The rare possibility of ipsilateral hip and knee dislocation, the modality of approach in such a scenario, and the importance of an assisted rehabilitation protocol to give the best outcome.
Dr. K Tarun Prashanth, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai - 600116, Tamil Nadu, India. E-mail: tarun10007@gmail.com
Introduction: Simultaneous ipsilateral hip and knee dislocations are extremely rare, especially when associated with fractures, and present significant challenges in diagnosis and management. These injuries, often resulting from high-velocity trauma, require prompt intervention to tackle the complications and achieve a good outcome.
Case Report: We present the case of a 28-year-old male who sustained an ipsilateral hip fracture dislocation and knee dislocation following a high-velocity road traffic accident. Initial clinical examination revealed significant deformities in both joints, and imaging confirmed posterior dislocation of the hip with an acetabular wall fracture and a posterior knee dislocation with an inferior pole patella fracture. Emergency closed reduction was performed within hours of the incident, followed by detailed imaging studies including computed tomography and magnetic resonance imaging. Surgical management involved open reduction and internal fixation of the femoral head and posterior acetabular wall reconstruction. Post-operative rehabilitation focused on joint mobility and strength, and the patient achieved full weight-bearing and near-complete range of motion by 18 months.
Discussion: The rare occurrence of simultaneous hip and knee dislocations necessitates careful management, with emphasis on early reduction and neurovascular assessment. This case highlights the challenges of managing such injuries, including the coordination of hip and knee reduction techniques and post-operative rehabilitation tailored to the patient’s needs. Despite the complexity, timely intervention and individualized care can lead to favorable outcomes, even in severe trauma.
Conclusion: Ipsilateral hip and knee dislocations require urgent diagnosis and a multidisciplinary approach for optimal management. Prompt closed reduction, appropriate surgical intervention, and a tailored rehabilitation protocol are key to achieving good functional outcomes in these rare and complex injuries.
Keywords: Dislocation, ipsilateral hip, knee dislocation.
Hip or knee dislocations, most commonly associated with high-velocity injuries, are common when occurring individually. Simultaneous ipsilateral hip and knee dislocation is an exceedingly rare presentation requiring emergency intervention [1-13]. Such cases associated with hip and knee fractures are even rare and very few cases have been reported worldwide [1,10,13]. The outcome of such cases can vary from an excellent recovery with nil neurovascular deficit to amputations [7,14]. Treatment of these injuries poses a great challenge to the surgeons owing to its rarity, unique presentation, and lack of treatment protocol. Prompt diagnosis and decision making are warranted to reduce the morbidity and provide a good clinical outcome. We present a case of a 28-year-old gentleman with ipsilateral hip fracture dislocation and knee dislocation and discuss the management protocol adapted.
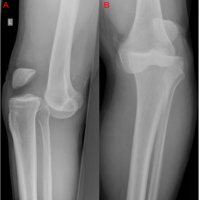
A 28-year-old gentleman with no known comorbidities was involved in a high-velocity road traffic accident (2-wheeler vs. 2-wheeler). The patient presented to the emergency department of our hospital 2 h after the time of incident with painful deformities over his left hip and left knee. There was no history of head injury, ear, nose, and throat bleed, abdominal pain, breathing difficulty. On examination, he was hemodynamically stable with no evidence of intracranial hemorrhage, intra-abdominal bleeding, or hemopneumothorax. His left hip was flexed, adducted, and internally rotated and left knee was in 30°–40° flexion with posterior sag, restricted hip and knee movements. Dorsalis pedis and posterior tibial pulses were well palpable and equal to that of the contralateral limb. There were no signs of neurological deficits with the presence of ankle dorsiflexion and plantar flexion without any sensory loss. As a first line of investigation, X-ray of left hip and X-ray of the knee joint were done which revealed posterior dislocation of the left hip with posterior acetabular wall fracture (Fig. 1) and posterior dislocation of the knee with inferior pole of patella fracture (Fig. 2).
