatively. The patient was positioned supine with a small bolster placed between the scapulae to mildly extend the thoracic spine and expose the anterior chest wall. A midline longitudinal incision was made to open the chest wall, allowing visualization of the fracture and examination of the underlying heart and lung tissue (Fig. 4). The sternal edges were realigned and approximated, any interposed soft tissue was removed, and a 3.5 mm straight locking reconstruction plate was applied for fixation (Fig. 5). Locked screws were placed in the proximal fragment, and standard screws were replaced with locked screws to ensure secure plate-screw fixation. Four locking screws were used on the distal-inferior side, and three locking screws on the proximal-superior side, all achieving a stable fixation (Fig. 6).
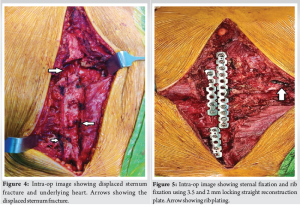
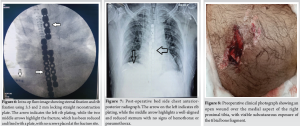
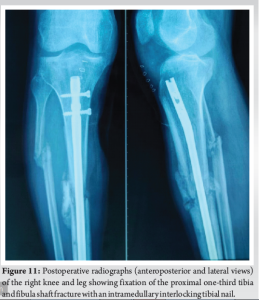
On the right side, the fractured 8th rib was reduced and stabilized with a 2 mm reconstruction plate. The wound was closed with a negative-pressure drain to prevent hematoma formation, which was removed after 48 h.Post-op X-ray (Fig. 7) shows well-aligned and reduced sternum with no evidence of pneumothorax or hemothorax.The open wound on the medial aspect of the proximal tibia (Fig. 8) was initially managed with urgent debridement, for the proximal tibia 1/3rd shaft fracture (Fig.-9) application of an external fixator (Fig. 10), and initiation of negative pressure wound therapy. After ensuring the wound was healthy, a flap coverage procedure was done by the plastic surgery team. Following flap maturation, the external fixator was removed, and the patient underwent closed reduction and internal fixation using tibial interlocking (intramedullary interlocking) nailing (Fig. 11).
The patient showed significant clinical improvement following surgical fixation. Chest wall stability was restored, which allowed for improved respiratory mechanics. The patient was extubated successfully in the immediate post-operative period and shifted to the intensive care unit for further monitoring. Adequate pain control was achieved with a multimodal analgesic approach, including parenteral opioids and local anesthetic infiltration at the incision site, and early mobilization was encouraged starting on post-operative day 3. Serial chest X-rays confirmed proper alignment of the sternum and rib with no displacement of hardware or new pleural collections. The patient tolerated breathing exercises and incentive spirometry well, with gradual improvement in pulmonary function.
There were no immediate or delayed post-operative complications. Specifically, there were:
- No signs of surgical site infection
- No implant-related complications (e.g., loosening or failure)
- No hematoma or seroma formation, as the negative pressure drain was removed at 48 h with minimal output
- No need for blood transfusion, with hemoglobin remaining stable postoperatively.
Follow-up at 2 weeks and 6 weeks showed good wound healing, improved respiratory effort, and no complaints of pain at rest. The patient returned to partial weight-bearing mobilization for the tibial fracture and continued physiotherapy for chest expansion and limb rehabilitation.
Sternal fractures, although relatively rare, are significant injuries that can lead to severe pain, respiratory compromise, and chest wall instability, necessitating careful evaluation and management. The literature emphasizes that while most sternal fractures are managed conservatively, surgical intervention becomes essential in cases of displaced fractures, instability, non-union, or severe pain interfering with respiration [1]. The primary cause of sternal fractures is high-impact trauma, particularly motor vehicle accidents, where direct anterior blunt trauma to the chest occurs due to seatbelt injuries or steering wheel impact [2]. The incidence of sternal fractures has increased with seatbelt legislation, although seatbelts remain crucial for overall injury reduction [1]. Less commonly, sternal fractures result from falls, sports injuries, or pathological causes such as osteoporosis [3]. Patients typically present with severe localized pain, tenderness, and deformity at the fracture site, often accompanied by associated rib fractures, pulmonary contusions, or vertebral fractures [4]. Diagnostic imaging, including lateral chest X-rays and CT scans, plays a crucial role in assessing the extent of injury [5,6]. Conservative treatment remains the mainstay for stable, non-displaced fractures, involving adequate analgesia, respiratory physiotherapy, and immobilization [1]. However, surgical fixation is indicated for displaced fractures, non-unions, and fractures contributing to chest wall instability and respiratory distress [7].
