• To assess the outcome using radiological parameters and Constant-Murley score • To incorporate the double endobutton technique in the management of lateral end of clavicle fractures
Dr. Prem Kumar Kothimbakkam, Department of Orthopaedics and Traumatology, Chettinad Hospital and Research Institute, Kelambakkam, Tamil Nadu, India. E-mail: drpremkumar.kvk@gmail.com
Introduction: Displaced lateral end clavicle fractures are challenging injuries with a high risk of non-union and functional impairment when treated conservatively. Open reduction and endobutton fixation is a novel surgical technique that aims to provide stable fixation while preserving shoulder biomechanics, potentially improving functional and radiological outcomes compared to traditional methods.
Materials and Methods: This prospective study included 20 male patients (mean age: 35.2 years, range: 18–56) with displaced lateral clavicle fractures (Neer type IIB and type V). All patients underwent open reduction and fixation using a twin coracoclavicular endobutton construct. Functional outcomes were assessed using the Constant-Murley scores at 6 weeks, 3 months, 6 months, and 12 months. Radiological outcomes, including fracture union and residual displacement, were evaluated with serial radiographs. Complications, return to activity, and patient satisfaction were also analyzed.
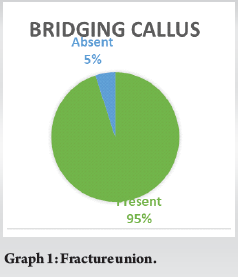
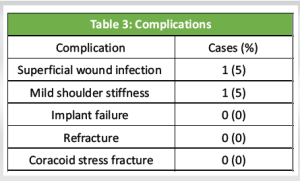
Results: The mean Constant-Murley score improved significantly from 60.3 ± 8.1 at 6 weeks to 87.4 ± 4.8 at 6 months (P < 0.01), stabilizing at 88.1 ± 5.2 by 12 months. Union was achieved in 95% of cases by 6 months, with a mean residual displacement of 1.1 mm. Complications were minimal (5% each for superficial infection and mild stiffness). All patients returned to sedentary work within 8 weeks and full manual labor or sports by 6 months. Patient satisfaction was high, with 90% reporting being “highly satisfied” at the end of 1 year.
Conclusion: Open reduction and endobutton fixation for displaced lateral clavicle fractures provide excellent functional recovery, high union rates, and minimal complications. This technique offers a reliable alternative to traditional fixation methods, particularly for young and active individuals. Further comparative studies and long-term follow-up are warranted to establish its role as the gold standard.
Keywords: Lateral end clavicle fractures, endobutton fixation, functional outcomes, radiological outcomes, fracture union.
Clavicle fractures are a common orthopedic injury, accounting for 2–4% of all fractures in adults, with the lateral end involved in approximately 15–30% of cases. Among these, displaced fractures of the lateral clavicle pose unique challenges due to its biomechanical instability and a higher risk of non-union when managed non-operatively. Non-union can lead to persistent pain, restricted shoulder mobility, and reduced upper limb strength, which significantly impact daily activities and hinder return to work or sports. Consequently, surgical management is often preferred, especially for younger and more active patients with higher functional demands [1,2]. Displaced fractures of the lateral clavicle are often unstable due to disruption of the coracoclavicular ligament complex. These injuries are commonly classified using systems such as the Neer and Edinburgh classifications, which account for ligament involvement and fracture displacement [1,2]. Traditional surgical techniques, such as coracoclavicular screws and hook-plate fixation, are widely used to treat displaced lateral clavicle fractures. These methods are effective in achieving fracture union but are associated with complications, including implant loosening, infections, and acromioclavicular joint stiffness. Furthermore, the rigidity of these implants often necessitates a secondary procedure for their removal, adding to patient morbidity and health-care costs [3,4]. A novel technique involving open reduction and twin coracoclavicular endobutton fixation offers a potential solution. This approach provides stable fixation while preserving the natural biomechanics of the acromioclavicular joint, potentially reducing complications such as joint stiffness and eliminating the need for routine implant removal. Preliminary studies indicate promising outcomes with this technique, including high union rates and satisfactory functional recovery, but further research is necessary to validate its efficacy and long-term benefits [5]. Surgical options such as hook plates and coracoclavicular screws offer rigid fixation but restrict natural shoulder movement and are associated with complications, including hardware failure and soft tissue irritation. In addition, these methods frequently require implant removal, leading to delays in recovery and increased health-care utilization [3,4]. The twin coracoclavicular endobutton technique represents a less rigid, innovative alternative. By replicating the function of the coracoclavicular ligaments and maintaining fracture reduction, this technique supports natural biomechanics while promoting union. Early clinical evidence suggests favorable functional and radiological outcomes with this method; however, data remain limited, especially in terms of comparative studies with established techniques [5]. This study aims to evaluate the functional and radiological outcomes of displaced lateral clavicle fractures treated with open reduction and endobutton fixation. The findings are expected to enhance understanding of this technique’s effectiveness and inform evidence-based management of these challenging injuries.