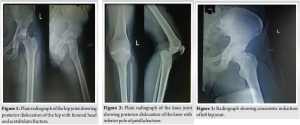
The patient was shifted to the operation theater within 5 h from the time of the incident and emergency hip and knee closed reduction was performed. Under IV sedation, the patient in supine position, with the primary surgeon on the same side as the injured limb, the femoral condyle along the girth of the thigh, was stabilized by the assistant and a anteriorly directed force was used to deliver the proximal tibia by closed reduction into the joint, good articular congruity was achieved and there was no evidence of varus or valgus instability of the knee on assessment. The hip joint was then reduced by giving longitudinal traction along the femur, with hip and knee in 90/90 flexion and providing gentle internal and external rotation while an assistant stabilized the knee joint. Once the hip and knee joints were reduced, knee joint was stabilized in extension using a long knee brace and post-reduction X-rays of the hip and knee were performed (Fig. 3 and 4).
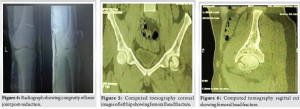
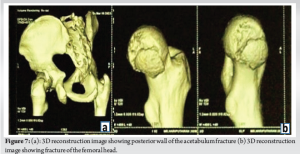
Computed tomography (CT) of the pelvis with hip joints was performed along with CT angiography of the left lower limb which showed intra-articular fracture of the femoral head with avulsion fracture of the posterior wall of the acetabulum (PIPKIN TYPE-IV) (Fig. 5-7). CT-angiography of the lower limb revealed no vascular injuries. Magnetic resonance imaging of the left knee joint was performed showed complete tear of the posterior cruciate ligament (PCL), Grade II tear of the posterior horn of the medial meniscus, and inferior pole of the patella fracture.
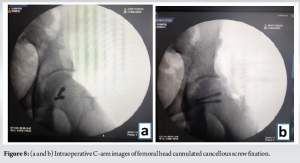
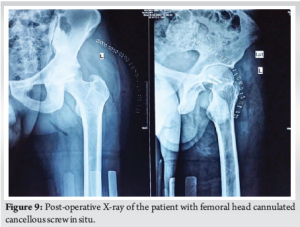
On 10th day post-trauma, the patient positioned in right lateral position, using Kocher-Langenbeck approach, the patient underwent left head of femur open reduction internal fixation with 2 headless compression screws, and posterior acetabular wall fracture was reconstructed using Ethibond. The choice of a posterior approach was chosen in view of initial presentation following injury being posterior, the tear of the capsular and muscular structures allows direct access to the joint and following fixation, and the torn structures can be visualized and repaired. The only limitation of achieving absolute reduction is to deliver the remaining portion of the infrafoveal femoral head to the rest of the femoral head and proximal femur, thereby gaining the necessary trajectory for screw fixation. This was achieved by dislocating the femur and accessing the infrafoveal fragment through the inferior portion of the joint and then reducing the fracture with a reduction clamp and provisional fixation was done with two 2 mm Kirschner wires, following which headless compression screw was inserted and maximum compression was achieved in-between the fragments (Fig. 8). The hip was relocated, the capsule was repaired with Ethibond, and the torn external rotators were reconstructed. Using image intensifier, it was confirmed that the joint was congruous; clinical assessment under anesthesia was performed and there was no impedance or blockade throughout the complete range of movements in all planes. To reduce the morbidity and the risk of arthrofibrosis of the knee, PCL reconstruction was planned for at a later date. Post-operative X-ray was done on post-operative day 2 which showed excellent reduction and articular congruity (Fig. 9).
Postoperatively, the knee was immobilized using a knee brace for the first 3 weeks following surgery. Left hip abduction and adduction exercises were initiated from post-operative day 1. Left hip passive flexion and extension exercises were started in the lateral position from 3-week onward. Active hip flexion and extension exercises were performed from 6 weeks postoperatively. At 2-month follow-up, the patient was mobilizing full weight bearing using walker support, and the patient developed knee stiffness with an ROM of 0–30°. Rigorous rehabilitation protocol was initiated. The patient was started on continuous passive mobilization exercises to the knee and wax bath mobilization and patellar gliding. He was also encouraged to perform quadriceps and hamstring strengthening, straight leg raising exercises.