Surgical techniques and fixation methods
The choice of fixation method depends on fracture type and surgeon preference. Literature suggests that plating is superior to wiring due to better stability, improved bone healing, and reduced non-union rates [8]. Techniques include:
- Locking compression plates (LCP): Studies have demonstrated that double LCP fixation provides excellent functional outcomes with minimal complications [2].
- Titanium plates: Low-profile titanium plates offer stability while minimizing mediastinal injury risks [7].
- Bone grafts and hybrid fixation: Some cases of non-union benefit from bone grafting in addition to plating [8].
- Minimally invasive fixation: Emerging techniques aim to reduce surgical trauma and expedite recovery, with biomechanical studies supporting less-invasive fixation approaches in selected patients [4,9].
In addition, a comprehensive literature review also emphasizes the value of timely surgical stabilization to reduce the risk of long-term complications such as chronic pain and pseudarthrosis, while advanced radiologic imaging assists in guiding preoperative planning and postoperative assessment [6,10]. A systematic review comparing conservative versus surgical treatment found that surgical fixation leads to faster pain relief, improved chest wall function, and lower rates of non-union [3]. However, long-term data are still limited, and further research is needed to establish standardized surgical indications [5]. In the present case, the decision for surgical intervention was driven by the presence of a displaced transverse sternal fracture with associated rib fractures and chest wall instability. The use of a 3.5 mm locking reconstruction plate provided effective stabilization, preventing further displacement and promoting healing. In addition, rib plating ensured comprehensive thoracic stability, minimizing respiratory complications. Postoperatively, early mobilization and respiratory physiotherapy were essential in preventing pulmonary complications such as pneumonia or atelectasis [4]. The patient’s outcome was favorable, with significant pain reduction and radiographic evidence of union.
This study highlights the necessity of surgical intervention in displaced sternal fractures with instability. Literature strongly supports plating over wiring for its biomechanical superiority, enhanced stability, and improved healing outcomes. The findings reinforce that early surgical fixation, particularly with locking plates, significantly reduces pain, improves respiratory function, and lowers complication rates. Moreover, multidisciplinary management involving trauma, orthopedic, and thoracic specialists ensures optimal patient recovery. Future research should focus on refining surgical techniques and evaluating long-term outcomes to establish standardized treatment protocols.
In cases of displaced or unstable sternal fractures, surgical stabilization using locking plates should be considered as the first-line approach. It enhances chest wall integrity, allows early mobilization, reduces pain, and prevents long-term complications such as non-union or respiratory impairment.
References
- 1.Klei DS, De Jong MB, Öner FC, Leenen LP, Van Wessem KJ. Current treatment and outcomes of traumatic sternal fractures-a systematic review. Int Orthop 2019;43:1455-64. [Google Scholar | PubMed]
- 2.Kalberer N, Frima H, Michelitsch C, Kloka J, Sommer C. Osteosynthesis of sternal fractures with double locking compression plate fixation: A retrospective cohort study. Eur J Orthop Surg Traumatol 2020;30:75-81. [Google Scholar | PubMed]
- 3.Harston A, Roberts C. Fixation of sternal fractures: A systematic review. J Trauma 2011;71:1875-9. [Google Scholar | PubMed]
- 4.Schulz-Drost S, Mauerer A, Grupp S, Hennig FF, Blanke M. Surgical fixation of sternal fractures: Locked plate fixation by low-profile titanium plates-surgical safety through depth limited drilling. Int Orthop 2014;38:133-9. [Google Scholar | PubMed]
- 5.Al-Qudah A. Operative treatment of sternal fractures. Asian Cardiovasc Thorac Ann 2006;14:399-401. [Google Scholar | PubMed]
- 6.Loos BM, El-Khatib H, Hegenscheid K, Heller M, Adam G. Radiologic evaluation and surgical management of sternal fractures. Eur Radiol 2002;12:1298-304. [Google Scholar | PubMed]
- 7.Mayberry JC, Ham LB, Schipper PH, Ellis TJ, Mullins RJ. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J Trauma 2009;66:875-9. [Google Scholar | PubMed]
- 8.Severson EP, Thompson CA, Resig SG, Swiontkowski MF. Transverse sternal nonunion, repair and revision: A case report and review of the literature. J Trauma 2009;66:1485-8. [Google Scholar | PubMed]
- 9.Bottlang M, Helzel I, Long W, Fitzpatrick D, Madey S. Less-invasive stabilization of rib fractures by intramedullary fixation: A biomechanical evaluation. J Trauma 2010;68:1218-24. [Google Scholar | PubMed]
- 10.El-Akkawi AI, Kanth N, Knight SL, El-Masry Y. Surgical stabilization of traumatic sternal fractures: A review of literature. Eur J Trauma Emerg Surg 2011;37:227-32. [Google Scholar | PubMed]