Objective
To study the functional and radiological outcomes in lateral end clavicle fracture managed with the double endobutton technique.
Study design
This prospective observational study was conducted to evaluate the functional and radiological outcomes of displaced lateral end clavicle fractures treated with open reduction and endobutton fixation. The study adhered to the ethical guidelines of the institute, and the institutional ethics committee approval was obtained before initiation. Informed consent was obtained from all participants.
Patient selection
A total of 20 patients with displaced lateral clavicle fractures were included in the study. Participants were recruited from the orthopedic trauma department of a tertiary care center between January 2020 and November 2023.
Inclusion criteria
- Age between 18 and 60 years
- Acute displaced lateral end clavicle fractures (Neer type IIB or type V, Edinburgh type 3B1 or 3B2) confirmed through radiography
- Injury occurring within 3 weeks of presentation
- Medically fit for surgery and capable of post-operative follow-up.
Exclusion criteria
- Patients with open fractures or associated neurovascular injuries
- Concomitant fractures involving the scapula or proximal humerus
- Pathological fractures or fractures resulting from malignancy
- Previous history of shoulder surgery on the affected side
- Inability to comply with follow-up or physiotherapy protocols.
Pre-operative assessment
Upon presentation, all patients underwent a detailed clinical examination and imaging studies, including anteroposterior and Velpeau radiographs. The fractures were classified according to the Neer and Edinburgh systems. Baseline functional status was assessed using the Constant-Murley score. Comorbidities and demographic data were recorded.
Surgical technique
All surgeries were performed under general anesthesia by a single senior orthopedic surgeon. The patients were positioned in a beach-chair configuration, with the affected shoulder exposed under sterile conditions.
- Incision and exposure: A 6-cm vertical incision, centered over the coracoid process, was made. The deltotrapezial fascia was incised perpendicular to the incision, and the fracture site was exposed by careful dissection.
- Bone tunnel creation: Two bone tunnels were drilled using a 4.5-mm cannulated drill bit. The first tunnel was made in the clavicle approximately 15-mm medial to the fracture site. The second tunnel was drilled centrally through the coracoid process under direct visualization, ensuring proper alignment and avoiding eccentric placement.
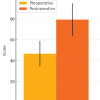
- Endobutton placement: A twin endobutton construct, consisting of two titanium buttons loaded with braided sutures, was used. The lower button was passed through the tunnels and toggled on the inferior surface of the coracoid. The fracture was reduced manually under direct vision, and the sutures were tensioned to achieve optimal alignment (Fig. 1 and 2).
4. Fixation and closure: Once the reduction was confirmed radiographically using fluoroscopy, the sutures were tied securely over the proximal button. The incision was closed in layers, and the arm was placed in a sling for immobilization.
Post-operative protocol
Postoperatively, patients were advised to use a broad arm sling for 4 weeks. Physiotherapy commenced after 4 weeks, focusing on gradual range-of-motion exercises followed by strengthening exercises. Full weight-bearing activities were allowed after radiographic evidence of fracture union.
Outcome measures
Patients were evaluated at 1, 6, and 12 weeks and at 6 and 12 months postoperatively. Functional outcomes were assessed using the Constant-Murley score. Radiological outcomes were evaluated using standard anteroposterior radiographs, measuring residual displacement and signs of fracture union. Union was defined as the absence of pain with evidence of bridging callus on radiographs.
Statistical analysis
Descriptive statistics were used to summarize baseline characteristics and outcomes. Continuous variables, such as Constant-Murley score, were expressed as means and standard deviations. Paired t-tests were used to compare functional scores at different time points. Statistical significance was set at P < 0.05. All analyses were done using Statistical Packages for the Social Sciences version 26.0.
A total of 20 patients were included in the study, with a mean age of 35.2 years (range 18–56 years). All patients were male, and the fractures were primarily sustained during sports activities (n = 14, 70%), followed by falls at home (n = 4, 20%) and road traffic accidents (n = 2, 10%). The mean time from injury to surgery was 7.4 days (range 2–14 days). The fractures were classified as Neer type IIB (n = 12, 60%) and type V (n = 8, 40%), and all cases met the criteria for complete displacement without residual cortical contact (Table 1).

Operative details
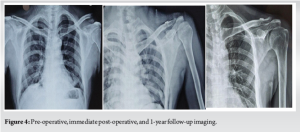
The mean duration of surgery was 45 min (range 30–70 min), and the mean intraoperative blood loss was 90 mL (range 50–150 mL). Fluoroscopic imaging confirmed satisfactory reduction in all cases, with a mean residual displacement of 1.2 mm (range 0–3 mm) postoperatively. No intraoperative complications, such as neurovascular injury or technical failure, were reported.