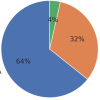
At 3-month follow-up postoperatively, he was able to mobilize full weight bearing without support and achieved a knee range of motion of 0–120°. At 18-month follow-up, the patient presented to the outpatient department with minimal hip and knee discomfort. He was able to carry out his daily activities without hindrance and able to sit on the floor crossed leg (Fig. 10). He was able to achieve a hip abduction 0–40°, hip extension 0–20°, hip flexion of 0–80°, and knee flexion 0–130° (Fig. 10). He had no knee instability and anterior drawer, posterior drawer, varus stress, valgus stress were negative. Conservative management for the left knee was decided after considering the patient’s current clinical condition and stability of the knee. Radiography of the hip and knee revealed concentric reduction of hip and knee without any evidence of avascular necrosis of the femoral head.

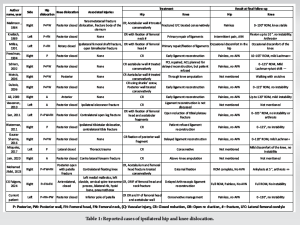
Isolated hip and knee dislocations are common in a high-velocity injury. Concomitant ipsilateral hip and knee dislocations are very rare and only 17 such cases including our case have been reported [1-12,14-17]. These kinds of injuries have extremely high chances of neurovascular compromise. Details of all the reported cases and their outcomes have been reported in Table 1.
Nature of injury
Posterior dislocation of the hip with or without associated knee injuries is common in a setting of high-velocity trauma. However, knee dislocation associated with hip dislocation is extremely rare. Hunter in 1969 reviewed 58 cases of hip dislocation among which 24 cases had associated knee injuries without dislocation [18]. Gillespie in 1975 reviewed 135 such similar injuries and noted 35 associated knee injuries with 10 ligamentous injury and no dislocations [19]. 17 cases of concomitant hip and knee dislocations were reported and 15 of which were associated with road traffic accident. Among the reported cases, 14 cases had posterior dislocation of hip [1-7,10-12,15-17] and 3 patients had anterior dislocation [8,9,14]. Among the 14 posterior hip dislocations, 11 were associated with posterior dislocation of the knee and only 2 had associated patella fracture and femoral head fracture including ours [16]. Nature and pattern of these injuries suggest that almost all such injuries happen due to extreme axial load over the knee and leg, directed along the femur to the hip joint, first dislocating the hip and then the knee if the force is persistent.
Neurovascular injury
The most common yet most critical complication associated with knee dislocation is the popliteal artery injury. 16.9% (12/71) of knee dislocations reported by McDonough and Wojtys were associated with injuries to the popliteal artery [20]. Within this group, up to 66.7% (8/12) had normal pulses on physical examination. This signifies the importance of neurovascular examination in these injuries and the requirement of CT angiography. Among the cases reported, 4 patients had vascular compromise, 3 resulting in popliteal artery injury [7,11,14]. One patient with popliteal artery injury underwent successful repair [11], while other two eventually required amputation. 17.6% incidence of vascular injury was observed among the reported cases, this tells us the importance of evaluation for vascular injuries in ipsilateral hip and knee dislocation and also provides an idea for the amount of force required to cause such damage. Four patients had neurological compromise, peroneal nerve being the most affected and all recovered eventually with conservative management [2,6,12,16]. Cornwall reported a 10% incidence of nerve injury following traumatic hip dislocations [21]. Harber CD, Plancher reported 10–40% incidence of nerve injury in knee dislocations [22,23]. It is recommended not to explore the nerve following hip dislocations, whereas if the nerve injury is following knee dislocation, the need for surgery is controversial.