Functional outcomes
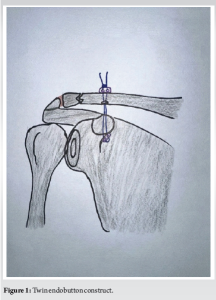
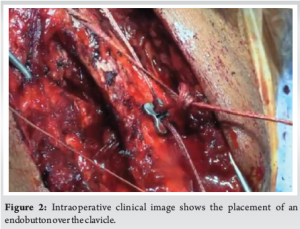
At 6 weeks, the mean Constant score was 60.3 ± 8.1, indicating moderate functional recovery. At 3 months, the score improved significantly to 81.2 ± 6.5 (P < 0.01 compared to 6 weeks). By 6 months, the mean score reached 87.4 ± 4.8, with no further significant improvement at the 1-year follow-up (mean score 88.1 ± 5.2, P = 0.18 compared to 6 months) (Table 2 and Fig. 3).


Radiological outcomes
All fractures achieved union by the 6-month follow-up except one, which developed an asymptomatic fibrous union. Radiographs showed evidence of bridging callus in 95% of cases by 3 months. At the 12-month follow-up, there was no loss of reduction or implant failure observed. Residual displacement at the union was minimal, with a mean of 1.1 mm (range 0–2.5 mm) (Graph 1 and Fig. 4). Early post-operative complications were minimal: One patient (5%) experienced superficial wound infection, which resolved with oral antibiotics. One patient (5%) developed mild shoulder stiffness, characterized by a 15° loss of external rotation, which resolved after 8 weeks of physiotherapy. No late complications, such as implant failure, refracture, or coracoid stress fractures, were observed. There was no incidence of symptomatic hardware irritation, and no patient required secondary surgery for implant removal (Table 3).
Return to work and sports
All patients returned to sedentary work within 8 weeks of surgery. Patients engaged in manual labor (n = 6) resumed full duties by 6 months. Of the 14 patients involved in sports, 12 (85.7%) returned to their pre-injury activity level by 6 months, and the remaining two downgraded to non-contact sports due to personal preference.
Patient satisfaction
At the 1-year follow-up, 18 patients (90%) reported being “highly satisfied” with their surgical outcomes, whereas two patients (10%) were “satisfied” due to minor stiffness during overhead activities.
This study highlights the functional and radiological success of open reduction and endobutton fixation for displaced lateral end clavicle fractures, demonstrating high union rates, excellent functional recovery, and low complication rates. These findings align with the growing preference for less rigid, ligament-mimicking fixation methods that preserve shoulder biomechanics. The study included patients with a mean age of 35.2 years, predominantly young males involved in high-energy activities such as sports, reflecting the typical demographic for these injuries [1,2]. The classification of fractures as Neer type IIB and type V underlines the instability and complexity of the injuries managed, with all cases involving complete displacement and loss of cortical contact, requiring surgical intervention [3]. The surgical metrics, including a mean operative time of 45 min and blood loss of 90 mL, reflect an efficient and reproducible procedure. The absence of intraoperative complications, such as neurovascular injury or implant malposition, suggests a favorable learning curve for surgeons familiar with the technique. The mean residual displacement of 1.2 mm postoperatively compares favorably with other techniques, such as hook plates, which often report higher displacement due to rigid plate fixation limiting fracture compression [6]. The significant improvements in Constant-Murley scores reflect rapid functional recovery. The mean Constant score reached 87.4 by 6 months and remained stable at 1 year, comparable to outcomes reported with anatomical locking plates and suture anchors [5,7]. The early gains in shoulder mobility suggest that the endobutton construct successfully avoids the stiffness associated with rigid constructs such as hook plates [6,8]. The 95% fracture union rate at 6 months and minimal residual displacement at union align with or exceed outcomes reported in comparative studies. For instance, Flinkkilä et al. reported a union rate of 85% using hook plates, with higher rates of symptomatic hardware irritation requiring implant removal [3]. Similarly, Ballmer and Gerber observed higher rates of delayed union with coracoclavicular screws, attributed to their inability to maintain physiological ligament function during healing [7]. The low complication rate observed in this study – 5% each for superficial wound infection and transient shoulder stiffness – compares favorably with other fixation methods. Hook plates have been associated with complication rates as high as 30–40%, including hardware irritation, plate impingement, and implant failure [6,7]. Suture anchor techniques, while less invasive, report higher incidences of suture loosening and implant failure, particularly in high-demand patients [9,10]. The absence of symptomatic hardware irritation or need for implant removal in this cohort underscores the endobutton construct’s advantage in minimizing patient morbidity. The majority of patients returned to sedentary work within 8 weeks and to full manual labor or sports activities by 6 months. This is consistent with studies of TightRope and similar suture-based techniques, which emphasize early return to function due to their biomechanical flexibility [9,11]. By contrast, patients treated with hook plates or coracoclavicular screws often experience delayed return to activity due to stiffness and hardware-related discomfort [6,12]. The high satisfaction rates (90% “highly satisfied”) are consistent with studies of minimally invasive techniques such as arthroscopic suture fixation or coracoclavicular loop augmentation [9,13]. The remaining 10% who reported minor stiffness with overhead activities highlight the need for tailored physiotherapy protocols to address residual functional limitations. Comparative studies offer important insights into the advantages of the endobutton technique over traditional methods:
Hook plates
Flinkkilä et al. reported a 38% complication rate and a need for routine implant removal in 63% of cases [3]. In contrast, the endobutton construct eliminates the need for routine implant removal, reducing secondary surgery rates.