Management of hip and knee dislocation
It is recommended to attempt closed reduction of the hip at the earliest to reduce the chances of avascular necrosis, neurovascular compromise, hip arthrosis [13]. There are multiple recommended techniques for hip reduction but when associated with knee dislocation, hip reduction becomes a challenge. Usually, hip reduction is done with knee and hip in 90/90 flexion and traction applied using the proximal leg as lever, which cannot be done in this setting due to knee dislocation. Freedman et al. performed the reduction with manual traction over the thigh [3]. Dubois et al. used Schanz pin over the femoral condyle and proximal femur to reduce the hip [6]. Jlidi et al. used 2 Steinmann pins over the femoral condyle to assist in hip reduction [16]. In our case, manual traction over the thigh and gentle manipulation helped in hip reduction. With respect to knee dislocation associated with multi-ligamentous injury, there remains a controversy between early and delayed surgical intervention. Few studies recommend early intervention to improve functional and clinical outcomes [22,24,25]. However, recent studies weigh on delayed surgery to avoid residual knee instability, stiffness, and flexion deformities associated with early surgery [26]. Considering the patient’s clinical condition, conservative management for the knee injury was adapted in our scenario and was able to reach a fully functioning knee without instability.
Rehabilitation
Simultaneous hip and knee fracture dislocation poses a great challenge to the surgeon in terms of prompt diagnosis and treatment. Extensive post-operative rehabilitation is crucial for achieving the desired clinical outcome. There is no available rehabilitation algorithm for such cases and the rehabilitation protocol must be exclusively tailored for each patient, considering the overall clinical condition of the patient and associated injuries.
Ipsilateral hip and knee dislocation presents a formidable challenge, demanding swift diagnosis and precise management to ensure good clinical outcome. This rare injury highlights the need for patient-centered approach. Through timely intervention and tailored rehabilitation, even the most complex injuries can achieve remarkable recoveries, redefining the limits of trauma care.
Ipsilateral traumatic pipkin fracture dislocation and knee dislocation are a very rare presentation that requires high level of clinical suspicion for prompt diagnosis and early intervention. It is important to rule out other associated injuries in such high-velocity trauma. Early reduction of the dislocated joints and timely surgical intervention if warranted followed by patient-centric rehabilitation is vital for good clinical outcome.
References
- 1.Malimson PD. Triple fracture-dislocation of the lower limb. Injury 1984;16:11-2. [Google Scholar | PubMed]
- 2.Kreibich DN, Moran CG, Pinder IM. Ipsilateral hip and knee dislocation. A case report. Acta Orthop Scand 1990;61:90-1. [Google Scholar | PubMed]
- 3.Freedman DM, Freedman EL, Shapiro MS. Ipsilateral hip and knee dislocation. J Orthop Trauma 1994;8:177-80. [Google Scholar | PubMed]
- 4.Millea TP, Romanelli RR, Segal LS, Lynch CJ. Ipsilateral fracture-dislocation of the hip, knee, and ankle: Case report. J Trauma 1991;31:416-9. [Google Scholar | PubMed]
- 5.Schierz A., Hotz T., Käch K. Ipsilateral knee and hip joint dislocation. Unfallchirurg. Jul 2002;105(7):660–663. doi: 10.1007/s00113-001-0398-8. [Google Scholar | PubMed | CrossRef]
- 6.DuBois B, Montgomery WH Jr., Dunbar RP, Chapman J. Simultaneous ipsilateral posterior knee and hip dislocations: Case report, including a technique for closed reduction of the hip. J Orthop Trauma 2006;20:216-9. [Google Scholar | PubMed]