Coracoclavicular screws
Ballmer and Gerber reported hardware failure and the necessity of implant removal in 40% of cases [7]. The rigid fixation of screws often restricts shoulder mobility, while the flexible endobutton construct allows dynamic joint motion.
TightRope technique
Salzmann et al. observed union rates of 90% with TightRope, though complications such as suture loosening and coracoid fractures were noted in 10% of cases [9]. The endobutton construct appears to mitigate such risks by providing a more robust fixation.
Suture anchor fixation
Shin et al. reported union rates of 88% with dual suture anchors but observed recurrent displacement in 12% of cases [10]. The biomechanical superiority of the endobutton in maintaining stable reduction likely contributes to its higher success rates. The study is limited by its small sample size and lack of a control group using alternative fixation methods. Long-term follow-up is needed to assess the incidence of late complications, such as acromioclavicular arthritis or implant-related stress fractures. In addition, a randomized controlled trial comparing the endobutton construct with other techniques, such as hook plates or TightRope, would provide more definitive evidence of its relative benefits.
The results of this study affirm that open reduction and endobutton fixation for displaced lateral clavicle fractures offers excellent functional and radiological outcomes with minimal complications. When compared to traditional techniques, the endobutton construct demonstrates clear advantages in preserving joint biomechanics, reducing hardware-related morbidity, and expediting functional recovery. Further studies with larger cohorts and direct comparisons are warranted to establish this technique as the gold standard for managing these challenging fractures.
A minimally invasive procedure with almost nil complications.
References
- 1.Neer CS 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res 1968;58:43-50. [Google Scholar | PubMed]
- 2.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998;80:476-84. [Google Scholar | PubMed]
- 3.Flinkkilä T, Ristiniemi J, Lakovaara M, Hyvönen P, Leppilahti J. Hook-plate fixation of unstable lateral clavicle fractures: A report on 63 patients. Acta Orthop 2006;77:644-9. [Google Scholar | PubMed]
- 4.Fraser-Moodie JA, Shortt NL, Robinson CM. Injuries to the acromioclavicular joint. J Bone Joint Surg Br 2008;90:697-707. [Google Scholar | PubMed]
- 5.Robinson CM, Akhtar MA, Jenkins PJ, Sharpe T, Ray A, Olabi B. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br 2010;92:811-6. [Google Scholar | PubMed]
- 6.Mizue F, Shirai Y, Ito H. Surgical treatment of comminuted fractures of the distal clavicle using Wolter clavicular plates. J Nippon Med Sch 2000;67:32-4. [Google Scholar | PubMed]
- 7.Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br 1991;73:291-4. [Google Scholar | PubMed]
- 8.Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop 1998;22:366-8. [Google Scholar | PubMed]
- 9.Salzmann GM, Walz L, Schoettle PB, Imhoff AB. Arthroscopic anatomical reconstruction of the acromioclavicular joint. Acta Orthop Belg 2008;74:397-400. [Google Scholar | PubMed]
- 10.Shin SJ, Roh KJ, Kim JO, Sohn HS. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury 2009;40:1308-12. [Google Scholar | PubMed]
- 11.Hosseini H, Friedmann S, Tröger M, Lobenhoffer P, Agneskirchner JD. Arthroscopic reconstruction of chronic AC joint dislocations by transposition of the coracoacromial ligament augmented by the tight rope device: A technical note. Knee Surg Sports Traumatol Arthrosc 2009;17:92-7. [Google Scholar | PubMed]
- 12.Fraser-Moodie JA, Shortt NL, Robinson CM. Injuries to the acromioclavicular joint. J Bone Joint Surg Br 2008;90:697-707. [Google Scholar | PubMed]
- 13.Levy O. Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elbow Surg 2003;12:24-8. [Google Scholar | PubMed]