- 7.Motsis EK, Pakos EE, Zaharis K, Korompilias AV, Xenakis TA. Concomitant ipsilateral traumatic dislocation of the hip and knee following high-energy trauma: A case report. J Orthop Surg (Hong Kong) 2006;14:322-4. [Google Scholar | PubMed]
- 8.Ali C, Malkus T, Podskubka A. Ipsilateral traumatic dislocation of hip and knee joints. Case report. Acta Chir Orthop Traumatol Cech 2009;76:329-34. [Google Scholar | PubMed]
- 9.Vaseenon T, Wongtriratanachai P, Laohapoonrungsee A. Ipsilateral anterior hip dislocation and posterior knee subluxation: A case report. J Med Assoc Thai 2010;93:128-31. [Google Scholar | PubMed]
- 10.Sen RK, Tripathy SK, Krishnan V, Goyal T, Jagadeesh V. Ipsilateral fracture dislocations of the hip and knee joints with contralateral open fracture of the leg: A rare case and its management principles. Chin J Traumatol 2011;14:183-7. [Google Scholar | PubMed]
- 11.Waterman BR, Banerjee R. Management of simultaneous ipsilateral dislocation of hip, knee, and ankle. Am J Orthop (Belle Mead NJ) 2011;40:301-4. [Google Scholar | PubMed]
- 12.Sharma G, Chahar D, Sreenivasan R, Verma N, Pankaj A. Ipsilateral hip and knee dislocation: Case report and review of literature. J Clin Orthop Trauma 2016;7:115-21. [Google Scholar | PubMed]
- 13.Tsai IT, Hsu CJ, Fong YC, Hsu HC, Chang CH, Tsai CH. Simultaneous ipsilateral hip and knee fracture-dislocations. Formosan J Musculoskeletal Disord. 2011;2(2):66–70. [Google Scholar | PubMed]
- 14.Jain M, Sathia S, Mahapatra RP, Swaroop S, Doki SK. Triple blow injury to a limb: Ipsilateral hip and knee dislocation with vascular occlusion. J Emerg Trauma Shock 2020;13:309-11. [Google Scholar | PubMed]
- 15.Miquelez AA, Familiari F, Arbeloa L, Azzarelli AD. Simultaneous ipsilateral dislocation of the hip and the knee: A case report. JBJS Case Connect 2017;7:e85. [Google Scholar | PubMed]
- 16.Jlidi M, Bouaicha W, Mallek K, Gharbi MH, Jaziri S, Daas S. A rare concomitant ipsilateral hip and knee dislocations: A case report and review of the literature. SAGE Open Med Case Rep. 2024 Feb 25;12:2050313X241233199. doi: 10.1177/2050313X241233199. PMID: 38410690; PMCID: PMC10896048. [Google Scholar | PubMed | CrossRef]
- 17.Falgons CG, Warner SJ. Simultaneous ipsilateral hip and knee dislocation: Management and outcome - a case report. Trauma Case Rep 2024;53:101079. [Google Scholar | PubMed]
- 18.Hunter GA. Posterior dislocation and fracture-dislocation of the hip. A review of fifty-seven patients. J Bone Joint Surg Br 1969;51:38-44. [Google Scholar | PubMed]
- 19.Gillespie WJ. The incidence and pattern of knee injury associated with dislocation of the hip. J Bone Joint Surg Br 1975;57:376-8. [Google Scholar | PubMed]
- 20.McDonough EB Jr., Wojtys EM. Multiligamentous injuries of the knee and associated vascular injuries. Am J Sports Med 2009;37:156-9. [Google Scholar | PubMed]
- 21.Cornwall R, Radomisli TE. Nerve injury in traumatic dislocation of the hip. Clin Orthop Relat Res 2000;377:84-91. [Google Scholar | PubMed]
- 22.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am 2004;86:262-73. [Google Scholar | PubMed]
- 23.Plancher KD, Siliski J. Long-term functional results and complications in patients with knee dislocations. J Knee Surg 2008;21:261-8. [Google Scholar | PubMed]
- 24.Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med 1997;25:769-78. [Google Scholar | PubMed]
- 25.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med 1995;23:580-7. [Google Scholar | PubMed]
- 26.Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: A systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am 2009;91:2946-57. [Google Scholar | PubMed]